Abstract
Background:
There are many more trials for low-dose chest computed tomography (LDCT) screening than for chest radiography, as a recent study shows that low-dose chest CT screening for smokers may reduce lung cancer mortality.Objectives:
To assess the differences of low-dose CT imaging features between smokers and non-smokers.Patients and Methods:
A retrospective review of all current smokers who visited our hospital between August 2015 and May 2016 to quit smoking and who had received chest LDCT was conducted. The patients had received an LDCT screening during the same period; non-smokers were considered as the control group. The retrospective interpretation for the nodule numbers and size, lymphadenopathy, emphysema, bronchiectasis, as well as coronary artery calcifications was performed at univariate and multivariate analyses.Results:
Among 304 patients (130 in the non-smoker group and 174 in the smoker group), the number and diameter of nodules, pleural lesions, lymphadenopathy, and bronchiectasis were not significantly different between the smoker and non-smoker groups. Emphysema was detected in 11 (8.5%) patients in the non- smoker group and 75 (43.1%) in the smoker group. Coronary artery calcifications developed in 22 patients (16.9%) in the non-smoker group and 60 patients (34.5%) in the smoker group. Respiratory bronchiolitis developed in two patients (1.5%) in the non-smoker group and 13 patients (7.5%) in the smoker group. With an increase in the smoking period, emphysema and coronary artery calcifications significantly increased (P = 0.002 and P = 0.007, respectively).Conclusion:
In the LDCT findings, emphysema, coronary artery calcifications, and respiratory bronchiolitis were significantly different between smokers and non-smokers. In multivariate analysis, emphysema was only significantly different between smokers and non-smokers. With an increase in the smoking period, the occurrence of emphysema and coronary artery calcifications increased as well at univariate and multivariate analysis.Keywords
Smoking Cessation Emphysema Coronary Artery Disease Computed Tomography
1. Background
The demand for low-dose computed tomography (LDCT) is increasing for the screening of lung cancer. There are many more trials for low-dose CT screening than for chest radiography, as a recent study shows that low-dose CT screening for smokers may reduce lung cancer mortality (1). Until now, smoking-related lung diseases, such as emphysema, respiratory bronchiolitis, acute eosinophilic pneumonia, and lung cancer have become widely known (2). However, there have been no studies for comparison of the overall CT findings between smokers and nonsmokers.
2. Objectives
Recently, a smoking cessation program has started in our institution. People willing to quit smoking visited our hospital for a low-dose CT scan and we investigated the CT findings for these patients. During the same period, non-smoker patients who visited the hospital for general health screening and CT were designated as the control group. The aim of this study was to evaluate the differences of the LDCT findings between smokers and non-smokers.
3. Patients and Methods
3.1. Patients
The present retrospective study was approved by the institutional review board and informed consent was waived from all patients. Between August 2015 and May 2016, 278 current smokers visiting Hallym University hospital to quit smoking underwent low-dose chest computed tomography (LDCT). Among these patients, 21 patients were excluded, 20 due to the lack of available precise information of their smoking history and one due to his ex-smoker status. Of the remaining 257 patients, 55 were excluded, because they had previous inflammatory/infectious sequelae. Of the remaining 202 patients, 27 patients with active diseases such as active tuberculosis, pneumonia, interstitial lung disease were excluded. Among the remained final 175 patients, only one patient was diagnosed with lung cancer and this patient was excluded. During the study period, the number of patients who had undergone LDCT for general health screening was 526. Among these patients, 164 non-smokers were considered as the control group. Of these 164, 21 patients were excluded due to their previous infectious/inflammatory sequelae. Of the remaining 143, after exclusion of 13 patients with active diseases such as active tuberculosis, pneumonia, eosinophilic infiltration, and nontuberculous mycobacteria (NTM), 130 patients were included in the control group.
3.2. CT Technique
For all patients, the LDCT examination was performed by using a 256-section multidetector CT machine (Somatom Definition Flash; Siemens Healthcare, Forchheim, Germany) and a 64-section multidetector CT machine (Brilliance 64; Phillips Medial Systems, Haifa, Israel). All patients were received in the supine position, from lung apex to adrenal glands (120 kVp, and 40 mA), and the images were reconstructed in the 3mm axial plane and the 1mm coronal plane. Contrast-enhanced studies were not performed.
3.3. Imaging Analysis
The LDCT scans of the patients were reviewed in consensus with two radiologists (IJ Lee with 19 years of experience and HY Song with 3 years of experience) on our picture archiving and communication system (PACS). If the opinions of the two radiologists did not converge, consensus was reached through discussion. The reviewers evaluated the numbers and size of the nodules, presence or absence of lymphadenopathy, emphysema, bronchiectasis, coronary artery calcifications, and respiratory bronchiolitis. If the patients had their prior studies, the CT scans were used to compare the lesions.
For each patient, the number of nodules was recorded and the diameter of the largest nodule was measured. A nodule was defined as a small, rounded opacity within the pulmonary interstitium, less than or equal to 3 centimeters. The number of nodules was classified 0, 1, 2, 3, 4, 5 and multiple. Furthermore, the presence or absence of pleural thickening, pleural effusion, and associated lymphadenopathy were evaluated. Emphysema, which is already known to be associated with smoking was also compared. Emphysema was assigned a score based on visual assessment. The score reflected the extent of emphysema in the upper, mid, and lower zones of each lung as measured on a 6-point scale, (1: absent; 2: < 5%; 3: 6 - 25%; 4: 26 - 50%; 5: 51 - 75% or 6: 76 - 100%) (3). Bronchiectasis was also accessed by its degree. The score of bronchial dilatation was quantified relative to the adjacent pulmonary artery as follows: 0 = none, 1 = 100% - 200% arterial diameter; 2 = 200% - 300% arterial diameter; 3 ≥ 300% arterial diameter (4). Coronary artery calcifications were evaluated and the number of involvement of three main branches (left anterior descending artery, left circumflex artery, right coronary artery) was also recorded. Finally, respiratory bronchiolitis was compared between the two groups.
Smokers and non-smokers were compared based on the above factors. In the smoker group, the findings were also compared according to the smoking period to see if there was a significant difference between the patients with different histories of smoking. The smoker group was further divided into four subgroups with the total length of smoking history; less than 20 pack years; 20 to 30 pack years; 30 to 40 pack years; and more than 40 pack years. A pack year was defined as twenty cigarettes smoked everyday for one year.
3.4. Statistical Analysis
The initial consensus review was used for the data analysis. The Mann-Whitney U test was used to compare the number and diameter of the nodules between the smoker and non-smoker groups. The Fisher exact test was used to compare the presence or absence of pleural thickening, pleural effusion, lymphadenopathy, emphysema, bronchiectasis, coronary artery calcification, and respiratory bronchiolitis at univariate analysis. A multivariate logistic regression analysis was performed to test the adjusted association between smoking and significant potential factors. The grade of coronary artery calcifications was compared using Trend test. Visual emphysema scores were compared using a Wilcoxon two-sample rank sum test due to the ordinal scale on which visual emphysema grading was based. The comparison of subgroups according to the smoking period was evaluated using the one-way analysis of variance (ANOVA). P < 0.05 was considered statistically significant for all analyses.
4. Results
The percentage of males was 87.9% (153 of 174) in the smoker group and 67.7% (88 of 130) in the non-smoker group. The mean age of non-smokers was 49.78 years, while that of smokers was 54.26 years. For the two groups, the mean number of nodules was 1.42 (standard deviation [SD], ± 0.142) for non-smokers and 1.73 (SD ± 0.151) for smokers. No significant differences were observed between the two groups (P = 0.454). For all patients, the diameter of the largest nodule was measured and the mean diameter was calculated. The mean diameter amounted to 2.98 (SD ± 0.241) in the non-smoker group and 3.62 (SD ± 0.496) in the non-smoker group, again with no significant difference between the groups (P = 0.999). During the study period, among the patients who had undergone LDCT, only one patient was diagnosed with lung cancer and this patient was a smoker with 40 pack years. The size of the mass was measured 7.6 centimeters on CT. There were no significant differences in pleural thickening, pleural effusion, lymphadenopathy, and bronchiectasis between the two groups (Table 1). For emphysema, the presence of this lesion was 11 of 130 (8.5%) in the non-smoker group and 75 of 174 (43.1%) in the smoker group, so a significant difference between the two groups was observed (P < 0.001). Coronary artery calcifications were compared among these patients. Of a total of 304 patients, 82 patients had coronary artery calcifications: 22 (16.9%) and 60 (34.5%) in the non-smoker and the smoker groups, respectively. The difference between the two groups with regard to coronary artery calcifications was statistically significant (P < 0.001). Furthermore, the presence or absence of respiratory bronchiolitis was observed in two (1.5%) non-smoker patients and 13 (7.5%) smoker patients, and the difference was statistically significant (P = 0.029). In sum, significant differences in emphysema, coronary artery calcifications, and respiratory bronchiolitis were observed between the two groups.
Univariate and Multivariate Analysis of Differences of CT Findings Between Smokers and Nonsmokersa
| Smoker | Non-smoker | Univariate analysis | Multivariate analysisb | OR (95% CI) | |
|---|---|---|---|---|---|
| (N = 174) | (N = 130) | (P value) | (P value) | ||
| Nodule number | 1.73 ± 0.151 | 1.42 ± 0.142 | 0.454 | - | - |
| Nodule diameter | 3.62 ± 0.496 | 2.98 ± 0.241 | 0.999 | - | - |
| Pleural thickening | 9 (5.2) | 2 (1.5) | 0.124 | - | - |
| Pleural effusion | 1 (0.6) | 2 (1.5) | 0.578 | - | - |
| Lymphadenopathy | 13 (7.5) | 7 (5.4) | 0.468 | - | - |
| Emphysema | 75 (43.1) | 11 (8.5) | < 0.001 | < 0.001b | 5.476 (2.680 - 11.192) |
| Bronchiectasis | 11 (6.3) | 6 (4.6) | 0.522 | - | - |
| Coronary artery calcifications | 60 (34.5) | 22 (16.9) | < 0.001 | 0.271b | 1.441 (0.752 - 2.761) |
| Respiratory bronchiolitis | 13 (7.5) | 2 (1.5) | 0.029 | 0.127b | 3.349 (0.710 - 15.804) |
In multivariate analysis, adjusted for sex and age, emphysema was significantly associated with smoking (odds ratio [OR], 5.476; 95% confidence interval [CI], 2.680 to 11.192; P < 0.001). Multivariate analysis demonstrated that coronary artery calcification was not significantly associated with smoking (OR, 1.441; 95% CI, 0.752 to 2.761; P = 0.271). Respiratory bronchiolitis was associated with smoking (OR, 3.349; 95% CI, 0.710 to 15.804; P = 0.127). However, there was no statistically significant difference (Table 1).
Furthermore, the smoker group was further subdivided into four groups according the smoking period and these findings were then compared (Table 2). No associations between the smoking period and emphysema were observed (32.6%, 25.6%, 57.1% and 58.1%, respectively). However, when the smoker group was divided into two groups by 30 pack years, the high smoking group was significantly higher than the low smoking group for the presence of emphysema (57.6% vs. 29.2%; P < 0.001). Emphysema was also significantly associated with smoking period in multivariate analysis (OR, 1.652; 95% CI, 1.351 to 2.020; P < 0.01) (Figure 1). Furthermore, associations between the smoking period and coronary artery calcifications were found. The longer the smoking period, the higher the percentage of patients with coronary artery calcifications (21.7%, 25.6%, 38.1% and 53.5%; P = 0.006). In multivariate analysis, coronary artery calcifications demonstrated borderline statistically significant association with smoking period (OR, 1.229; 95% CI, 0.999 to 1.511; P = 0.051). However, there was no association between the smoking period and respiratory bronchiolitis (P = 0.297).
| Less than 20 pack-year | 20~30 pack-year | 30~40 pack-year | More than 40 pack-year | Univariate analysis | Multivariate analysisb | OR (95% CI) | |
|---|---|---|---|---|---|---|---|
| (N = 46) | (N = 43) | (N = 42) | (N = 43) | (P value) | (P value) | ||
| Emphysema | 15 (32.6) | 11 (25.6) | 24 (57.1) | 25 (58.1) | 0.002 | < 0.001b | 1.652 (1.351 - 2.020) |
| Coronary artery calcifications | 10 (21.7) | 11 (25.6) | 16 (38.1) | 23 (53.5) | 0.006 | 0.051b | 1.229 (0.999 - 1.511) |
| Respiratory bronchiolitis | 2 (4.3) | 6 (13.9) | 2 (4.8) | 3 (7.0) | 0.297 | 0.440b | 1.153 (0.804 - 1.653) |
A, Axial low dose computed tomography (LDCT) scan of a 55-year-old nonsmoker shows no emphysema. B, LDCT in a 56-year-old man who is a 26 pack-year smoker. Axial CT scan shows mild emphysema in bilateral lungs with lobe predominance in both lungs. C, LDCT scan of a 55-year-old male smoker with a pack-year history of 140 shows diffuse emphysema in bilateral lungs.
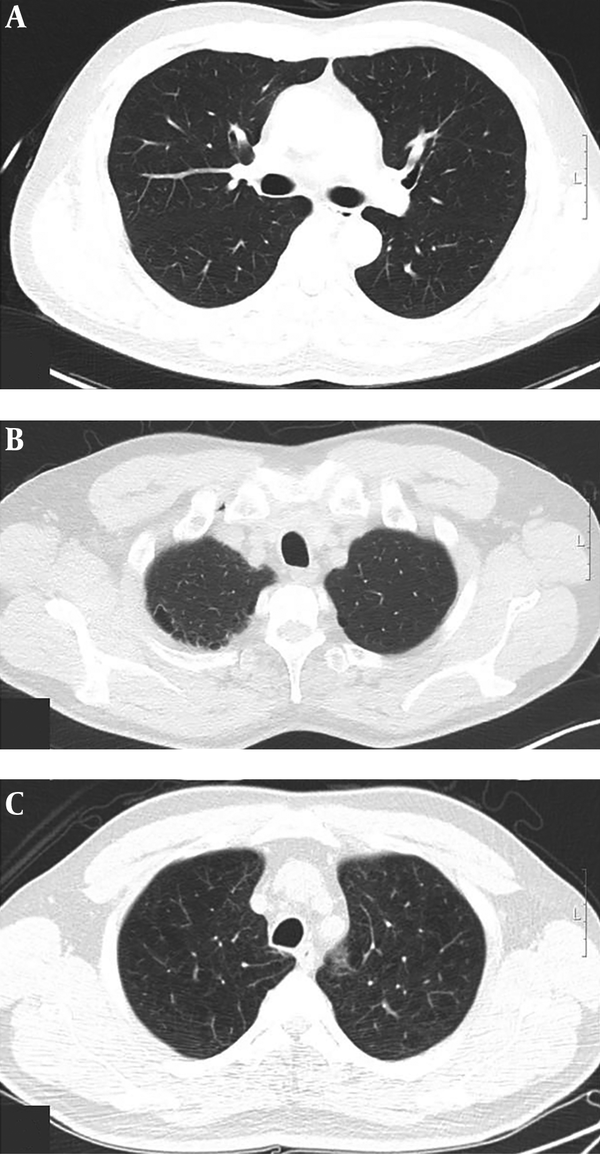
The extent of emphysema for lung zones was rated on a 6-point scale based on visual assessment (Table 3) (3). The degree of emphysema in the smoker group was higher than that in the non-smoker group (right upper lung [RUL], 2.50 ± 1.16 vs. 2.09 ± 0.83; right middle lung [RML], 1.69 ± 0.98 vs. 1.45 ± 0.69; right lower lung [RLL], 1.77 ± 1.01 vs. 1.55 ± 0.93; left upper lung [LUL], 2.24 ± 1.03 vs. 1.91 ± 0.70; left middle lung [LML], 1.72 ± 0.93 vs. 1.45 ± 0.69; let lower lung [LLL], 1.80 ± 1.02 vs. 1.45 ± 0.69 for smokers vs. non-smokers, respectively). However, these differences did not reach statistical significance (P = 0.265, P = 0.446, P = 0.491, P = 0.303, P = 0.373, P = 0.285, respectively).
| Lung zone | Smoker (N = 74) | Non-smoker (N = 11) | P value |
|---|---|---|---|
| Right upper lung zone | 2.50 ± 1.16 | 2.09 ± 0.83 | 0.265 |
| Right middle lung zone | 1.69 ± 0.98 | 1.45 ± 0.69 | 0.446 |
| Right lower lung zone | 1.77 ± 1.01 | 1.55 ± 0.93 | 0.491 |
| Left upper lung zone | 2.24 ± 1.03 | 1.91 ± 0.70 | 0.303 |
| Left middle lung zone | 1.72 ± 0.93 | 1.45 ± 0.69 | 0.373 |
| Left lower lung zone | 1.80 ± 1.02 | 1.45 ± 0.69 | 0.285 |
The degree of bronchiectasis was also divided into three subgroups (mild, moderate, and severe) (4). The total number of patients with bronchiectasis was 17 (7 non-smokers and 11 smokers). The mild degree was seen among three non-smokers and six smokers. Three non-smokers and four smokers had a moderate degree, and none of the non-smokers and one smoker had a severe degree of bronchiectasis. However, since there was no significant difference between the two groups, division by the degree proved to be meaningless.
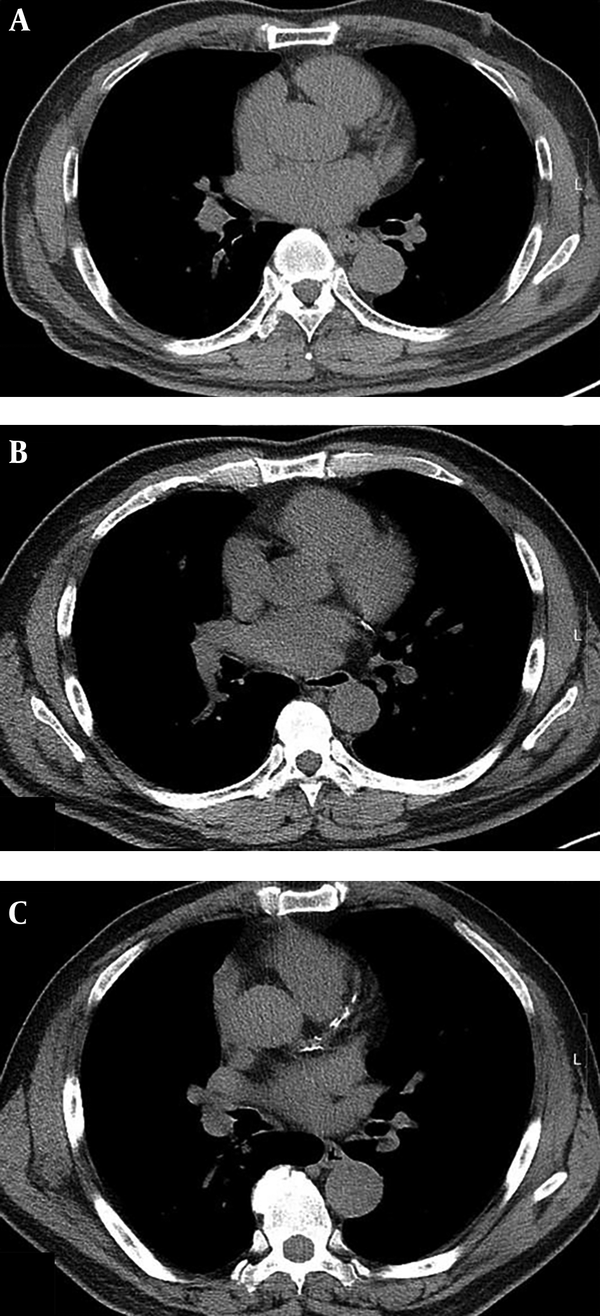
Regardless of the degree of severity, the degrees of coronary artery calcifications were subcategorized to 1, 2, and 3, according to the number of the coronary arteries involved (right coronary artery, left anterior descending artery, and left circumflex coronary artery). In the non-smoker group, the number of patients with coronary artery calcifications was 13 (10.0%) for only one artery involvement, five (3.8%) for two vessel involvement, and four (3.1%) for three vessel involvement. In the smoker group, the number of patients with coronary artery calcifications was 38 (21.8%) for only one vessel involvement, 16 (9.2%) for two vessel involvement, and six (3.4%) for three vessel involvement (Figure 2). There was no significant difference between the two groups.
A, Axial low dose computed tomography (LDCT) scan of a 64-year-old nonsmoker shows no coronary artery calcification. B, LDCT in a 62-year-old male smoker who has a 30 pack-year history. Axial CT scan shows coronary artery calcification at the left circumflex artery. C, LDCT scan of a 66-year-old male smoker with a 45 pack-year history shows coronary artery calcifications at the left anterior descending artery and right coronary artery.
5. Discussion
According to world health organization, the proportion of female smokers is higher in high-income countries, including most countries of Western Europe. However, the proportion of female smokers is still low in many low- and middle-income countries, including eastern societies, although it has increased as compared to the past. Therefore, the percentage of men who were enrolled in this program was also high. Accordingly, we observed a difference in gender distribution between smokers and non-smokers in our study.
Meaningful differences were observed in respiratory bronchiolitis and emphysema, for which smoking has already been known as a risk factor (2), and this is consistent with the results of previous studies (5, 6). In this study, we further investigated whether presence or absence of emphysema and respiratory bronchiolitis differed according to the smoking period. The results of our retrospective study showed that the quantity of cigarette smoking (pack years) was negatively correlated with pulmonary function test and positively correlated with chronic obstructive pulmonary disease grade (7, 8). Our study also examined the association of emphysema severity according to the smoking period and the results yielded no association when the smoker group was subdivided into four subgroups according to the length of their smoking history. However, when the smokers were divided into two groups based on 30 pack year, statistically significant results were observed for emphysema (but not for respiratory bronchiolitis). In multivariate analysis with adjusting for age and sex, the emphysema were also statistically significantly more common in the smoker group, and emphysema was significantly more frequent with an increase of the duration of smoking history.
The association between smoking and cardiovascular diseases is well established in prior research (9). Pakdaman et al. (10) reviewed the prognostic value of coronary artery calcifications for cardiovascular diseases. Therefore, detection of coronary artery calcification is important due to its clinical significance. Although there was no statistically significant result in multivariate analysis, the results of our study show that coronary artery calcifications were also more common in the smoker group in univariate analysis.
There is a lack of studies on the association of coronary artery calcifications with smoking duration. One of previous studies revealed that smoking duration was positively correlated with coronary artery calcification in middle-aged Japanese men, whereas the smoking period was not found to be significantly associated with coronary artery calcification in middle-aged Korean men (11). However, our study shows that coronary artery calcifications were borderline significantly more frequent with an increase of the duration of smoking history.
The degree of emphysema was assessed based on visual assessment. The results on this procedure suggested that smokers showed a slightly higher degree of emphysema, but the difference did not reach statistical significance. In our study, the degree of emphysema was divided between grades 1 to 6, but there were few cases of severe emphysema of grade 4 or higher. Non-smoker had not degree of 5 or 6, and degree 4 was only two patients. Regardless of the duration of the smoking period, only five of the smokers were grade 6 and six smokers were grade 5. Since there were too few cases of severe degree, the difference between non-smokers and smokers remains unclear. This particular research requires further studies.
Furthermore, smoking has not been found to be a direct cause of bronchiectasis. However, smoking and repeated infections may worsen pulmonary function and accelerate the disease progression (12, 13). Our study found no significant difference in the degree of bronchiectasis, but there was one patient with severe bronchiectasis (degree 3) in the smoker group. Most patients with bronchiectasis have a history of previous infection with underlying NTM infection and tuberculosis and these infections are also associated with smoking. Thus, this is a limitation of the present study, because these patients were excluded from the sample we studied.
There are several limitations in our study. First, because the follow-up period was relatively short, few patients underwent follow-up CT in the meantime and lung cancer incidence was not observed. During the study period, one 40 pack years smoker was diagnosed with lung cancer in our study, but this patient was excluded from the sample. Therefore, in our study, the difference in lung cancer detection between smokers and non-smokers could not be studied, though this parameter would be important to compare our other CT findings too.
Second, visual assessment was performed to evaluate the degree of emphysema and no quantification was performed. There was difficulty in performing quantitative analysis at the time of the initial reading, because this study was conducted retrospectively and re-reviewed CT findings that had already been interpreted. So two radiologists reviewed the CT scans in consensus and discussed for discrepancies. A recent study reveals that visual assessment of emphysema is helpful in the lung cancer risk analysis and the presence of emphysema is associated with lung cancer occurrence (3). Therefore, it is reasonable to compare the differences between the two groups without quantitative analysis in our study. However, further quantitative study should be required to assess these issues.
Finally, the Agatston calcium score, which is commonly used for the evaluation of coronary artery calcification, was not calculated in the present study and only the involvement counts of the main coronary artery were compared (14). Therefore, our study only evaluated the number of involved coronary arteries regardless of grade. Further studies for calcifications of coronary arteries will be needed using advanced techniques such as 3D reconstruction.
In conclusion, LDCT-based findings of the present study suggest that emphysema, coronary artery calcifications, and respiratory bronchiolitis are significantly different between smokers and non-smokers. No significant differences were observed for other studied factors. In multivariate analysis, the emphysema was only significantly different between smokers and non-smokers. Our results also suggest that, with an increase of the smoking period, the incidence of emphysema and coronary artery calcifications increase as well at univariate and multivariate analysis.
References
-
1.
Gulia V. Amsterdam Long-Term outcomes of a pilot CT screening for lung cancer: 10-years results, MO05.07. 2011. Available from: https://www.webges.com/cslide/library/wclc/.com.
-
2.
Attili AK, Kazerooni EA, Gross BH, Flaherty KR, Myers JL, Martinez FJ. Smoking-related interstitial lung disease: radiologic-clinical-pathologic correlation. Radiographics. 2008;28(5):1383-96. discussion 1396-8. [PubMed ID: 18794314]. https://doi.org/10.1148/rg.285075223.
-
3.
Wille MM, Thomsen LH, Petersen J, de Bruijne M, Dirksen A, Pedersen JH, et al. Visual assessment of early emphysema and interstitial abnormalities on CT is useful in lung cancer risk analysis. Eur Radiol. 2016;26(2):487-94. [PubMed ID: 25956938]. https://doi.org/10.1007/s00330-015-3826-9.
-
4.
Ibrahim RM, Elnekeidy A, Rizk A, Yossef A, Abdelrahman S. Correlation between a proposed MDCT severity score of bronchiectasis and pulmonary function tests. Egypt J Radiol Nucl Med. 2016;47(2):413-20. https://doi.org/10.1016/j.ejrnm.2016.02.012.
-
5.
Fraig M, Shreesha U, Savici D, Katzenstein AL. Respiratory bronchiolitis: a clinicopathologic study in current smokers, ex-smokers, and never-smokers. Am J Surg Pathol. 2002;26(5):647-53. [PubMed ID: 11979095]. https://doi.org/10.1097/00000478-200205000-00011.
-
6.
Yasunaga K, Cherot-Kornobis N, Edme JL, Sobaszek A, Boulenguez C, Duhamel A, et al. Emphysema in asymptomatic smokers: quantitative CT evaluation in correlation with pulmonary function tests. Diagn Interv Imaging. 2013;94(6):609-17. [PubMed ID: 23601360]. https://doi.org/10.1016/j.diii.2013.02.013.
-
7.
Zhang J, Lin XF, Bai CX. Comparison of clinical features between non-smokers with COPD and smokers with COPD: a retrospective observational study. Int J Chron Obstruct Pulmon Dis. 2014;9:57-63. [PubMed ID: 24426780]. [PubMed Central ID: PMC3890400]. https://doi.org/10.2147/COPD.S52416.
-
8.
Liu Y, Pleasants RA, Croft JB, Wheaton AG, Heidari K, Malarcher AM, et al. Smoking duration, respiratory symptoms, and COPD in adults aged ≥45 years with a smoking history. Int J Chron Obstruct Pulmon Dis. 2015;10:1409-16. [PubMed ID: 26229460]. [PubMed Central ID: PMC4516194]. https://doi.org/10.2147/COPD.S82259.
-
9.
Bullen C. Impact of tobacco smoking and smoking cessation on cardiovascular risk and disease. Expert Rev Cardiovasc Ther. 2008;6(6):883-95. [PubMed ID: 18570625]. https://doi.org/10.1586/14779072.6.6.883.
-
10.
Pakdaman MN, Rozanski A, Berman DS. Incidental coronary calcifications on routine chest CT: Clinical implications. Trends Cardiovasc Med. 2017;27(7):475-80. [PubMed ID: 28583439]. https://doi.org/10.1016/j.tcm.2017.04.004.
-
11.
Hirooka N, Kadowaki T, Sekikawa A, Ueshima H, Choo J, Miura K, et al. Influence of cigarette smoking on coronary artery and aortic calcium among random samples from populations of middle-aged Japanese and Korean men. J Epidemiol Community Health. 2013;67(2):119-24. [PubMed ID: 22844083]. [PubMed Central ID: PMC3521870]. https://doi.org/10.1136/jech-2011-200964.
-
12.
Rezende Goncalves J, Corso Pereira M, Figueiras Pedreira De Cerqueira EM, Oliveira Magro D, Mello Moreira M, Paschoal IA. Severe obstructive disease: similarities and differences between smoker and non-smoker patients with COPD and/or bronchiectasis. Rev Port Pneumol. 2013;19(1):13-8. [PubMed ID: 23017504]. https://doi.org/10.1016/j.rppneu.2012.05.003.
-
13.
Popa V. Airway obstruction in adults with recurrent respiratory infections and IgG deficiency. Chest. 1994;105(4):1066-72. [PubMed ID: 8162726]. https://doi.org/10.1378/chest.105.4.1066.
-
14.
Kirsch J, Buitrago I, Mohammed TL, Gao T, Asher CR, Novaro GM. Detection of coronary calcium during standard chest computed tomography correlates with multi-detector computed tomography coronary artery calcium score. Int J Cardiovasc Imaging. 2012;28(5):1249-56. [PubMed ID: 21833776]. https://doi.org/10.1007/s10554-011-9928-9.
