Abstract
Background:
In the intervening years, a few randomized clinical trials have confirmed that foam sclerotherapy is effective in managing great vein incompetence. However, no details have been published in its efficacy in comparison with conventional methods such as stab avulsion in the treatment of varicosis in small veins.Objectives:
This randomized clinical trial was conducted to compare results and outcomes of the ultrasonography-guided foam sclerotherapy and conventional stab avulsion ambulatory phlebectomy in the treatment of varicosis in small veins of the leg.Patients and Methods:
In a randomized single-blinded clinical trial, patients with varicosis in the small veins of the leg were randomly assigned for treatment with ultrasonography-guided foam sclerotherapy (n = 45) or with ambulatory phlebectomy (n = 45). Follow-up visits were done in 1 week, 1 and 6 months after operation and all patients were assessed regarding postoperative pain, need for analgesics, time to return to work, and level of satisfaction.Results:
Postoperative pain was significantly lower in foam sclerotherapy group by VAS (P = 0.003). There was a significant difference in the morbidity rate between the two techniques (13.3%. in foam sclerotherapy, 37.8% in ambulatory phlebectomy, P = 0.008). The main predictors of the pain incidence included ambulatory phlebectomy, female gender, and advanced age. Satisfaction was significantly higher in foam sclerotherapy group (P = 0.024). Also, this group had shorter time to return to work (P < 0.001).Conclusion:
Foam sclerotherapy is more preferred to ambulatory phlebectomy for treating varicosis in small veins of the leg because of its lower morbidity, less pain, more satisfaction, and shorter time to return to work.Keywords
Ultrasonography-guided Foam Sclerotherapy Stab Avulsion Ambulatory Phlebectomy Leg Small Vein Varicose
1. Background
For several years, ambulatory phlebectomy has been adopted as the “gold standard” to remove segments of varicose or reticular veins of any size (1). Ambulatory phlebectomy, stab avulsion, microphlebectomy, and microextraction are synonymous terms that define this local-anesthetic, ambulatory, outpatient technique (2, 3). Complications arising from ambulatory phlebectomy are quite rare but do exist (4-7), including anesthetic complications, skin complications (blister, keloid formation, dimpling, infection, induration, hypo- or hyperpigmentation, tattooing, and pigmentation), compression bandage complications (swelling, blisters, ischemia, skin necrosis, and contact dermatitis), vascular complications (bleeding, seroma, superficial thrombosis, deep venous thrombosis, pulmonary embolism, or telangiectasias), lymphatic complications (lymphorrhea, persisting edema, lymphocele) and neurological complications (nerve damage, temporary hypoesthesia, dysesthesia, or traumatic neuroma). Despite high efficacy of this procedure to treat lower limb vein varicose, its potential complications led to high patients’ dissatisfaction and high cost due to necessity for controlling the complications, prolonged hospitalization, and delaying return to work, and daily activities (8-11).
Advances in technology have recently led to improvements in the practice of sclerotherapy instead of stab avulsion. Moreover, the next significant advancement came in 1995 when foam created using carbon dioxide mixed with a polidocanol as a detergent sclerosant was used instead of liquid detergents leading higher cost-effectiveness and lower procedural complications (12). The increased efficacy of foam was attributable to it displacing blood from the treated vein and increasing the contact time between the sclerosant and the vein (13).
In the intervening years, several clinical series and a few randomized clinical trials have confirmed that foam sclerotherapy is effective in managing great vein incompetence. However, no details have been published in its efficacy on treatment of small veins in the lower limb especially in comparison with conventional methods such as stab avulsion.
2. Objectives
The present study aimed to compare the results and outcomes of the two common methods of ultrasonography-guided foam sclerotherapy versus conventional stab avulsion ambulatory phlebectomy in the treatment of varicosis in the small veins of the leg.
3. Patients and Methods
This was a randomized single-blinded parallel clinical trial in which patients with small vein varicosis of the leg were randomly selected for treatment with ultrasonography-guided foam sclerotherapy (group 1) or conventional stab avulsion ambulatory phlebectomy (group 2) in ratio of 1/1. Those who were previously scheduled for oral medication or invasive procedures because of vein varicosis were excluded.
The study was conducted in the vascular surgery department of Imam Khomeini hospital, Sari, Iran. On admission, baseline data including demographic characteristics, medical history, drug history, and time of the onset of disease were collected by interviewing the patients or referring recorded files.
All subjects underwent duplex scan and were scored according to clinical-etiology-anatomy-pathophysiology (CEAP) scoring system. In group 1, after mapping the treatment area, access to the vein was achieved under ultrasound guidance. Access was confirmed by return of blood, and the needle was taped to the patient’s leg. The sclerosing agent was prepared by placing one part of sodium tetradecyl sulfate (STS) in one syringe to four parts air in the other syringe. The syringes were attached to the stopcock, the stopcock was closed off, and the foam solution was created by rapidly mixing the air and chemical back and forth between the two syringes. This rapid movement was performed 20 times. After moving most of the solution to one syringe, the filled syringes were connected to the needle, and after reconfirming of intravascular positioning, a small amount of foam was injected to confirm needle placement. The amount of foam delivered was determined during injection by using ultrasound to visualize when the targeted vein was filled with foam. On completion the needle was removed, and folded 2×2-inch gauze was secured over the injection site with adhesive tape.
In group 2, skin incision was done with a No. 11 blade aligned with the lines of the Langer. The small dermal varicosities were hooked and avulsed. The vein loop was cleared of fat, doubly clamped and divided. Steri-Strip closure was used to close the incision.
Follow up visit and assessment were done 1 week, 1 month, and 6 months after operation regarding evaluation of complications including local complications, postoperative pain, and need to analgesics. Also, the patients were reassessed by duplex scan 1 month after operation to determine and compare treatment success rates between the two groups. In this regard, time to return to work and level of satisfaction were also assessed by interviewing.
Based on confidence level of 95% and power of 90% sample size was calculated as 90 subjects by a biostatistician. Randomization was done by computer software. The randomized numbers attached to envelopes contained treatment methods. At the time of the procedure, each patient was referred to the operation room with his/her envelope and at that time the surgeon found out what method he had to use.
Patients were interviewed, assigned to enroll in the study and followed up by a vascular surgeon (corresponding author). Random allocation was done by a surgery resident. Participants did not know which method was carried out on them.
Results were presented as mean ± standard deviation (SD) for quantitative variables and were summarized by absolute frequencies and percentages for categorical variables. Pain, satisfaction, and time return to work were compared using t test or non-parametric Mann-Whitney U test across the groups. Treatment success and need to analgesic was compared using chi-square test or Fisher’s exact test. The Pearson’s correlation test was applied to examine association between the study measures. For statistical analysis, statistical software SPSS version 20.0 for windows (SPSS Inc., Chicago, IL) was used. P values of 0.05 or less were considered statistically significant.
4. Results
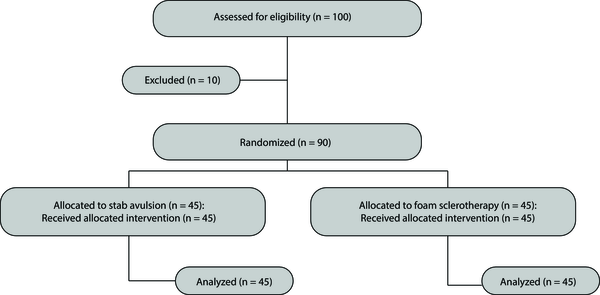
In total, 90 patients were treated with ultrasonography-guided foam sclerotherapy (n = 45) or conventional stab avulsion ambulatory phlebectomy (n = 45) (Figure 1). Patients were enrolled in the study between Feb 2013 and Feb 2014. The study ended because the sample size target was achieved.
Patients’ allocation and randomization
The two groups were similar in mean age (46.84 ± 10.12 versus 45.55 ± 11.09, P = 0.566), male to female ratio (27 to 18 versus 30 to 15, P = 0.798).
Ablation rate (6th month after surgery) was 95.5% (43/45) in foam sclerotherapy and 100% (45/45) in stab avulsion with no significant difference (P = 0.11). After one week of treatment completion, 11.1% in the foam sclerotherapy group and 37.8% in ambulatory phlebectomy group suffered from ecchymosis with a significant difference (P = 0.003). At one and six months follow-up, no complication including phlebitis, paresthesia, erythema, local infection, or hematoma was detected in either groups. The overall prevalence of deep vein thrombosis in foam sclerotherapy group and ambulatory phlebectomy group were 2.2% and 2.6%, respectively, with no difference (P = 0.301). In total, the morbidity rate in the groups treated with foam sclerotherapy and conventional stab avulsion ambulatory phlebectomy were 13.3% and 37.8%, respectively with a significant difference (P = 0.008). Regarding postoperative pain using visual analog scale (VAS), pain more than 4 (moderate and severe) was significantly less reported in patients treated with foam sclerotherapy, 15.6% versus 44.4% (P = 0.003). Also, need to analgesic use was significantly lower in the foam sclerotherapy group, 11.1% versus 37.8% (P = 0.003). In the multivariable logistic regression model, a significant difference was observed in the morbidity rate between the two techniques (Table 1). In addition, a similar regression model showed a meaningful difference in postoperative pain between the two groups (Table 2). In fact, main predictors of postoperative pain included ambulatory phlebectomy, female gender, and advanced age.
Multivariate Logistic Regression Model to Assess Difference in One-Week Complication Rate Between Ultrasound-Guided Foam Sclerotherapy and Stab Avulsion Ambulatory Phlebectomy Groups
| Item | P Value | Odds Ratio | 95% CI |
|---|---|---|---|
| Treatment method | 0.036 | 0.665 | 0.112 - 0.889 |
| Gender | 0.224 | 1.874 | 0.663 - 3.841 |
| Age | 0.779 | 0.825 | 0.524 - 1.065 |
| Length of segment | 0.541 | 0.587 | 0.225 - 1.229 |
| Side of involvement | 0.729 | 1.175 | 0.472 - 2.922 |
Multivariate Logistic Regression Model to Assess Difference in Postoperative Pain Between Ultrasound-Guided Foam Sclerotherapy and Stab Avulsion Ambulatory Phlebectomy Groups
| Item | P Value | Odds Ratio | 95% CI |
|---|---|---|---|
| Treatment method | 0.010 | 0.221 | 0.044 - 0.666 |
| Gender | 0.045 | 1.663 | 1.079 - 4.775 |
| Age | 0.036 | 1.016 | 1.002 - 1.055 |
| Length of segment | 0.260 | 0.924 | 0.805 - 1.060 |
| Side of involvement | 0.378 | 0.654 | 0.254 - 1.682 |
With respect to the level of satisfaction using VAS for satisfaction, VAS of 9 and higher was revealed in 95.6% in the foam sclerotherapy group, and 80.0% in the ambulatory phlebectomy group after 6 months, that was significantly higher in the first group (P = 0.024). Besides, time to return to work was significantly shorter in the foam sclerotherapy group compared with the ambulatory phlebectomy group (3.6 ± 1.2 days versus 13.7 ± 2.7 days, P < 0.001).
5. Discussion
In this study we compared outcomes and early results of the two techniques for treatment of varicosis in small veins of the leg including ultrasonography-guided foam sclerotherapy and stab avulsion ambulatory phlebectomy. Early studies on foam sclerotherapy in treating vein varicose could not demonstrate its efficacy probably because of its unknown technical details and applications as well as incorrect designing clinical trials. However, recently, the superiority of this procedure in comparison with surgical procedures and also ambulatory phlebectomy has been clearly identified. But most published studies have shown its efficacy on treating great saphenous vein varicose (not in small veins) without adequate following-up. In the present study, we clearly showed that foam sclerotherapy could be a good alternative for previous methods such as ambulatory phlebectomy due to its good outcomes as similar efficacy, lower postoperative pain, shorter acquired time for returning to daily activities and social workings, and overall lower morbidity rate. On the other hand, our findings were consistent with some previous trials, but most of them were studied on great saphenous vein varicosis. Subsequently, a number of authors have published clinical series based on this technique. In other study (14) have subsequently published a detailed analysis of the efficacy of foam sclerotherapy in 194 patients, reporting a good outcome in 93% of patients. In fact, this technique has become widely used in southern Europe, Australia, New Zealand, South America, and the USA (15). One randomized study of foam sclerotherapy in comparison with surgery has been published. This was a multicenter European study (16), in which 654 patients were treated to obliterate the saphenous trunks by foam sclerotherapy. After 12 months, post-treatment pain was assessed by a visual analogue scale, which showed that surgery was much more painful during the first week. Normal activities were resumed significantly quicker in the foam sclerotherapy group compared to the surgery group (2 days versus 13 days). A personal experience of the use of ultrasound-guided foam sclerotherapy for truncal saphenous incompetence between January 2002 and August 2005 has been published (17). Out of 808 patients (666 women, 142 men) who were managed by ultrasound-guided foam sclerotherapy, thrombophlebitis occurred in a small number of patients (5%). It was managed by analgesia, compression, and aspiration of thrombus. A further study showed relative efficacy of 1% and 3% for sclerosant foam (18). Frullini and Cavezzi showed foam sclerotherapy is equally applicable in complicated and uncomplicated venous disease (19). Rapid healing of ulcers following foam sclerotherapy was reported in some clinical researches and it confirmed that this treatment could probably achieve the same outcomes that result from saphenous obliteration in leg ulcer patients (20-27).
In conclusion, as foam sclerotherapy was suggested effective for treating varicosis in the great saphenous vein, in this study we showed it could be used in small varicose veins of the leg because of its higher effectiveness, lower complications, higher patient satisfaction and earlier returning to the work.
References
-
1.
Olivencia JA. Ambulatory phlebectomy turned 2400 years old. Dermatol Surg. 2004;30(5):704-8. discussion 708. [PubMed ID: 15099311]. https://doi.org/10.1111/j.1524-4725.2004.30210.x.
-
2.
Hobbs JT. Surgery or sclerotherapy for varicose veins: 10-year results of a random trial. Superficial and deep venous diseases of the lower limbs. Panminerva Medica, Turin; 1984. p. 243-8.
-
3.
Fegan WG. Injection with compression as a treatment for varicose veins. Proc R Soc Med. 1965;58(11 Part 1):874-6. [PubMed ID: 5851527].
-
4.
Olivencia JA. Complications of ambulatory phlebectomy. Review of 1000 consecutive cases. Dermatol Surg. 1997;23(1):51-4. [PubMed ID: 9107295].
-
5.
Beale RJ, Gough MJ. Treatment options for primary varicose veins--a review. Eur J Vasc Endovasc Surg. 2005;30(1):83-95. [PubMed ID: 15933989]. https://doi.org/10.1016/j.ejvs.2005.02.023.
-
6.
Sam RC, Silverman SH, Bradbury AW. Nerve injuries and varicose vein surgery. Eur J Vasc Endovasc Surg. 2004;27(2):113-20. [PubMed ID: 14718891]. https://doi.org/10.1016/j.ejvs.2003.11.007.
-
7.
Subramonia S, Lees T. Sensory abnormalities and bruising after long saphenous vein stripping: impact on short-term quality of life. J Vasc Surg. 2005;42(3):510-4. [PubMed ID: 16171598]. https://doi.org/10.1016/j.jvs.2005.05.021.
-
8.
MacKenzie RK, Paisley A, Allan PL, Lee AJ, Ruckley CV, Bradbury AW. The effect of long saphenous vein stripping on quality of life. J Vasc Surg. 2002;35(6):1197-203. [PubMed ID: 12042731].
-
9.
Mackenzie RK, Lee AJ, Paisley A, Burns P, Allan PL, Ruckley CV, et al. Patient, operative, and surgeon factors that influence the effect of superficial venous surgery on disease-specific quality of life. J Vasc Surg. 2002;36(5):896-902. [PubMed ID: 12422098].
-
10.
Sam RC, MacKenzie RK, Paisley AM, Ruckley CV, Bradbury AW. The effect of superficial venous surgery on generic health-related quality of life. Eur J Vasc Endovasc Surg. 2004;28(3):253-6. [PubMed ID: 15288627]. https://doi.org/10.1016/j.ejvs.2004.04.007.
-
11.
Wright AP, Berridge DC, Scott DJ. Return to work following varicose vein surgery: influence of type of operation, employment and social status. Eur J Vasc Endovasc Surg. 2006;31(5):553-7. [PubMed ID: 16460971]. https://doi.org/10.1016/j.ejvs.2005.05.016.
-
12.
Orbach EJ, Petretti AK. The thrombogenic property of foam of a synthetic anionic detergent (sodium tetradecyl sulfate N.N.R.). Angiology. 1950;1(3):237-43. [PubMed ID: 15425861]. https://doi.org/10.1177/000331975000100303.
-
13.
Breu FX, Guggenbichler S. European Consensus Meeting on Foam Sclerotherapy, April, 4-6, 2003, Tegernsee, Germany. Dermatol Surg. 2004;30(5):709-17. discussion 717. [PubMed ID: 15099312]. https://doi.org/10.1111/j.1524-4725.2004.30209.x.
-
14.
Shadid N, Ceulen R, Nelemans P, Dirksen C, Veraart J, Schurink GW, et al. Randomized clinical trial of ultrasound-guided foam sclerotherapy versus surgery for the incompetent great saphenous vein. Br J Surg. 2012;99(8):1062-70. [PubMed ID: 22627969]. https://doi.org/10.1002/bjs.8781.
-
15.
Liu X, Jia X, Guo W, Xiong J, Zhang H, Liu M, et al. Ultrasound-guided foam sclerotherapy of the great saphenous vein with sapheno-femoral ligation compared to standard stripping: a prospective clinical study. Int Angiol. 2011;30(4):321-6. [PubMed ID: 21747350].
-
16.
Thomasset SC, Butt Z, Liptrot S, Fairbrother BJ, Makhdoomi KR. Ultrasound guided foam sclerotherapy: factors associated with outcomes and complications. Eur J Vasc Endovasc Surg. 2010;40(3):389-92. [PubMed ID: 20547076]. https://doi.org/10.1016/j.ejvs.2010.04.007.
-
17.
Darvall KA, Bate GR, Adam DJ, Bradbury AW. Recovery after ultrasound-guided foam sclerotherapy compared with conventional surgery for varicose veins. Br J Surg. 2009;96(11):1262-7. [PubMed ID: 19847864]. https://doi.org/10.1002/bjs.6754.
-
18.
Chapman-Smith P, Browne A. Prospective five-year study of ultrasound-guided foam sclerotherapy in the treatment of great saphenous vein reflux. Phlebology. 2009;24(4):183-8. [PubMed ID: 19620701]. https://doi.org/10.1258/phleb.2009.008080.
-
19.
Frullini A, Cavezzi A. Sclerosing foam in the treatment of varicose veins and telangiectases: history and analysis of safety and complications. Dermatol Surg. 2002;28(1):11-5. [PubMed ID: 11991262].
-
20.
Breu FX, Guggenbichler S, Wollmann JC. 2nd European Consensus Meeting on Foam Sclerotherapy 2006, Tegernsee, Germany. Vasa. 2008;37 Suppl 71:1-29. [PubMed ID: 18426039].
-
21.
Wright D, Gobin JP, Bradbury AW, Coleridge-Smith P, Spoelstra H, Berridge D, et al. Varisolve® polidocanol microfoam compared with surgery or sclerotherapy in the management of varicose veins in the presence of trunk vein incompetence: European randomized controlled trial. Phlebol J Venous Dis. 2016;21(4):180-90. https://doi.org/10.1258/026835506779115807.
-
22.
Smith PC. Chronic venous disease treated by ultrasound guided foam sclerotherapy. Eur J Vasc Endovasc Surg. 2006;32(5):577-83. [PubMed ID: 16782367]. https://doi.org/10.1016/j.ejvs.2006.04.033.
-
23.
Hamel-Desnos C, Ouvry P, Benigni JP, Boitelle G, Schadeck M, Desnos P, et al. Comparison of 1% and 3% polidocanol foam in ultrasound guided sclerotherapy of the great saphenous vein: a randomised, double-blind trial with 2 year-follow-up. "The 3/1 Study". Eur J Vasc Endovasc Surg. 2007;34(6):723-9. discussion 730. [PubMed ID: 17884623]. https://doi.org/10.1016/j.ejvs.2007.07.014.
-
24.
O'Hare JL, Parkin D, Vandenbroeck CP, Earnshaw JJ. Mid term results of ultrasound guided foam sclerotherapy for complicated and uncomplicated varicose veins. Eur J Vasc Endovasc Surg. 2008;36(1):109-13. [PubMed ID: 18313336]. https://doi.org/10.1016/j.ejvs.2008.01.015.
-
25.
Hertzman PA, Owens R. Rapid healing of chronic venous ulcers following ultrasound-guided foam sclerotherapy. Phlebology. 2007;22(1):34-9. discussion 39. [PubMed ID: 18265552]. https://doi.org/10.1258/026835507779700662.
-
26.
Bergan J, Pascarella L, Mekenas L. Venous disorders: treatment with sclerosant foam. J Cardiovasc Surg (Torino). 2006;47(1):9-18. [PubMed ID: 16434941].
-
27.
Pascarella L, Bergan JJ, Mekenas LV. Severe chronic venous insufficiency treated by foamed sclerosant. Ann Vasc Surg. 2006;20(1):83-91. [PubMed ID: 16378144]. https://doi.org/10.1007/s10016-005-9381-0.