Abstract
Background:
Kawasaki Disease (KD) is an acute febrile vasculitis of early childhood and the leading cause of acquired heart disease in children. The most important complication of KD is coronary artery aneurysm that may lead to thrombosis and myocardial infarction, occurring in 25% of untreated cases. Fortunately, timely treatment decreases it to 2 - 4%. There is no specific test for the diagnosis of KD, which is entirely based on clinical and laboratory criteria.Objectives:
Since KD is very common in Iran and other Asian countries, it is necessary to get a clear picture on the frequency of KD related anomalies in the clinical and laboratory findings as well as the frequency of coronary aneurysms in our region.Patients and Methods:
We retrospectively studied the medical records of all children discharged from the Besat Hospital, Hamedan, Iran, with a final diagnosis of KD, from 2004 to 2013. Outpatient documents were also studied. Demographic data, clinical features, laboratory and echocardiographic findings were also recorded onto the forms.Results:
Seventy four patients, 43 (58.1%) males and 31 (41.9%) females, were discharged with a final diagnosis of KD, 77% of which were less than 5 years old. No seasonal variability was noticed in the study population. Among all cases, 44 (59.5%) were diagnosed as complete and 30 (40.5%) as incomplete KD. Conjunctivitis, considered as the most common clinical finding, occurred in 79% of patients, whereas peripheral erythema was the least common, corresponding to 23% of cases. Finger desquamation and leukocytosis occurred in 54% and 49.3% of cases, respectively. Amongst the timely-treated patients, 11 (14,8%) developed coronary artery aneurysm.Conclusions:
Sex, age, and seasonal patterns of KD in Hamedan Province, IR Iran, are similar to other regions. However, finger desquamation is less prevalent, diminishing its value as a measure for patients’ follow up. The most common supplementary laboratory criteria were leukocytosis, thrombocytosis and anemia, which were determined by a complete blood count. Coronary artery aneurysm in timely-treated patients was far more common compared to other studies, which may indicate the need for revising the golden time for initiating the treatment.Keywords
Mucocutaneous Lymph Node Syndrome Children Coronary Aneurysm Vasculitis Iran
1. Background
Kawasaki disease (KD) is a febrile vasculitis that was first described in 1967 in Japan. The etiology of KD is unknown, although the clinical and epidemiological evidences support the role of an infective agent. Nowadays, KD is considered as the most common cause of acquired heart disease in children in many countries, surpassing the acute rheumatic fever. The KD has a worldwide distribution, but is more common in Asian countries (1). The incidence of the disease varies in different parts of the world, as it is 17, 66, and 137 in every 100000 children less than 5 years old in USA, Taiwan and Japan, respectively. Its incidence has increased in recent years (1-3). The KD is an illness of early childhood, as 80% of patients are less than 5 years-old, although adolescents and adults may also be affected.
There is no specific diagnostic test. Therefore, the diagnosis of KD is based on the following clinical criteria: presence of fever for 5 days or more and at least four of the five principal clinical criteria including bilateral conjunctivitis, mucosal changes, changes in extremities, rashes and cervical lymphadenopathy (1).
Other clinical findings that are not included in the diagnostic criteria are arthritis, diarrhea and erythema at the site of previous bacillus Calmette-Guérin (BCG) vaccination. Laboratory findings include: elevated C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) (in almost all of the cases), anemia, leukocytosis, thrombocytosis, sterile pyuria, decreased albumin levels and mild increase of the hepatic enzymes (1, 2, 4).
Cardiac involvement is the most important manifestation of KD and diagnosis is usually based on echocardiographic findings (5). However, the most important presentation is coronary artery aneurism, which occurs in almost 25% of untreated cases in the 2nd to 3rd week of disease and may lead to arterial thrombosis, arterial stenosis, myocardial infarction, coronary aneurysm rupture and even sudden death (1). With an appropriate treatment, the risk for coronary artery aneurysms decreases to 2 - 4% (1).
There are patients who do not fulfill the KD diagnostic criteria. However, they are still at risk for cardiac complications. Based on the defined diagnostic criteria, these cases are considered as “incomplete KD” and represent an indication for prompt initiation of the appropriate treatment (4).
2. Objectives
Studies show that the epidemiological characteristics vary in different regions of the world (1-3). Since KD is very common in Iran as in other Asian countries and its diagnosis is based on clinical criteria having no specific test, it is necessary to acquire precise information about the clinical and laboratory findings in our country. To determine whether there are differences among regions, it is necessary to study cases from different parts of the country. Therefore, the aim of this study was to assess the frequency of each clinical and laboratory finding and to survey the demographic features of KD as well as its outcomes and potentially-prognostic factors in our region.
3. Patients and Methods
As the Besat Hospital, Hamedan, Iran is the only pediatric infection and cardiology center in the Hamedan province and almost all children suspected with KD are referred there, we retrospectively studied the medical records of all children discharged from the Besat Hospital with a final diagnosis of KD from 2004 to 2013. Follow up data were also retrieved from the patients’ records. Demographic data, clinical features, and laboratory and echocardiographic findings were included in the assessment forms. This study was approved by the Ethics Committee of The Hamedan University of Medical Sciences, Hamedan, IR Iran.
Diagnosis of complete KD was made based on the clinical criteria: presence of fever for 5 days or more and at least four of the five principal clinical criteria: 1) bilateral, nonexudative bulbar conjunctivitis, 2) mucosal changes (pharyngeal injection, strawberry tongue, injected lips and dry fissured lips), 3) changes in extremities (peripheral edema, peripheral erythema and desquamation), 4) rash (maculopapular rashes, hives, erythema multiform) and 5) cervical lymphadenopathy >1.5 cm in diameter (usually unilateral).
For incomplete KD, the diagnostic criteria were: fever ≥ 5 days (not explainable by other causes) in the presence of at least two of the principal clinical criteria, in the setting of elevated ESR and/or CRP (ESR > 40 mm/h, CRP ≥ 30 mg/dL) and abnormal echocardiographic findings, or three supplementary laboratory criteria (3). The supplementary laboratory criteria included albumin < 3.0 g/dL, age-related anemia, elevation of alanine aminotransferase (ALT), platelet count > 450,000/mm3 after 7 days, white blood cell count (WBC) > 15,000/mm3, and urine WBC > 10/high-power field (1).
The software package used for data analysis was the SPSS version 16.0 (SPSS, Chicago, Illinois, USA). Statistical significance was noted for P ≤ 0.05. For finding the association between the qualitative variables, Chi-Square test was used, while independent sample t-test was applied for comparison of quantitative variables.
4. Results
In the present study, among the 74 patients discharged from the Besat Hospital with a final diagnosis of KD from 2004 to 2013, 31 (41.9%) were female and 43 (58.1%) were male, 49 (66.2%) were from urban and 25 (33.7%) were from rural areas, 16 (21.6%) were admitted in spring, 18 (24.3) in summer, 20 (27.0%) in fall and 20 (27.0%) in winter. Age distribution of patients is shown in Table 1.
Age Distribution of Patients With KD
| Age, mo | No. (%) |
|---|---|
| < 12 | 11 (14.8) |
| 13 - 24 | 16 (21.6) |
| 25 - 36 | 13 (17.5) |
| 37 - 48 | 12 (16.2) |
| 49 - 60 | 5 (6.7) |
| 61 - 72 | 5 (6.7) |
| 73 - 84 | 4 (5.4) |
| 85 - 96 | 3 (4.0) |
| > 96 | 5 (6.7) |
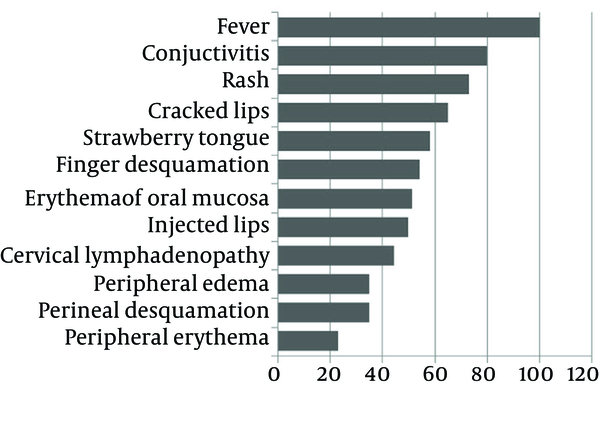
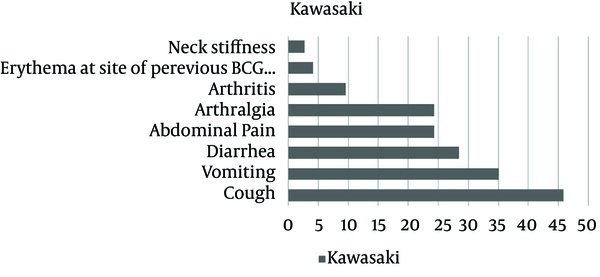
Among all patients, 44 (59.5%) were diagnosed with complete and 30 (40.5%) with incomplete KD. The frequency of each principal clinical finding is shown in Figure 1, and the other symptoms in Figure 2. Only 4 (5.4%) of the 74 patients were found with transverse lines on fingernails (Beau’s lines).
The Frequency of Principal Clinical Findings in Patients With KD
The Frequency of Associated Clinical Findings in Patients With KD
The frequencies of the supplementary laboratory criteria were also studied. Leukocytosis was found in 36 (48.6%), thrombocytosis in 32 (43.2%), anemia in 28 (37.8%), sterile pyuria in 15 (20.2%), increased ALT in 9 (12.1%), and hypoalbuminemia in 4 (5.4%) cases. We also compared the frequencies between patients with complete and incomplete KD. The results are shown in Table 2.
The Frequency of Supplementary Laboratory Criteria in Patients With Complete and Incomplete KD
According to the echocardiographic findings, 17 (22.9%) cases were diagnosed with coronary artery abnormalities, of which six (8.1%) had complete and 11 (14.8%) incomplete KD. Out of 17 coronary involvements, four (5.4%) accounted for coronary wall irregularities and 13 (17.5%) for aneurysms. Given that two patients referred after the acute phase of the disease, in timely-treated patients, only 11 (14.8%) were complicated with coronary aneurysm. With respect to the treatment, all 74 patients received intravenous immunoglobulin (IVIG). Only 9 (12.1%) cases required repetitive doses of IVIG, while two others (2.7%) received methylprednisolone.
Due to the importance of the coronary involvement, we also studied the relationships between its underlying factors as well as between the clinical and laboratory findings. Results showed that coronary artery involvement is not significantly different with the variation of age, gender, and clinical and laboratory findings. Nevertheless, it was significantly more frequent in patients with incomplete KD (P = 0.028).
In addition, prolonged fever was considered to be a risk factor for coronary aneurysms in other studies. In our study, there was no significant relationship between the duration of fever and coronary artery aneurysm. The considerable point is that if only echocardiography performed in acute phase of the disease was included in our study, there would be a significant difference between the coronary artery involvement and conjunctivitis, injected lips, and oral mucosa erythema (P < 0.05).
5. Discussion
Our study showed that the incidence of KD in the Hamedan province was somewhat higher in males compared to females, similar to other national and international studies (1, 2, 6-9). There was no significant seasonal variability. According to Table 1, 77% of patients were less than 5 years old, a finding in accordance to the other reports (1).
Among the principal clinical criteria, except for fever, which was presented in all patients, the most common findings were conjunctivitis, rashes, and changes of the oral cavity and tongue, respectively, which that are similar to as reported by previous studies (1, 10). Peripheral erythema was the rarest finding. Cervical adenopathy was found in more than 40% of cases, which was consistent with the findings of Saket et al. study in the Mofid Hospital of Tehran, IR Iran, as well as pediatric medical center study, even though it is considered as the rarest main symptom in many references and is reported in less than 30% of cases (9, 11).
Finger desquamation in the sub-acute phase of the illness was reported in more than 90% of cases in literature. Consequently, the American Heart Association (AHA) recommends performing echocardiography in patients who do not fulfill the complete criteria for KD in the acute phase of the disease, but present finger desquamation in the sub-acute phase (1, 3). In the present study, finger desquamation was only found in almost half of the patients during the follow up visits. This was consistent with similar reports in Iran, as it was described in almost 30% of patients in the researches of Yazd and Bandarabbas provinces studies and in 41% of cases in a study in Fars province (10, 12, 13). All of these studies show that finger desquamation in Iranian patients is less common and it is not reliable as a follow up measurement in patients with incomplete criteria and it is necessary to lower the threshold of echocardiography performing in suspected febrile patients.
According to Figure 2, among the associated clinical findings, cough, vomiting and diarrhea, respectively, were the most common, although other studies have shown a greater importance of gastrointestinal symptoms in 65% of cases and respiratory symptoms in 30% (1). The presence of these symptoms is very important, because, although one of the main criteria for the KD diagnosis is a fever not explainable with other causes, there is a constant emphasis on the increasing incidence of gastrointestinal and respiratory symptoms in recent years.
Among laboratory findings, leukocytosis, thrombocytosis, and anemia, respectively, were the most common supplementary laboratory criteria, in consistence with Yazd and Tehran provinces studies (9, 12). Anemia and leukocytosis were significantly more frequent in patients with incomplete KD. These findings suggested that the complete blood count (CBC), as a cost-effective test. is likely to further give a picture of the three supplementary criteria required for diagnosis of incomplete KD. Sterile pyuria was found in 22% of cases, which, according to references, is usually found in half of the patients. As it is a transient finding, it is suggested to repeat the urine analysis (UA) in suspected cases.
If fever persists for up to 36 hours after completion of the initial IVIG, a second dose of immunoglobulin should be administered. In this study, only 12.1% of cases required the repetitive dose. This result was similar to other studies in which the need for a repetitive dose of IVIG was reported in 15% of cases (1, 4). Although the effects of corticosteroids in the prevention of coronary involvement has not been proven to date, it is recommended to administer methylprednisolone in the presence of persistent fever after the second dose of IVIG. In our study, only two patients received methylprednisolone, which was similar to the results of other reports (1, 4, 14). In addition, the coronary aneurysm in the timely-treated patients (14.8% of all cases) was very impressive compared to the other studies. Coronary involvement was reported 7.2% in a study on Taiwanese children and in almost 9% in Fars province, and was identical with that of Rezaei et al. in Mazandaran (2, 7, 10).
The relationship between the diagnosed coronary involvement in echocardiography in different phases of the disease (acute, sub-acute, and at the end of treatment) and all clinical findings as well as supplementary laboratory criteria, showed no significant statistical relationship. Furthermore, prolonged fever, considered as a risk factor for coronary aneurysm in other studies, had no significant relationship with our study (1, 12, 15).
Although males aged less than 1 year-old and incomplete KD are considered risk factors for developing coronary involvement by other studies, in our study, there was no significant difference regarding gender and age. However, coronary aneurysms were significantly more common in patients with incomplete KD (P = 0.028) (1, 16, 17).
With respect to the present study and other studies performed in Iran, it seems that despite initiating the treatment in the first 10 days of fever, suggested as the golden time for the prevention of coronary artery aneurysm, cardiac complications occurred much more frequently in our patients. One reason might be the higher frequency of incomplete KD (40.5%) compared to other studies. In our opinion, other national studies should be performed, and, if our results repeated, this would suggest that the golden time for IVIG treatment should be revised and decreased to a safer time, in order to prevent these unpleasant cardiac events in our region, which is considered as a high-prevalence area for KD.
Acknowledgements
References
-
1.
Son M, Newburger J. Kawasaki Disease. In: Kliegman RM, editor. Nelson text book of pediatrics. 19th ed. Philadelphia: Elsevier; 2011. p. 862-7.
-
2.
Huang WC, Huang LM, Chang IS, Chang LY, Chiang BL, Chen PJ, et al. Epidemiologic features of Kawasaki disease in Taiwan, 2003-2006. Pediatrics. 2009;123(3):e401-5. [PubMed ID: 19237439]. https://doi.org/10.1542/peds.2008-2187.
-
3.
Nakamura Y, Yashiro M, Uehara R, Sadakane A, Chihara I, Aoyama Y, et al. Epidemiologic features of Kawasaki disease in Japan: results of the 2007-2008 nationwide survey. J Epidemiol. 2010;20(4):302-7. [PubMed ID: 20530917].
-
4.
Freeman AF, Shulman ST. Kawasaki disease: summary of the American Heart Association guidelines. Am Fam Physician. 2006;74(7):1141-8. [PubMed ID: 17039750].
-
5.
Hiraishi S, Yashiro K, Oguchi K, Kusano S, Ishii K, Nakazawa K. Clinical course of cardiovascular involvement in the mucocutaneous lymph node syndrome. Relation between clinical signs of carditis and development of coronary arterial aneurysm. Am J Cardiol. 1981;47(2):323-30. [PubMed ID: 7468484].
-
6.
Muta H, Ishii M, Yashiro M, Uehara R, Nakamura Y. Late intravenous immunoglobulin treatment in patients with Kawasaki disease. Pediatrics. 2012;129(2):e291-7. [PubMed ID: 22250032]. https://doi.org/10.1542/peds.2011-1704.
-
7.
Rezai MS, Shokohi L, Saffar MJ, Zeinali A, Abbaskhanian A. Relationship between Eosinophilia with Coronary Artery Disease in Patients with Kawasaki Disease. J Mazand Univ Med Sci. 2012;22(88):10-6.
-
8.
Azhar AS, Al-Attas A. Risk factors for coronary artery lesions in Kawasaki disease. Med Glas (Zenica). 2013;10(2):254-7. [PubMed ID: 23892841].
-
9.
Moradinejad MH, Kiani A. Kawasaki disease in 159 iranian children. Iran J Pediatr. 2007;17(3):241-6.
-
10.
Asadi-Pooya AA, Borzoee M, Amoozgar H. The experience with 113 patients with Kawasaki disease in Fars Province, Iran. Turk J Pediatr. 2006;48(2):109-14. [PubMed ID: 16848108].
-
11.
Saket S, Mojtahedzadeh S, Karimi A, Shiari R, Shirvani F. Relationship between Electrolyte Abnormalities, ESR, CRP and platelet count with Severity of Kawasaki Disease. Yafteh. 2009;11(3):5-14.
-
12.
Golestan M, Bahjati M, Akhavan-karbasi S, Roozbeh P. Review of Kawasaki Patients in Yazd. J Shahid Sadoughi Univ Med Sci. 2009;16(4):21-5.
-
13.
Rahmati MB, Houshmandi MM. Evaluating the clinical and paraclinical aspects of Kawasaki patients referred to Bandar-Abbas children hospital during 2008-2011. Feyz J Kashan Univ Med Sci. 2012;16(4).
-
14.
Ogata S, Ogihara Y, Honda T, Kon S, Akiyama K, Ishii M. Corticosteroid pulse combination therapy for refractory Kawasaki disease: a randomized trial. Pediatrics. 2012;129(1):e17-23. [PubMed ID: 22144699]. https://doi.org/10.1542/peds.2011-0148.
-
15.
Schroh AM, Dominguez P, Laghezza LB, Melonari PA, Olguin M, Miatello R. [Kawasaki disease: heart disease during childhood]. Rev Esp Cardiol. 2006;59(4):387-90. [PubMed ID: 16709393].
-
16.
No SJ, Kim DO, Choi KM, Eun LY. Do predictors of incomplete Kawasaki disease exist for infants? Pediatr Cardiol. 2013;34(2):286-90. [PubMed ID: 23001516]. https://doi.org/10.1007/s00246-012-0440-3.
-
17.
Ruan Y, Ye B, Zhao X. Clinical characteristics of kawasaki syndrome and the risk factors for coronary artery lesions in China. Pediatr Infect Dis J. 2013;32(10):e397-402. [PubMed ID: 23722531]. https://doi.org/10.1097/INF.0b013e31829dd45e.
