Abstract
Background:
In this study, we aimed to evaluate the accuracy of echocardiography compared to plain radiography in determining the appropriate line tip position of peripherally-inserted central catheters (PICC). Also, we aimed to evaluate the relationship between independent predictors (chronological age, birth weight, gestational age, and gender) and related complications with PICC line tip position.Methods:
In this prospective observational study, which was performed in the neonatal intensive care units of teaching hospitals affiliated with Iran University of Medical Sciences in 2019, 50 out of 96 neonates were non-randomly selected based on inclusion criteria. The radiographic and echocardiographic tests were simultaneously performed, and the data were analyzed.Results:
The findings of this study showed that there was an agreement between radiography and echocardiography in determining the PICC line tip position in 43 neonates (86%). The sensitivity and specificity of echocardiography in determining the ectopic position of the catheter were 81% and 77%, respectively. In 32 neonates (64%), a second radiograph prevented the following line manipulation using echocardiography. In addition, there was no significant relationship between independent predictors (chronological age, birth weight, gestational age, and gender) and PICC line complications.Conclusions:
The results of the present study showed that echocardiography was a useful tool for determining the position of the catheter’s tip in LBW neonates. It also minimizes radiation exposure on subsequent radiographs and obviates the need for additional radiographs following catheter manipulation by echocardiography.Keywords
Newborn Infant Peripheral Catheterization Echocardiography Sonography
1. Background
Vascular access is an important aspect of treatment in neonates. Central venous catheters, which are embedded in peripheral veins, have been considered for this purpose in recent years (1). Approximately 8 - 33% of the neonates admitted to the intensive care unit (ICU) need this type of catheter for receiving further care (2). Although radiography is the most common method for locating the catheter’s tip, it provides limited information on the correct position of the peripherally-inserted central catheters (PICC) (3). In addition, the confirmation of the position of the catheter’s tip using radiography has many disadvantages (4). Despite advances in antenatal care, premature births have increased in recent years, leading to a higher rate of hospitalization of premature neonates. In fact, access to venous routes for supplying nutrients, water, and electrolytes, as well as essential drugs, is a common challenge in neonatal intensive care units (NICUs) (1, 5). Due to the long-term hospitalization of premature neonates in ICUs, and the fact that it is not possible to use peripheral veins as vascular routes for a long time, it is important to find an alternative method to secure long-term access to intravenous routes (2). Concerns over the complications of central venous cannulation, including pneumothorax, arterial cavities, and poor patient acceptance, have led to the introduction of PICC catheters (i.e., central venous catheters) (6). The PICC is a thin, long catheter (14 - 16 inches long) made of either soft, flexible silicone or polyurethane. This catheter is usually inserted into large peripheral veins in the arm (the cephalic or basilic vein) or into the superior vena cava near the heart. Due to the long-term applicability of PICC catheters, this procedure can reduce the need for repeated needling of infants (7). The application of PICC in infants requires a specialized and privileged bedside operation without a need for surgical interventions. In addition, PICCs are associated with a lower risk of circulatory infections compared to non-tunnel catheters (8, 9). In recent years, ultrasound (USG)/echocardiography has been widely used to locate the catheter’s tip (10), which is important to prevent the migration or displacement of the catheter. Also, the incidence of catheter migration or catheter displacement, including slipping, extrusion, and thrusting, varies from 5% to 31% (11).
2. Objectives
Given the above-mentioned, we here aimed to evaluate the accuracy of echocardiography compared to plain radiography in determining the position of the PICC line’s tip in the infants admitted to the NICU. Also, we evaluated the relationship between independent predictors (chronological age, birth weight, gestational age, gender, and intubation status) and the PICC line’s tip position.
3. Methods
In this prospective observational study, out of 96 neonates, 50 cases admitted to the NICU in teaching hospitals affiliated with the Iran University of Medical Sciences in 2019 were studied. These neonates were non-randomly chosen by the convenient sampling method based on inclusion criteria. The neonates’ demographic information was recorded into a data collection form. For each neonate, the catheter placement process was simultaneously monitored through radiographic and echocardiographic examinations. Using SPSS, the results of these two processes were compared by the chi-square test, and in some cases, by the Fisher’s exact test. Also, the sensitivity and specificity of echocardiography were determined by comparing the results of the two tests.
Chest X-ray is the standard diagnostic method for confirming the position of the central venous catheter’s tip. The primary purpose of the present study was to compare the sensitivity and specificity of portable echocardiography with that of chest X-rays. Thus, we used a sonography machine with a variable-frequency 4- to 8-MHz curvilinear P10xp probe (SonoSite, Inc, Bothell, WA) and a scan depth of 15 cm. Because the primary aim of our study was to determine the sensitivity and specificity of echocardiography (and not a combination of echocardiography and ultrasound), we did not use a linear probe.
Non-random convenient sampling was performed considering inclusion and exclusion criteria. The data were collected by field study using a checklist. Hemodynamically stable infants admitted to the teaching hospitals affiliated with the Iran University of Medical Sciences, who were expected to need a venous line for more than a week, were included. Exclusion criteria were contraindications to PICC implantation such as coagulopathy, confirmed venous thrombosis, generalized skin disease, skin infections at the catheter insertion site, being transferred to a center other than the educational centers affiliated with the Iran University of Medical Sciences, chromosomal abnormalities, and the diagnosis of congenital diseases during hospitalization.
Chest X-ray-guided catheterization was performed on either the right or left vein. If it was required to be conducted on the right upper extremity, then one of the following three ideal positions were adapted to position the catheter’s tip during the procedure:
(1) The junction of SVC at the right atrium (up to 2 cm above the junction, and 1 cm inside the right atrium for preterm infants and 2 cm for term infants).
(2) and (3) The upper part of mid-SVC or through the innominate vein.
It is noteworthy that for left-sided catheters, the ideal tip position is at the caval-atrial junction, and the other two positions are inappropriate. Also, looping the catheter or positioning it through azygous, hemiazygos, internal jugular, or subclavian veins is inappropriate during the procedure.
The ideal target tip position at the lower extremity is the inferior vena cava-right atrial junction (outside the cardiac silhouette) in a region above the L2 vertebrae, with the tip of the catheter being visible. The appropriate position of the catheter’s tip based on echocardiography is defined as the positioning of the tip at the junction of the SVC and right atrium (up to 2 cm above the junction, 1 cm inside the right atrium in preterm infants, and 2 cm in term infants). When the tip is undetectable, its position can be estimated by rapidly injecting a bolus of saline through the distal lumen of the catheter, known as the bubble test. When micro-bubbles are evident in the right atrium within less than 2 seconds after the beginning of the injection, the test is considered positive, indicating an appropriate position of the catheter’s tip.
3.1. Ethical Considerations
The present study was approved by the institutional ethics committee. We also obtained informed consent and provided parents with complete information about their neonates’ conditions in this study. The principle of confidentiality was observed, and no additional costs were imposed on the patients’ families. There was no compulsion to participate in the study.
4. Results
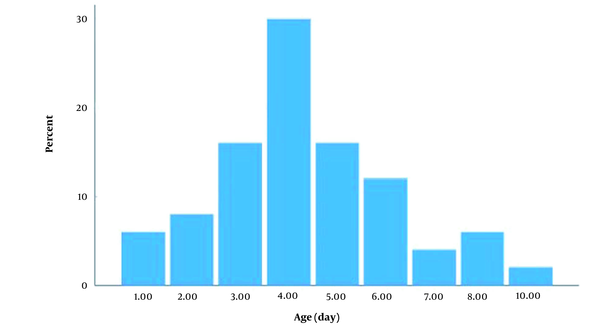
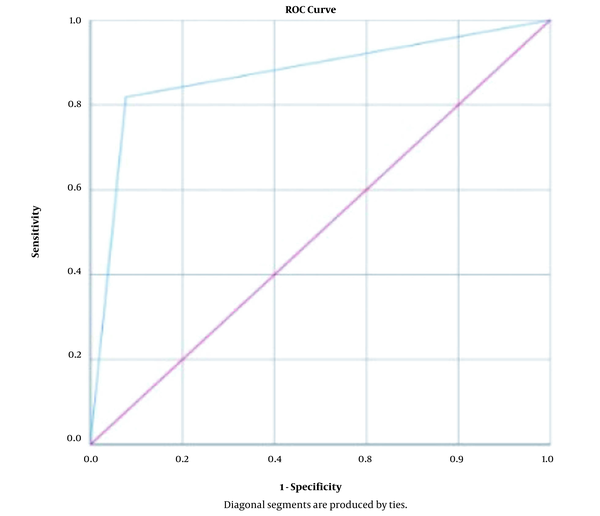
A total of 50 neonates with a mean age of 4.38 ± 1.9 days were examined in this study. According to Figure 1, A 16% of the neonates were evaluated on the third day, 30% on the fourth day, and 16% on the fifth day after birth. As shown in Table 1, in 86% of the neonates, the catheter’s location was in agreement with the prediction of echocardiography, and in 14%, the catheter’s location was not consistent with echocardiography. According to the ROC curve (Figure 2), in comparison with chest radiography, the sensitivity and specificity of echocardiography in determining the appropriate position of the PICC catheter in neonates were 81% and 77%, respectively.
Neonates’ age distribution (days)
The Catheter’s Location by Echocardiography
| Valid | No. (%) |
|---|---|
| Compatible to graph | 43 (86) |
| Not compatible with graph | 7 (14) |
| Total | 50 (100) |
ROC curve analysis
Five out of seven cases in whom the results of echocardiography and chest X-ray were inconsistent had an ideal tip position based on chest X-ray; however, the position of the tip of the catheter was rather unsuitable according to echocardiography. In three cases (one male and two females) in weeks 28, 34, and 35 of their gestational age, the tip of the catheter was found to be inserted through the oval foramen into the left atrium, which is regarded as an inappropriate position. As a result of catheter malalignment, two neonates in weeks 27 and 32 of their gestational age were diagnosed with tricuspid valve dysfunction.
In two cases, the position of the catheter was actually inappropriate, while based on echocardiography, it was in a suitable position. The diagnostic accuracy of echocardiography in determining the appropriate position of the PICC catheter in neonates was 100% on the first day, 75% on days 2nd, 3rd, and 5th, and 87.7% on day 4th. the worst accuracy was on 10th day (0%).
Also, the results of the chi-square test showed that there was no statistically significant relationship between the two variables. According to the results of the present study, the neonates’ weight, gestational age, and intubation status or mode were not significantly associated with the specificity and sensitivity of echocardiography. In 32 neonates (64%), echocardiography obviated the need for a second radiograph to determine the new location of PICC following manipulation of the catheter.
5. Discussion
Vascular access is an important aspect of neonatal treatment. Chest X-ray is the gold standard diagnostic method to confirm the position of the central venous catheter’s tip. The primary purpose of this study was to investigate the sensitivity and specificity of portable echocardiography compared to that of chest X-ray in identifying the correct position of the PICC catheter’s tip in the neonates admitted to NICU.
The improper position of the upper limbs relative to the trunk (adduction versus abduction or not performing the frog-leg position for lower extremities), crying, restlessness, and deep breathing of the baby can negatively affect the tip’s location during catheterization as monitored by chest X-ray.
For upper catheterization, shoulder abduction and elbow flexion will decrease the distance between the tip of the catheter and the heart while inserting the catheter into the basilic vein. When the catheter is inserted into the cephalic vein, abduction of the arm and flexion of the elbow cause it to move away or become closer to the heart, respectively (12). During echocardiography, these dynamic changes can be observed, and the inappropriate location of the catheter’s tip can be corrected if necessary in several respiratory and cardiac cycles.
In a 2012 study by Jain et al. (13) in Canada, the researchers focused on SVC and RA, which are the most common sites of PICC placement in preterm neonates and potentially have the widest margins of error. This study on 22 low birth-weight, preterm neonates showed that echocardiography and radiography findings were consistent in 59% of the cases, while 41% required a concurrent approach such as echocardiography in addition to radiography.
In other studies, the overall agreement between radiography and echocardiography for the position of the PICC line’s tip in neonates was reported to be 60 to 80%. In a study by Diemer three decades ago, the utility of ultrasound in the detection of the position of the silastic catheter’s tip was investigated in neonates, showing that ultrasound can reduce the need for radiography for positioning the catheter’s tip (14). In addition, Ohki et al. (15) recently provided further evidence that ultrasound was a useful and practical method for determining the position of the catheter’s tip in infants, reporting an agreement of 75% to 93% between ultrasound and radiography in determining the catheter tip’s position in SVC and RA, which was broadly different from that reported by Jain et al. (59%) (13). The discrepancy between the two methods can be attributed to the difficulty of accurately detecting the SVC/RA junction in radiography and the differences in physicians’ perceptions of this point. In Jain et al.’s study, ultrasound had an obvious advantage in accurately detecting the position of the tip rather than the SVC/RA junction (16). In addition, the position of the PICC tip varies depending on the position of the baby’s limbs.
In another study by Tauzin et al. (17) in France, which was published in 2013, out of 89 infants with PICC catheters, all had low birth weight. It was reported that the use of echocardiography increased diagnostic accuracy during PICC placement, and its use along with radiography was recommended to increase the accuracy of catheter placement (18).
In the present study, the catheter’s location was correctly determined by echocardiography in 86% of the neonates but not in 14% of the cases. Also, comparing echocardiography with chest radiography in terms of detecting the position of PICC in neonates based on ROC curve analysis, the sensitivity and specificity of echocardiography were obtained as 81% and 77%, respectively.
Five out of seven cases for whom the findings of echocardiography and chest X-ray were inconsistent showed an ideal tip position based on chest X-ray but an inappropriate position based on echocardiography. So, the catheter’s tip was repositioned to a suitable location. In many neonates, the first attempt to insert catheters often leads to mispositioning, requiring repositioning the catheter and reperforming X-ray radiography. Using echocardiography; however, increases the chance of appropriate positioning of catheters even in the first attempt.
In a prospective cohort study, Motz et al. (19) compared the validity and accuracy of ultrasound with that of radiography in identifying PICC mispositioning in neonates. They showed that out of 30 neonates (96.6% (n = 29) premature and 63.3% (n = 19) with a birth weight above 1500 gr), the results of ultrasound and radiography were consistent in 94 % (n = 28) of the cases. Also, in this study, the sensitivity was 0.97, and the specificity was 0.66, with a positive predictive value of 0.98. Ren et al. (20), in a 2-year retrospective analytical study, examined the performance of ultrasound in determining the position of the PICC’s tip in newborns and showed that out of 186 patients, PICC placement was successful in 174 (93.5%) cases. In 11 patients, the catheter’s tip was out of place (i.e., too deep in the right atrium in four patients, low-deep in four cases, and mispositioned in three patients). Moreover, the sensitivity and specificity of ultrasound in identifying the location of the PICC’s tip were 100%.
One of the most common complications of catheter placement is pneumothorax (PTX), which according to reports, comprises 30% of all mechanical side effects of PICC placement. The probability of occurrence of this complication varies between 1% and 6.6% (21). Two cases of pneumothorax were diagnosed in our study using chest X-ray, which could not be detected by echocardiography.
According to the results of the chi-square test, there was no statistically significant relationship between birth weight and the sensitivity and specificity of echocardiography in determining the appropriate position of PICC in neonates (P = 0.612), and the diagnostic accuracy of this method was found to be 100% for most birth weight groups. The birth weight has been shown to be an independent risk factor for complications, contributing to the success or failure of PICC placement (17). Using univariate and multiple logistic regression analyses, many studies have shown the role of independent predictors such as birth weight, gestational age, chronological age, and duration of PICC placement in the occurrence of complications and determining the appropriate position of PICC. Moreover, these variables have been reported to be associated with the risk of PICC-related complications and PICC positioning. The findings of some of these studies are consistent with our observations, yet some of them have reported different results from ours.
Li et al. (22) showed that premature neonates weighing more than 1,500 gr were less likely to develop PICC complications than neonates weighing less than 1,500 g. According to Hoffman et al., a high birth weight may also protect the baby from PICC-related complications (23).
Sengupta et al. (24) found that PICC complications had no significant association with gestational age, chronological age, and birth weight. The differences between the findings of previous studies and our observations appear to be due to differences in the quantitative mean of each of the independent predictor variables (including birth weight, gestational age, chronological age, gender, and PICC duration), as well as differences in the populations studied and sample sizes in each research.
In another study by Wen et al., gestational age and chronological age had no association with complications, while birth weight, as an independent variable, showed a significant relationship with the occurrence of complications (25). Neonates with a gestational age of lower than 32 weeks, chronological age of lower than seven days, and birth weight of less than 1,500 g were significantly more likely to develop PICC complications (14).
Regarding the diagnostic accuracy of echocardiography in determining the appropriate position of PICC in neonates based on gender, the diagnostic accuracy of this technique was found to be 73.9% in female infants and 77.8% in male infants. The results of Fisher’s exact test also showed that there was no statistically significant relationship between these two variables (P = 0.503).
Regarding the sensitivity and specificity of echocardiography in determining the appropriate position of PICC in neonates based on gestational age, the results showed that in 76% of the neonates, the catheter was placed in the correct position, and in 24% of cases, the catheter was misplaced. Based on the results obtained in this study, none of gestational age, intubation status, and the mode of ventilator had significant associations with the sensitivity and specificity of echocardiography.
5.1. Conclusions
This study highlighted the value of echocardiography as a useful tool for determining the position of the catheter’s tip in LBW infants, providing the possibility for real-time examination of the catheter’s position, minimizing exposure to radiation by obviating the need for obtaining secondary radiographs following catheter manipulation.
Acknowledgements
References
-
1.
Hosseini MB, Jodeiri B, Mahallei M, Abdoli-Oskooi S, Safari A, Salimi Z. [Early outcome of peripherally inserted central catheter versus peripheral IV line in very low birth weight neonates]. Feyz Journal of Kashan University of Medical Sciences. 2014;17(6):561-7. Persian.
-
2.
Pettit J, Mason-Wyckoff M. Peripherally Inserted Central Catheters: Guidelines for Practice. National Association of Neonatal Nurses: Glenview, IL. 1st ed. Chicago, USA: Glenview, IL; 2001.
-
3.
Fletcher SJ, Bodenham AR. Safe placement of central venous catheters: where should the tip of the catheter lie? Br J Anaesth. 2000;85(2):188-91. [PubMed ID: 10992821]. https://doi.org/10.1093/bja/85.2.188.
-
4.
Sneath N. Are supine chest and abdominal radiographs the best way to confirm PICC placement in neonates? Neonatal Netw. 2010;29(1):23-35. [PubMed ID: 20085874]. https://doi.org/10.1891/0730-0832.29.1.23.
-
5.
Haghighi Aski B, Manafi Anari A, Abolhasan Choobdar F, Zareh Mahmoudabadi R, Sakhaei M. Cardiac abnormalities due to multisystem inflammatory syndrome temporally associated with Covid-19 among children: A systematic review and meta-analysis. Int J Cardiol Heart Vasc. 2021;33:100764. [PubMed ID: 33778151]. [PubMed Central ID: PMC7983575]. https://doi.org/10.1016/j.ijcha.2021.100764.
-
6.
Safari S, Bastan Hagh E. [More familiarity with medical equipment Access to the central vein: Familiarity with the principles of catheterization]. II. Tehran, Iran: Farateb Jarrah; 2018. Persian.
-
7.
Njere I, Islam S, Parish D, Kuna J, Keshtgar AS. Outcome of peripherally inserted central venous catheters in surgical and medical neonates. J Pediatr Surg. 2011;46(5):946-50. [PubMed ID: 21616258]. https://doi.org/10.1016/j.jpedsurg.2011.02.037.
-
8.
Vilar AMA, de Oliveira MF, Mattos CM, Silvino ZR. [Interventional ultrasound for implantation and monitoring of peripherally inserted central venous catheter: scoping review]. Enfermagem Uerj. 2020;28. Portuguese.
-
9.
van den Hoogen A, Brouwer MJ, Gerards LJ, Fleer A, Krediet TG. Removal of percutaneously inserted central venous catheters in neonates is associated with the occurrence of sepsis. Acta Paediatr. 2008;97(9):1250-2. [PubMed ID: 18477060]. https://doi.org/10.1111/j.1651-2227.2008.00864.x.
-
10.
Barone G, Pittiruti M, Biasucci DG, Elisei D, Iacobone E, La Greca A, et al. Neo-ECHOTIP: A structured protocol for ultrasound-based tip navigation and tip location during placement of central venous access devices in neonates. J Vasc Access. 2021:11297298211007700. [PubMed ID: 33818191]. https://doi.org/10.1177/11297298211007703.
-
11.
Bertoglio S, Faccini B, Lalli L, Cafiero F, Bruzzi P. Peripherally inserted central catheters (PICCs) in cancer patients under chemotherapy: A prospective study on the incidence of complications and overall failures. J Surg Oncol. 2016;113(6):708-14. [PubMed ID: 27020965]. https://doi.org/10.1002/jso.24220.
-
12.
Connolly B, Amaral J, Walsh S, Temple M, Chait P, Stephens D. Influence of arm movement on central tip location of peripherally inserted central catheters (PICCs). Pediatr Radiol. 2006;36(8):845-50. [PubMed ID: 16758187]. https://doi.org/10.1007/s00247-006-0172-8.
-
13.
Jain A, McNamara PJ, Ng E, El-Khuffash A. The use of targeted neonatal echocardiography to confirm placement of peripherally inserted central catheters in neonates. Am J Perinatol. 2012;29(2):101-6. [PubMed ID: 22105438]. https://doi.org/10.1055/s-0031-1295649.
-
14.
Diemer A. Central venous silastic catheters in newborns: localization by sonography and radiology. Pediatr Radiol. 1987;17(1):15-7. [PubMed ID: 3822578]. https://doi.org/10.1007/BF02386588.
-
15.
Ohki Y, Maruyama K, Harigaya A, Kohno M, Arakawa H. Complications of peripherally inserted central venous catheter in Japanese neonatal intensive care units. Pediatr Int. 2013;55(2):185-9. [PubMed ID: 23253251]. https://doi.org/10.1111/ped.12033.
-
16.
Jain A, Deshpande P, Shah P. Peripherally inserted central catheter tip position and risk of associated complications in neonates. J Perinatol. 2013;33(4):307-12. [PubMed ID: 22955288]. https://doi.org/10.1038/jp.2012.112.
-
17.
Tauzin L, Sigur N, Joubert C, Parra J, Hassid S, Moulies ME. Echocardiography allows more accurate placement of peripherally inserted central catheters in low birthweight infants. Acta Paediatr. 2013;102(7):703-6. [PubMed ID: 23551125]. https://doi.org/10.1111/apa.12245.
-
18.
Kennedy Blandford K. Peripherally Inserted Central Catheter Placement Verification Using Electrocardiogram Technology. Virginia, USA: University of Virginia; 2017.
-
19.
Motz P, Von Saint Andre Von Arnim A, Iyer RS, Chabra S, Likes M, Dighe M. Point-of-care ultrasound for peripherally inserted central catheter monitoring: a pilot study. J Perinat Med. 2019;47(9):991-6. [PubMed ID: 31605580]. https://doi.org/10.1515/jpm-2019-0198.
-
20.
Ren XL, Li HL, Liu J, Chen YJ, Wang M, Qiu RX. Ultrasound to Localize the Peripherally Inserted Central Catheter Tip Position in Newborn Infants. Am J Perinatol. 2021;38(2):122-5. [PubMed ID: 31412404]. https://doi.org/10.1055/s-0039-1694760.
-
21.
Spiliotis J, Kordossis T, Kalfarentzos F. The incidence of delayed pneumothorax as a complication of subclavian vein catheterisation. Br J Clin Pract. 1992;46(3):171-2. [PubMed ID: 1286015].
-
22.
Li R, Cao X, Shi T, Xiong L. Application of peripherally inserted central catheters in critically ill newborns experience from a neonatal intensive care unit. Medicine (Baltimore). 2019;98(32). e15837. [PubMed ID: 31393341]. [PubMed Central ID: PMC6709114]. https://doi.org/10.1097/MD.0000000000015837.
-
23.
Hoffman MA, Snowden JN, Simonsen KA, Nenninger TM, Lyden ER, Anderson-Berry AL. Neonatal late-onset sepsis following peripherally inserted central catheter removal: association with antibiotic use and adverse line events. J Infus Nurs. 2015;38(2):129-34. [PubMed ID: 25723835]. https://doi.org/10.1097/NAN.0000000000000096.
-
24.
Sengupta A, Lehmann C, Diener-West M, Perl TM, Milstone AM. Catheter duration and risk of CLA-BSI in neonates with PICCs. Pediatrics. 2010;125(4):648-53. [PubMed ID: 20231192]. [PubMed Central ID: PMC4492110]. https://doi.org/10.1542/peds.2009-2559.
-
25.
Wen J, Yu Q, Chen H, Chen N, Huang S, Cai W. Peripherally inserted central venous catheter-associated complications exert negative effects on body weight gain in neonatal intensive care units. Asia Pac J Clin Nutr. 2017;26(1):1-5. [PubMed ID: 28049254]. https://doi.org/10.6133/apjcn.112015.07.
