Abstract
Introduction:
Primary pulmonary hypertension (PPH) is an uncommon disease in children. This pulmonary vascular disease may be idiopathic, familial or a kind of hereditary systemic vasculopathy. Multisystemic vascular diseases in children are rare and may be under-recognized. A few reports have described the involvement of cerebral vessels such as moyamoya disease (MD) in patients with PPH. MD is a unique cerebrovasculopathy, characterized by occlusion of the internal carotid arteries.Case Presentation:
We reported a 2-year-old boy with PPH, who presented unusual and intractable seizure which suggested the diagnosis of MD. We also reviewed a few previous reports about the association of PPH with moyamoya disease.Discussion:
Moyamoya disease is a kind of cerebral vasculopathy and should be considered as a differential diagnosis for patients with unusual seizure attacks who are suffering from primary pulmonary hypertension.Keywords
1. Introduction
Pulmonary hypertension has been defined as an increase in mean pulmonary arterial pressure which is greater than or equal to 25 mmHg at rest as assessed by right heart catheterization (1). Pulmonary hypertension is associated with pre-capillary obstruction of the pulmonary vascular bed as a result of hyperplasia of the muscular and elastic tissue and a thickened intima of the small pulmonary arteries and arterioles. The most recent clinical classification (Revised WHO classification of pulmonary hypertension) defines five pulmonary hypertension groups with pulmonary arterial hypertension (PAH) as group 1. PAH can be idiopathic, familial, or associated with conditions such as congenital heart disease and can occur at any age (2). The presence of PAH with a normal pulmonary capillary wedge pressure is the diagnostic of primary PAH. At least 6% of individuals diagnosed with PPH have a family history of the disorder. Mutation in the gene for bone morphogenetic protein receptor-2 (BMPR-2) on chromosome 2q33 has been detected in at least 60% of the families studied to date (3). PPH is characterized by pulmonary vascular obstructive disease and right-sided hear loss. The progression of PPH is usually rapid in children as compared to adults and the mean survival is 2-3 years after diagnosis. Life-threatening arrhythmia may result in sudden death in some of these patients (4).
MD is a kind of cerebral vascular disease with unknown etiology. The principal feature of this disorder is progressive stenosis in terminal segments of internal carotid arteries and its main branches. The above pathology results in a compensatory collateral network at the base of skull or circle of Willis. For the first time in 1969, Suzuki and Takaku noticed that the appearance of this collateral network in cerebral angiography is similar to a puff of smoke; so they called it moyamoya (4). The peak incidence of disease in childhood is at 5 years of age, and in adults it is at the forth decade of life. The female/male ratio is reported to be 2/1. Eighty percent of children suffering from this disease present frequent episodes of stroke or transient ischemic attacks. Signs are usually exasperated by hyperventilation; such as crying, coughing, or straining. Other atypical signs comprise syncope, paraparesis, visual disturbances, and involuntary movements. Microthrombi formation in stenotic vessels results in endothelial damage, intimal thickness, and proliferation of smooth muscles. In 15% of patients, the disease had been occurred in other members of family. No effective medical therapy is applicable to treat children with MD. Treatment is largely based on surgical renovascularization procedures (5).
Extracranial vascular involvement especially of renal arteries has been reported in MD. Involvements of other arteries such as pulmonary, coronary, and pancreatic arteries have also been found in this disorder. The ratio of intima/media thickness in extracranial arteries has been substantially increased. It is suggested that a systemic vascular disease such as fibromuscular dysplasia is the causative factor for MD and its extracranial manifestations. Progressive stenosis of internal carotid arteries in fibromuscular dysplasia can produce a cerebral angiographic view similar to the one seen in MD. Histopathologic findings in fibromuscular dysplasia have great similarity to those findings in MD (6). We present a child who suffered from a systemic vasculopathy. The patient showed the manifestations of PPH in addition to intractable and unusual seizure suggestive of moyamoya disease.
2. Case Presentation
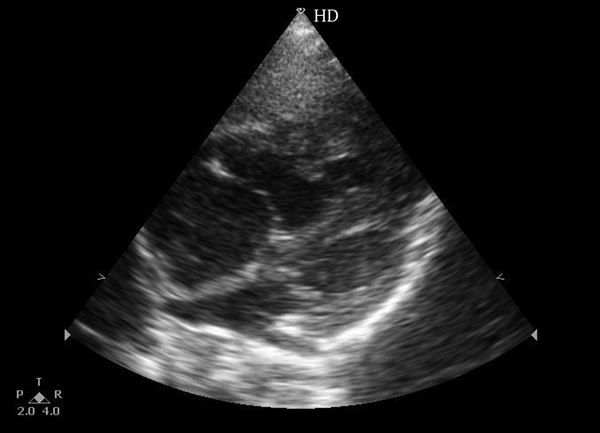
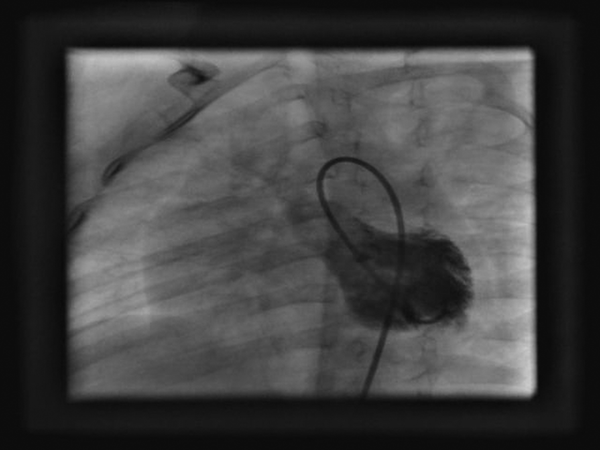
A 2-year-old boy was admitted to pediatric-cardiology ward of Modarres hospital to be evaluated for heart disease. He was supposed to be suffering from heart disease as an underling reason for his intractable seizure. The patient had frequent episodes of seizure since 14 months of age. The episodes usually provoked by crying or fatigue. Seizure occurred as paroxysmal attacks of paleness, weakness, eye deviation, and involuntary movements of extremities. Sometimes it occurred as nocturnal paroxysm, and sometimes there were several attacks per day. Duration of seizure was several seconds to 1-2 minutes. The EEG was reported normal, brain MRI without contrast was reported unremarkable, and there was no response to different combination of anticonvalescent drugs. The patient was the second child of family, and was the product of an uneventful full term pregnancy. The patient was born by repeat C-section delivery without birth asphyxia. There was no previous history of jaundice or sepsis during the neonatal period. Parents were first degree cousins, and their first child was a girl who died at 1.5 years of age with similar symptoms. On physical examination, general condition was good. Weight was 12 Kg, and development was normal. There was no syndromic facies, and no extra cardiac malformation. The child was acyanotic. Cardiac auscultation revealed a grade 2/6 systolic murmur at subxiphoid area with loud second heart sound. Femoral pulse was normal, and there was not clubbing at nail beds. Physical examination of other organs was unremarkable. Hematological, immunological, metabolic, and coagulation tests revealed no abnormalities. Hepatitis B antigen, Hepatitis C antibody and HIV antibody were negative. Electrocardiogram showed sinus rhythm, right axis deviation, and right ventricular hypertrophy. Chest X-ray showed moderate cardiomegaly, large right atrium, large right ventricle, prominent pulmonary artery segment, and normal pulmonary vascular marking. Echocardiography revealed normal segmental connection, large right atrium and right ventricle, dilated pulmonary artery, and tricuspid regurgitation of 70 mmHg (Figure 1). No anatomic abnormality was detected. Ejection fraction was 56%. 24-hour Holter monitoring showed no evidence of dysrhythmia during the episodes of seizure. Catheterization and angiography study were performed for patient. The courses of venous and arterial catheters were normal. Saturation of right and left heart chambers were within normal ranges. No shunt or systemic desaturation was detected. Pressures of right heart chambers were as follows: right atrium =7 mmHg, right ventricle = 80/7 - 10 mmHg, pulmonary artery = 80/45 (mean = 60 mmHg), pulmonary artery wedge = 10 mmHg. Pressures of left heart chambers were as follows: left ventricle = 90/8 mmHg, aorta = 90/60 (mean 70 mmHg). Calculation showed Qp/Qs of 1, and Rp/Rs of 0.8 units. Angiocardiography showed no structural abnormality of heart (Figures 2 and 3). Diagnosis of severe pulmonary hypertension was established for patient. According to WHO classification of pulmonary hypertension, this was a primary and most probably familial pulmonary hypertension. Treatment with digoxin, diuretic, and sildenafil was started with no significant effect.
Echocardiography sub Costal View Shows Large Right Atrium and Right Ventricle With Intact Ventricular and Atrial Septum
Angiographic View Demonstrates Filling of Left Ventricle With Intact Ventricular Septum and Lack of VSD
Angiographic View Demonstrates Normal Aortic Arch With no Evidence of Patent Ductus Arteriosus

The seizure attack of the patient was defined as anoxic seizure by pediatric neurologist. Under this heading, there are several entities including, drowning, near drowning, apnea, hypoxic spell, sleep apnea disorders, and moyamoya disease. All the differential diagnoses had been rolled out except for moyamoya disease. The provocation of seizure by crying, weakness, eye deviation, involuntary movement of extremities, normal EEG, previous history in other sibling, Parental consanguinity, Asian ethnicity, and unresponsiveness to medical therapy, were compatible with moyamoya disease. Cerebral angiography was recommended for patient, and diagnosis was discussed with parents. They decided to discharge the patient against medical advice. One month after discharge the patient died in home during one of the episodes of seizure.
3. Discussion
Pediatric pulmonary hypertension is an important cause of morbidity and mortality. The Tracking Outcomes and Practice in Pediatric Pulmonary Hypertension (TOPP) registry is a global prospective study. According to a recent survey (2012) by TOPP, out of 362 consecutive patient with confirmed diagnosis of PH, 317 (88%) had PAH, which was idiopathic or familial in 182 (57%), and associated with other disorders in 135 (43%), of which 115 (85%) cases were associated with congenital heart disease. Median age at diagnosis was 7 years (3 to 12 years), and 59% were female. Functional class was 1 or 11 in 230 of 362 (64%) patients, which is consistent with preserved right-heart function. This pediatric profile, suggestive of a preserved cardiac performance despite severe PH, could change as children grow into adults. The most frequently reported adulthood symptoms at presentation were dyspnea on exertion and fatigue. Syncope was reported in 25% of patients (7). In a retrospective analysis by Calderon Colmenero et al., 18 patients under two years of age who suffered from PPH were evaluated. In 13 patients diagnosis was made before the first year of life and in 8 of them diagnosis was made in the neonatal period. Cardiac catheterization showed a mean pulmonary systolic arterial pressure of 64.4 mmHg. Five patients (27%) died two months after the diagnosis was made and three months after the onset of symptoms. Four of them died due to CHF and one had sudden death. This study shows the early onset of the disease as well as its short-term high-rate mortality (8). The progression of PPH is usually rapid in children as compared to adults and the mean survival is 2 to 3 years after the diagnosis is made. Life threatening arrhythmia may result in sudden death in some of these patients (4). Cardiopulmonary resuscitation for circulatory arrest in patients with PAH is rarely successful (9). In our patient pulmonary artery pressure was near systemic pressure, and mean PA pressure of 60 mmHg was compatible with severe PAH. The normal wedge pressure and lack of anatomical defects were compatible with PPH.
Moyamoya disease is a chronic and slowly progressive occlusive cerebral vasculopathy of unknown etiology. In a report by Kim et al. (2012), seizure was observed in 27% of 64 patients as an initial symptom. In the patients with focal seizure, eye-ball deviation, head or/and mouth deviation, and secondary generalization were observed. Isolated seizures were more frequent in infancy (60%) and toddlerhood/preschool age children. Loss of consciousness was observed in 5% of children as an initial symptom. Crying and anger were the most common provoking events which were followed by eating food. Symptoms occurred during sleep or upon awakening from sleep. Seventy percent of all 64 patients became symptomatic at 3 to 8 years of age (10). moyamoya disease is relatively common in Asia, particularly in Japan and Korea, although the global incidence of MD is not high (10). Patients most frequently present transient ischemic attacks or cerebral infarcts. Headaches, seizures, hemorrhages, epilepsy, and mental retardation can also occur (6). In some cases similar angiographic features are evident in children with other medical conditions, such as sickle cell disease and Down syndrome. In these instances, the term “moyamoya syndrome” is used (5).
Multisystemic vascular diseases in children are rare and may be under-recognized. Kapusta et al. for the first time on 1990 described a child with moyamoya disease and primary pulmonary hypertension. This association had never been reported until that time. they were attempting to consider a common vascular pathology for both diseases although they were not able to prove the hypothesis (11). De Vries et al. (2003), reported two children with moyamoya and extra cranial vascular involvement. In their report, the first child was a boy who experienced paroxysmal nocturnal episodes of paleness, yawning, and perspiration since age 2. At the age of 7 he began to complain of episodic headache and vomiting. Cerebral angiography revealed severe bilateral stenosis in terminal portion of carotid arteries accompanied with extensive collateral network. Three years later he presented dizziness, palpitation, paleness, and fainting during exercise. ECG and echocardiographic findings were suggestive of right ventricular hypertrophy and pulmonary hypertension. The patient died due to severe hemorrhage during balloon dilatation of pulmonary arteries. Postmortem examination showed tearing of pulmonary artery at the upper lobe of right lung. Histopathologic findings were indicative of intimal fibroplasias. The second child was a boy who had been admitted in the hospital due to progressive left hemiparesis at the age of two. After admission he had lost his consciousness and showed the paroxysmal attacks of smacking, eye deviation, and severe bilateral pyramidal signs. There had been no epileptic evidence in EEG. Cerebral angiography had demonstrated bilateral stenosis of internal carotid arteries accompanied with typical puff of smoke appearance of collateral network. Diagnosis of MD had been proposed and aspirin had been administrated with good results. Five years later the patient was admitted in hospital because of aphasia, right-sided facial palsy, and gaze paralysis. Cerebral angiography showed extension of collateral network. The patient started complaining of abdominal pain. Abdominal angiography showed occlusion of the celiac trunk and superior mesenteric artery. The diagnosis of fibromuscular dysplasia was made. He did not develop hypertension (6).
Ou et al. on 2006 reported the first case, to the best of their knowledge, a child with the unusual association of moyamoya disease and both systemic and pulmonary hypertension. Histological examination revealed fibromuscular dysplasia as the common designation for a diffuse arteriopathy (12). Klein et al. on 2007 reported 2 patients. They were 2 sisters presenting with encephalitis-like symptoms in infancy. They were supposed to be suffering from metabolic disease. Many years after neurologic symptoms, the patients exhibited pulmonary hypertension and renovascular hypertension. Further investigations led to diagnosis of systemic vasculopathy. The reporters recommended that these two sisters were afflicted with intracranial vasculopathy of internal carotid arteries and at the first year of life showed transient ischemic cerebral attacks. During the course of MD, involvement of extracranial arteries may be extensive and should always be investigated. There might be some kinds of treatments for these types of implications (13).
Day et al. on 2010 introduced a 7-year-old girl with Down syndrome. She suffered from severe pulmonary hypertension and was receiving calcium channel blocker agents. She showed signs and symptoms of transient ischemic attacks or stroke during the course of treatment. Cerebral angiography demonstrated bilateral stenosis in supraclinoid segments of internal carotid arteries, stenosis and occlusion at the proximal segments of anterior and middle cerebral arteries, and occlusion of left posterior cerebral artery. The patient underwent surgery for improving the circulation of damaged areas of brain. Medical treatment of pulmonary hypertension was changed to oral endothelin receptor antagonist (Bosentan). This experience identified that bosentan can be used safely in patients with MD. Other researches are required to display the efficacy of endothelin receptor antagonist in improving the cerebral blood flow after surgical operation (14).
When the child was admitted into our ward, there was no diagnosis for his illness. Our aim at the time of patient’s catheterization was diagnosing his heart disease. After confirmation of PPH as underlying heart disease, we made an extensive review of literature to find the correlation between neurologic and cardiovascular symptoms of the patient. By ruling out all other differential diagnoses, we reached to diagnosis of moyamoya disease. We wanted to perform MR angiography, but parents did not give their consent. We had many data in favor of a genetic multisystem arteriopathy .Consanguinity of parents, family history of a sibling, Asian ethnicity, unusual seizure with normal EEG and resistance to treatment, rapid progressive course of pulmonary hypertension in the absence of congenital heart disease, and death in early life were compatible with moyamoya disease and PPH. He needed cerebral angiography, but parents discharged the child against medical advice. To the best of our knowledge this is a case of moyamoya disease with PPH that has been reported in Iran, and possibly this is the 8th case in English literature.
In conclusion, moyamoya disease is a kind of systemic vasculopathy and should be considered as a differential diagnosis in children with intractable unusual seizure accompanied with signs and symptoms of pulmonary or systemic hypertension.
Acknowledgements
References
-
1.
Galie N, Hoeper MM, Humbert M, Torbicki A, Vachiery JL, Barbera JA, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J. 2009;34(6):1219-63. [PubMed ID: 19749199]. https://doi.org/10.1183/09031936.00139009.
-
2.
Bernstein D. Primary pulmonary hypertension. In: Kliegman R, Stanton B, St. Gene J, Schor N, Behrman R, editors. Nelson textbook of pediatrics. 19 ed. Philadelphia: Elsevier; 2011. p. 1600-1601.
-
3.
Sztrymf B, Yaici A, Jais X, Sitbon O, Simonneau G, Humbert M. Idiopathic pulmonary hypertension: what did we learn from genes? Sarcoidosis Vasc Diffuse Lung Dis. 2005;22 Suppl 1:S91-100. [PubMed ID: 16457021].
-
4.
Krishnan U. Diagnosis and management of primary pulmonary hypertension. Indian J Pediatr. 2000;67(3 Suppl):S41-5. [PubMed ID: 11129920].
-
5.
Currie S, Raghavan A, Batty R, Connolly DJ, Griffiths PD. Childhood moyamoya disease and moyamoya syndrome: a pictorial review. Pediatr Neurol. 2011;44(6):401-13. [PubMed ID: 21555050]. https://doi.org/10.1016/j.pediatrneurol.2011.02.007.
-
6.
de Vries RR, Nikkels PG, van der Laag J, Broere G, Braun KP. Moyamoya and extracranial vascular involvement: fibromuscular dysplasia? A report of two children. Neuropediatrics. 2003;34(6):318-21. [PubMed ID: 14681758]. https://doi.org/10.1055/s-2003-44664.
-
7.
Berger RM, Beghetti M, Humpl T, Raskob GE, Ivy DD, Jing ZC, et al. Clinical features of paediatric pulmonary hypertension: a registry study. Lancet. 2012;379(9815):537-46. [PubMed ID: 22240409]. https://doi.org/10.1016/S0140-6736(11)61621-8.
-
8.
Calderon Colmenero J, Rylaarsdam M, Camacho L, Attie F, Zabal C, Buendia A. [Primary pulmonary arterial hypertension in children under 2 years of age]. Arch Inst Cardiol Mex. 1991;61(6):533-7. [PubMed ID: 1793305].
-
9.
Hoeper MM, Galie N, Murali S, Olschewski H, Rubenfire M, Robbins IM, et al. Outcome after cardiopulmonary resuscitation in patients with pulmonary arterial hypertension. Am J Respir Crit Care Med. 2002;165(3):341-4. [PubMed ID: 11818318]. https://doi.org/10.1164/ajrccm.165.3.200109-0130c.
-
10.
Kim YO, Joo SP, Seo BR, Rho YI, Yoon W, Woo YJ. Early clinical characteristics according to developmental stage in children with definite moyamoya disease. Brain Dev. 2013;35(6):569-74. [PubMed ID: 22951249]. https://doi.org/10.1016/j.braindev.2012.08.001.
-
11.
Kapusta L, Daniels O, Renier WO. Moya-Moya syndrome and primary pulmonary hypertension in childhood. Neuropediatrics. 1990;21(3):162-3. [PubMed ID: 2234323]. https://doi.org/10.1055/s-2008-1071486.
-
12.
Ou P, Dupont P, Bonnet D. Fibromuscular dysplasia as the substrate for systemic and pulmonary hypertension in the setting of Moya-Moya disease. Cardiol Young. 2006;16(5):495-7. [PubMed ID: 16984702]. https://doi.org/10.1017/S104795110600045X.
-
13.
Klein A, Fasnacht M, Huisman TA, Neuhaus TJ, Martin E, Boltshauser E. Siblings with infantile cerebral stroke and delayed multivessel involvement--a new hereditary vasculopathy? Eur J Paediatr Neurol. 2007;11(5):292-6. [PubMed ID: 17428710]. https://doi.org/10.1016/j.ejpn.2007.02.007.
-
14.
Day RW, Brockmeyer DL, Feola GP. Safe treatment of pulmonary hypertension with bosentan in a patient with moyamoya disease and cerebral ischemia. J Child Neurol. 2010;25(4):504-7. [PubMed ID: 19808994]. https://doi.org/10.1177/0883073809339360.