1. Background
Imperforate anus is a congenital disease with abnormal termination of the hindgut. It has a wide spectrum of muscle sphincter complex development from near-normal muscles to complete absence of the sphincter muscle. Routinely, depending on the level of the obstruction in above and below of muscle sphincter, this anomaly is categorized into two groups; high and low type (1). There are numerous factors that control fecal continence after the surgery, the most important is the diagnosis of the exact place of the sphincter muscle complex (2).
There are various surgical approaches and procedures for anus reconstruction, including the use of preoperative MRI for diagnosis of type and level of anorectal malformation (3, 4). In addition, there are some articles about the use of MRI in the detection of sphincter complex and the anus path guidance (5, 6). However, the later technique has some limitations and is not available in all pediatric surgery centers.
In imperforate anus (IA) patients, sonography is used to determine the level of disorder (low and high), which may be divided into two groups according to the distance between perineal skin surface and rectal pouch. However, there is not an exact cut off for their differentiation and there is diagnostic overlap (1). Some articles consider above 15 mm as high type and below 10 mm as low type anorectal malformations (ARM) (1), although other numbers between 5 and 25 mm are also considered as the cut off point in articles (7-9). The passage of rectum from levator ani muscle in transverse view of infra-coccygeal region is another method that can help in differentiation between high and low groups (10). Furthermore, it is also used for diagnosis of internal fistula (rectourethral and rectovaginal), which can be helpful in determining the level of the disorder (9, 10). However, in practice, these criteria have little value for operation protocols and surgical planning is mostly based on clinical criteria and intraoperative findings.
The exact localization of anal pit and muscle sphincter complex with preoperative sonography can help the surgeon to select the less invasive surgical technique and improve surgical results.
2. Objectives
The aim of this study is investigation of ultrasonic criteria of the perineal region in imperforated anus.
3. Patients and Methods
This descriptive cross-sectional study was performed at Dr. Sheikh Pediatric hospital in 2016 after being approved by the Institutional Review Board of Mashhad University of Medical Sciences, Iran.
In this study, ten patients (6 - 12 weeks age) with imperforate anus were selected after obtaining informed consent from their parents. Nine patients had previous colostomy within the first two days of life. Another patient with rectovestibular fistula did not previously go through colostomy because this patient was misdiagnosed and had little defecation from the fistula and was visited late . Patients were also evaluated for associated congenital anomalies (VACTERL-H and etc.).
The children were placed in lithotomy position and a Foley catheter was passed from the distal limb of colostomy to the rectum and the balloon was inflated and retracted backward and fixed. For better visualization of the rectal pouch, normal saline was injected through the fixed Foley catheter in the rectum. After prep & drape as the first step, transperineal sonography was performed by an experienced pediatric radiologist. Sterile gel and betadine were used for sonographic window. The ultrasound device used in this study was SonoSite Model S-Nerve with a 12 MHz linear superficial probe.
The sonographic criteria such as shortened distance of rectal pouch from the surface of skin, distance of rectal pouch from the surface of skin in anal sphincter complex pathway, the presence of internal fistula, multi-layered view of anal pit, and state of anal sphincter complex were evaluated in both sagittal and coronal planes. The distance between rectal pouch from the surface of skin in the shortest path and this distance in correlation with sphincter complex were separately measured.
The distance between the rectal pouch and the surface of the skin and the presence of internal fistula were evaluated in the sagittal sonographic plane. Retrovaginal fistula can be identified by ultrasonographic images.
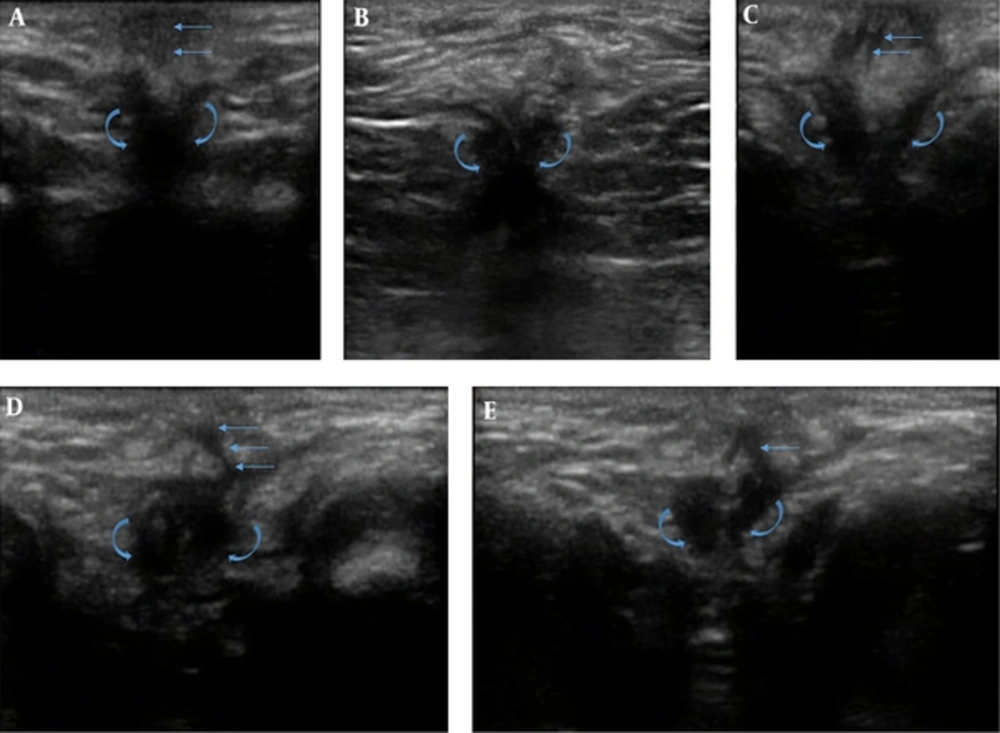
The multi-layered view of anal pit is exactly similar to gut signature, and visualized as a peripheral hypoechoic layer with two central parallel echogenic lines just below the skin (dermis). It is located vertically compared to the anal pit (Figure 1A) and is visible only in the coronal plane. Anal sphincter complex is noticeable as circular muscular tissue in the depth of the subcutaneous perineal area and is visible in the coronal plane (Figure 1B).
The findings of coronal trans-perineal ultrasonography of imperforate anus. Anal pit demarcated by straight arrows and muscle sphincter complex demarcated by curved arrow. A, Anal pit: two parallel echogenic lines perpendicular to the skin. B, The symmetric muscle sphincter complex without multi-layered view of anal pit. C, Curved path of anal pit. D, The parasagittal path of anal pit is closer to the muscle sphincter complex. E, The partial parasagittal path of anal pit and the asymmetric muscle sphincter complex.
4. Results
Table 1 shows the demographic and sonographic findings of ten imperforate anus patients who were selected for this study. Eight patients were male and the other two were female.
| Sex | Age, w | Weight, kg | Associated anomalies | Distance of rectal pouch-skin: straight | Distance of rectal pouch-skin: path | Fistula | Multi layered view of anal pit | Long of anal pit | Muscle complex thickness, mm | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | 6 | 6 | Urinary reflux | 8 | 11 | Yes | Yes | 8 | 3.5 |
| 2 | Male | 7 | 6 | Single-kidney, ASD | 18 | 22 | Yes | Yes | 6 | 2.7 |
| 3 | Male | 8 | 6 | No | 15 | 20 | Yes | Yes | 6 | 2.7 |
| 4 | Male | 6 | 5.5 | No | 17 | 21 | Yes | Yes | ||
| 5 | Male | 7 | 6 | Hydronephrosis, ASD | 14 | 22 | Yes | Yes | 7 | 2.5 |
| 6 | Male | 6 | 5.5 | No | 16 | 19 | Yes | Yes | 5 | 2.6 |
| 7 | Male | 6 | 6 | No | 18 | 21 | Yes | Yes | 7 | 2.5 |
| 8 | Male | 8 | 5 | Down syndrome, Cardiac and renal problems | 12 | 20 | No | Yes | 5 | 2.5 |
| 9 | Female | 12 | - | Rectovestibular fistula | 9 | 15 | Yes | No | - | 3.6 |
| 10 | Female | 5 | 7 | Cloacal anomaly, Hydronephrosis | 20 | 23 | Yes | Yes | 5 | 3 |
Abbreviation: ASD; atrial septal defect, w; week
The shortest distance between the rectal pouch and the skin surface was between 8 and 20 mm, but the distance between the rectal pouch and the surface of skin via the anal sphincter path was longer and between 11 and 23 mm, or in other words, 3 - 8 mm (mean, 4.7 mm) longer.
There were rectourethral fistula in seven, rectovaginal fistula in one, rectovestibular fistula in one, and in another one patient, no fistula was detected. In the patient with rectovestibular fistula, anal sphincter complex was pushed back toward the coccygeal tip due to fecal material pressure.
The multi-layer view of anal pit was seen in all patients except for the rectovestibular fistula patient. The maximum multiple layer diameter of anal pit was 3 - 4 mm, but in the patient with cloacal anomaly, it was about 10 mm in the sagittal plane on the posterior of the perineal orifice. In most patients, the anal pit path until the center of the muscle complex had a curved and occasionally parasagittal path and it was not straight (Figure 1C). The visible length of multi-layer view of anal pit was 5 - 8 mm, and it attaches to the mucus of muscle complex internally and externally (Figure 1D).
Anal muscle sphincter complex could be seen in all patients. The muscle complex thickness was 2 - 3.6 mm, which was occasionally asymmetric (Figure 1E).
5. Discussion
There are many articles about the role of preoperative MRI in determining the type and level of anorectal malformation that can be helpful in planning and predicting the prognosis and also investigating the spinal and urethral anomalies that indirectly affect the management of disease and operation (2). MRI also has a role in these patients for demonstration of the status of sphincter muscle complex, the symmetry of the sphincter, and perirectal fibrosis (10, 11).
Sonography is usually used to determine the level of the disorder (low and high) indirectly based on the distance between location of anoplasty and pouch of rectum. Although this approach is not very determinative and there are a lot of diagnostic overlaps in this field (1, 7-9).
In review articles, we found only one paper about the detection of the passage of rectum from levator ani muscle in the transverse view of infra-coccygeal plane that could be helpful for differentiation of high and low groups (10). In the study, infra-coccygeal US was sited inferior to the coccyx and posterior to the anus for conducting the approach. Transverse images of the anorectal area were obtained by scanning. Sedation was not used during the procedure. Similar to our study, cases underwent colostomy. After that, a definitive repair pull-through was operated.
The pre-operative exact localization of anal pit and especially sphincter muscle complex with sonography can be helpful for surgeons to select less invasive approaches that determine the future fecal continence of the patient (12).
In this study, with accurate ultrasound investigation of the perineal region, we noticed two sonographic findings that can be helpful in patients with imperforate anus to determine the proper path of the anal canal for pull-through operation. These findings were multi-layered view of anal pit and sphincter muscle complex.
Multi-layered view of anal pit is exactly similar to gut signature and is determined as a peripheral hypoechoic layer with two central parallel echogenic lines. This view was probably the result of fetal anal pit as a result of non-ruptured anal membrane and/or non-route formation. This view was not seen in patients with recto-vestibular fistula. Although it had 3-4 mm diameter, in cloacal anomaly patient, it had about 10 mm anterior-posterior diameters in sagittal plane that was probably due to fetal merge of anal and vaginal orifices.
In most of patients, the anal pit was not straight and it had a parasagittal position and a slightly curved with eccentric attachment to the center of the sphincter muscle complex. These can explain the pathophysiology of the disease.
Anal sphincter and muscle complex was seen as a circular muscular tissue bulk that surrounds the echogenic mucus of the gastrointestinal tract. It was visible on the coronal plane at depth of subcutaneous fat of the perineal area with 2 - 3.6 mm thickness. This complex was visible in all of our 10 patients.
In addition, the result of this study shows that the distance between the rectal pouch and the skin without attention to the muscle sphincter is unreliable and can make serious pitfalls and unaware complications. In all patients, the distance between the rectal pouch and skin through the anal pit and muscle complex (11 mm) was longer than the shortened distance between the rectal pouch and the skin (3 - 8 mm, mean: 4.7 mm).
In lithotomy position, it is important to notice that the multi-layered view of the anal pit and anal sphincter complex was only visible in the coronal view and was invisible in the routine sagittal and transverse view, then it may be ignored and not noticed in studies. Therefore, we believe sonography is mandatory in both sagittal and coronial views. In the review of articles, we did not encounter a similar publication about the use of these findings in patients with imperforate anus, although there are many articles about the use of sonography in determining the anal sphincter complex in adults with various diseases (13, 14).
This is a preliminary cross sectional study with a low number of patients. In addition, the frequency of the ultrasonic probe device was our study limitation. Exact examination of the perineal region with high-frequency probes (14 to 20 MHz) with a high number of patients can provide better and more reliable results.
The multi-layer view of anal pit and the muscular bulk of anal sphincter complex are the two important sonographic findings that can better differentiate the level of anal malformation and act as an indicator for the location of anal sphincter pull through in patients with imperforate anus.