Abstract
Keywords
Adrenal Gland Neoplasm Epithelioid Hemangioendothelioma Adrenalectomy Laparoscopy Male Human
1. Introduction
Epithelioid hemangioendothelioma (EHE) is a rare vascular endothelial tumor of unknown etiology that shows a variable clinical course (1) and was first described by Weiss and Enzinger in 1982 (2). EHE represents less than 1% of all vascular tumors and usually develops in the soft tissues, lung, liver, or bone, although involvement of the head and neck area, breast, lymph nodes, skin, abdomen, and other sites is possible (3). EHEs are very rare in the urinary tract, although a few cases in the kidney and bladder have been reported (4, 5). Due to its rarity, EHE arising from the adrenal gland is scarcely described and is poorly understood in terms of imaging findings, treatment options, and the clinical course. Here, we report a case of primary adrenal EHE in a young male patient that was incidentally detected on computed tomography (CT) examination.
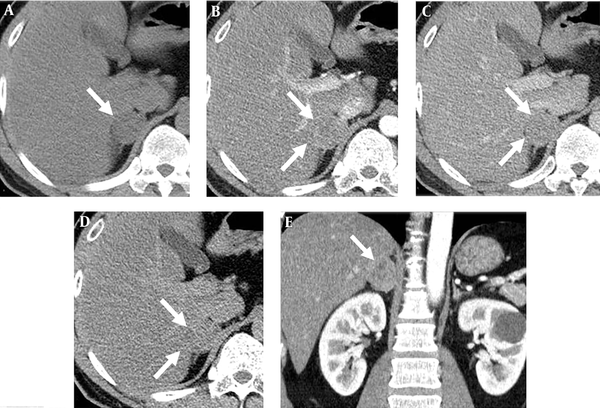
A 33-year-old man with microscopic hematuria. Computed tomography (CT) with adrenal protocol. A, Pre-enhanced image. B, Image at 1 min after contrast enhancement. C, Image at 2 min after contrast enhancement. D, Image at 15 min after contrast enhancement. E, Coronal reformatted image of 1-min post-enhanced scan. A well-defined low-grade enhancing solid mass with slight heterogeneous enhancement was noted in the right adrenal gland, but no necrosis, hemorrhage, or calcification was observed.
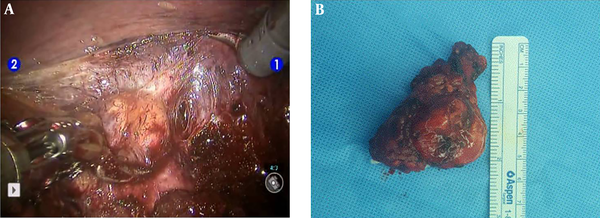
A, Intraoperative image during laparoscopic excision. B, The gross specimen of the resected adrenal tumor. The upper margin of the adrenal gland was densely adhered to the adjacent liver. The adrenal tumor was a well-defined solid mass.
Histologic findings of the adrenal tumor. A, The gross specimen of the adrenal tumor. B, Hematoxylin and eosin (H&E) staining (× 40); [N: normal adrenal gland; T: tumor]. C, H&E staining (× 200). D, Immunohistochemical staining for CD31 (× 100). Microscopic examination indicated vascular neoplasm and the tumor cells were positive for CD31, CD34 and reticulin; the Ki-67 proliferation index was low (< 10%).
![Histologic findings of the adrenal tumor. A, The gross specimen of the adrenal tumor. B, Hematoxylin and eosin (H&E) staining (× 40); [N: normal adrenal gland; T: tumor]. C, H&E staining (× 200). D, Immunohistochemical staining for CD31 (× 100). Microscopic examination indicated vascular neoplasm and the tumor cells were positive for CD31, CD34 and reticulin; the Ki-67 proliferation index was low (< 10%). Histologic findings of the adrenal tumor. A, The gross specimen of the adrenal tumor. B, Hematoxylin and eosin (H&E) staining (× 40); [N: normal adrenal gland; T: tumor]. C, H&E staining (× 200). D, Immunohistochemical staining for CD31 (× 100). Microscopic examination indicated vascular neoplasm and the tumor cells were positive for CD31, CD34 and reticulin; the Ki-67 proliferation index was low (< 10%).](https://services.brieflands.com/cdn/serve/31453/213c5229875aede72486a6aae659bc5332bd69f4/iranjradiol-15-4-64787-i003-preview.png)
2. Case Presentation
A 33-year-old male presented at our institution for evaluation of microscopic hematuria. He had no specific past medical history and no relevant symptoms. There was unremarkable findings on physical examination. He underwent contrast-enhanced CT, and an incidental right adrenal mass was detected. There was no other abnormal findings such as urolithiasis or mass in both kidneys and urinary tracts except for a simple cyst in left kidney. Subsequent adrenal CT consisting of a pre-enhanced and contrast-enhanced scans at 1 minutes, 2 minutes, and 15 minutes was performed to characterize the adrenal mass. The adrenal mass measured up to 3.5 cm in long diameter and exhibited persistently low-grade enhancement, barely discernible from adjacent liver parenchyma on three contrast-enhanced scans at 1 minutes, 2 minutes, and 15 minutes. On coronal reformatted images, the lesion exhibited somewhat heterogeneous enhancement with slight marginal lobulations. Attenuation was calculated at 22 Hounsfield units (HU) (> 10 HU) in the pre-enhanced scan, the absolute washout value was 37% (< 60%), and the relative washout value was 25% (< 40%), indicating a non adenomatous tumor (Figure 1). Although typical benign adenoma was ruled out, the specific radiologic diagnosis was challenging. Because the lesion represented nonspecific radiologic findings and common non adenomatous tumor such as metastasis, pheochromocytoma or tuberculosis did not correspond with this case. Therefore, we reported this case as unspecified non adenomatous tumor or atypical adrenal adenoma because rarely adenoma can manifest low washout value due to hemorrhage, necrosis, and degeneration. Preoperative laboratory data revealed no endocrinological abnormality.
Robotic adrenalectomy was performed via a transperitoneal approach. There was no adhesion or other surgical difficulty during dissection of the adrenal gland, except for the upper margin of the adrenal mass, which was densely adhered to the adjacent liver (Figure 2). The surgery was successfully completed without any complications, and there were no fluctuations in vital signs during surgery.
The resected adrenal tumor was a well-capsulated ovoid mass measuring 3.5 × 3.0 × 2.5 cm3 that exhibited a whitish fibrous cut surface with multiple yellowish entrapped adrenal tissue sections. No necrosis or hemorrhage was found. Histologically, the tumor comprised solid nests of epithelioid cells and vascular channels. The tumor cells had round or ovoid nuclei and characteristic cytoplasmic vacuoles. Mitosis was less than 1 per 10 high-power field (HPF), and there was little nuclear pleomorphism. The tumor cells were strongly positive for cluster of differentiation 31 (CD31) on immunohistochemical staining (Figure 3). The final diagnosis was EHE arising from the adrenal gland.
Immediate postoperative CT scanning revealed a small amount of fluid collection in the adrenalectomy bed. However, this was resolved on the follow-up CT, and the patient was doing well 3 months after surgery.
3. Discussion
We described an incidentally detected adrenal EHE, which was successfully treated by laparoscopic excision. The adrenal EHE showed nonspecific radiologic findings and therefore, correct preoperative diagnosis was challenging. However, with adrenal CT consisted of four phases including pre, post enhanced scans at 1 minutes, 2 minutes and 15 minutes, non adenomatous tumor was diagnosed and appropriate further evaluation with surgical excision could be performed.
EHE has been rarely reported in the urologic system, leading to scarcity of data on adrenal EHE. There have been a few case reports of adrenal EHE in infants (6, 7) and EHE involving the liver and adrenal gland (presumed metastatic adrenal lesion with primary hepatic EHE) (8). However, to our knowledge, there is only one case reporting primary adrenal EHE in an adult patient (9).
The imaging features of adrenal EHE are not established in the literature, and no specific radiologic findings are known. The case presented by Bozkurt et al. (9) exhibited a more heterogeneously enhancing tumor with central necrosis, irregular margin, and focal calcification compared to our case; smoother margin and homogeneous attenuation were observed in our case. The different imaging features for the same disease entity may stem from histologic heterogeneity of EHE itself (1). However, adrenal CT contributed to differential diagnosis and treatment planning for this adrenal tumor because > 10 HU on a pre-enhanced scan and low washout values calculated from adrenal protocols could rule out benign adenoma. Therefore, a nonadenomatous tumor was suggested and was safely excised by laparoscopy.
Definitive diagnosis of EHE is possible on pathologic examination. Microscopic evidence of vascular differentiation and expression of endothelium-specific markers CD31, CD34, and factor VIII can be used to make a correct diagnosis (8).
EHE is a low- to intermediate-grade malignant tumor with indeterminate biologic behavior. This tumor has unpredictable malignant potential ranging between benign hemangioma and epithelioid forms of angiosarcoma (3). The prognostic factors for EHE have not yet been well established. Previous articles have reported that the presence of pulmonary lesions, multiorgan involvement, disease progression, age > 55 years, tumor size > 3 cm, and male sex may be factors indicating worse prognosis (10). The presence of necrosis, notable mitosis (> 10 mitosis/HPF), and marked nuclear atypia also reportedly increase the risk of metastasis; (11) whereas, Makhlouf et al. reported that histology of the tumor, nuclear pleomorphism, and mitotic count are of no value in predicting the clinical outcome (12). In our case, the adrenal mass showed no necrosis or hemorrhage, little nuclear pleomorphism, and scant mitosis (< 1/10 HPF), and the patient was young (< 50 year); therefore, we can assume a good prognosis, although longer follow-up after surgery is needed.
Primary adrenal EHE is very rare; hence, preoperative diagnosis is challenging and requires a high degree of suspicion. The definitive diagnosis depends on histopathological and immunohistochemical features. Nonetheless, our case could be properly managed with surgical excision after preoperative adrenal CT revealed diagnostic features of non adenomatous tumor. Although this case appears to have favorable prognostic factors and laparoscopic excision was successfully performed, regular follow-up is required to monitor local recurrence and distant metastasis.
Acknowledgements
References
-
1.
Lauffer JM, Zimmermann A, Krahenbuhl L, Triller J, Baer HU. Epithelioid hemangioendothelioma of the liver: A rare hepatic tumor. Cancer. 1996;78(11):2318-27. https://doi.org/10.1002/(sici)1097-0142(19961201)78:11<2318::aid-cncr8>3.0.co;2-i.
-
2.
Weiss SW, Enzinger FM. Epithelioid hemangioendothelioma a vascular tumor often mistaken for a carcinoma. Cancer. 1982;50(5):970-81. https://doi.org/10.1002/1097-0142(19820901)50:5<970::aid-cncr2820500527>3.0.co;2-z.
-
3.
Weiss SW, Ishak KG, Dail DH, Sweet DE, Enzinger FM. Epithelioid hemangioendothelioma and related lesions. Semin Diagn Pathol. 1986;3(4):259-87. [PubMed ID: 3303234].
-
4.
Xiao Y, Wang C, Song Y, Wang C, Wang X, Zhang X, et al. Primary epithelioid hemangioendothelioma of the kidney: the first case report in a child and literature review. Urology. 2013;82(4):925-7. [PubMed ID: 23726166]. https://doi.org/10.1016/j.urology.2013.04.006.
-
5.
Jain D, Sharma MC, Epari S, Gupta NP, Kolla SB. Hemangioendothelioma of urinary bladder--report of rare case. Urology. 2009;73(6):1259-61. [PubMed ID: 19232692]. https://doi.org/10.1016/j.urology.2008.12.043.
-
6.
Kim ME, Fallon SC, Lopez ME, Hicks MJ, Brandt ML. Recurrent hemangioendothelioma in a pediatric patient: report and review of the literature. J Pediatr Surg. 2013;48(6):1426-8. [PubMed ID: 23845642]. https://doi.org/10.1016/j.jpedsurg.2013.03.064.
-
7.
Soboleski D, Mehta S, Kamal I, Dexter D, Poenaru D. Hemangioendothelioma of the adrenal gland in a 4-month-old male infant. AJR Am J Roentgenol. 1999;172(1):235-7. [PubMed ID: 9888774]. https://doi.org/10.2214/ajr.172.1.9888774.
-
8.
Kamath SM, Nagaraj HK, Mysorekar VV. Hepatic and adrenal hemangioendothelioma-a case report. J Clin Diagn Res. 2013;7(11):2583-4. [PubMed ID: 24392409]. [PubMed Central ID: PMC3879870]. https://doi.org/10.7860/JCDR/2013/6808.3620.
-
9.
Bozkurt O, Demir O, Yener S, Tuna B, Secil M, Yorukoglu K. Malignant epithelioid hemangioendothelioma of the adrenal gland treated by laparoscopic excision. Urology. 2015;85(3):e15-6. [PubMed ID: 25733308]. https://doi.org/10.1016/j.urology.2014.12.016.
-
10.
Mesquita RD, Sousa M, Trinidad C, Pinto E, Badiola IA. New Insights about Pulmonary Epithelioid Hemangioendothelioma: Review of the Literature and Two Case Reports. Case Rep Radiol. 2017;2017:5972940. [PubMed ID: 28884037]. [PubMed Central ID: PMC5573100]. https://doi.org/10.1155/2017/5972940.
-
11.
Sardaro A, Bardoscia L, Petruzzelli MF, Portaluri M. Epithelioid hemangioendothelioma: an overview and update on a rare vascular tumor. Oncol Rev. 2014;8(2):259. [PubMed ID: 25992243]. [PubMed Central ID: PMC4419652]. https://doi.org/10.4081/oncol.2014.259.
-
12.
Makhlouf HR, Ishak KG, Goodman ZD. Epithelioid hemangioendothelioma of the liver. Cancer. 1999;85(3):562-82. https://doi.org/10.1002/(sici)1097-0142(19990201)85:3<562::aid-cncr7>3.0.co;2-t.
