Abstract
Background:
Congenital anomalies are considered as one of the major causes of neonatal death. The prevalent pattern of congenital anomalies may vary diachronically or geographically. With regard to the pervasiveness of under-five mortality (probability of dying between birth and exactly 5 years old) in Hamadan province in the recent years, the present study intended to determine the risk factors of congenital anomalies of newborns in Hamadan province in 2017.Methods:
The present case-control study was conducted in the hospitals affiliated to Hamadan University of Medical Sciences for 6 months in 2017. The study targeted all the newborns from birth to hospital discharge. The neonatal cases with congenital anomalies were identified through clinical examination. A report sheet was assigned to a healthy newborn, as a control, per each case of congenital anomalies born on the same day and in the same hospital. Once data was collected, they were statistically analyzed by means of SPSS V. 16 software.Results:
According to the current results, the prevalence of congenital anomalies was 0.85% (8.5 per 1,000 live births). Genitourinary (40%), musculoskeletal (25.2%), eye, ear and neck (18.5%), chromosomal (5.9%), respiratory tract (3.7%) and cardiovascular system (2.2%) were the most common congenital anomalies, respectively. Consanguineous marriage, concomitant use of contraceptive methods and male sex were found to be the most important risk factors for congenital anomalies.Conclusions:
The present study aimed at identifying the various types and prevalence of congenital anomalies in Hamadan province. Regular prenatal examination and early diagnosis for prevention, early intervention and scheduled termination of pregnancy are recommended. Besides, public awareness of the disadvantages of consanguineous marriage and other pertaining risk factors affecting the incidence of congenital anomalies is also recommended.Keywords
1. Background
Congenital anomalies refer to any anatomic birth malformations that are diagnosable in almost 3% - 5% of newborns (1-4). The etiology of congenital anomalies is multifactorial which remains unrecognized in 40% - 60% of birth defects. The observed risk factors for congenital anomalies consisted of 15% for genetic and chromosomal attributes, 10% for environmental exposures and 20% - 25% for the interplay of genetic and environmental factors (5-9). An annual amount of 30,000 - 40,000 disabled and paralyzed infants are born in Iran; the disability of these infants not only does make them suffer from many physical and psychological disorders throughout their life but also causes their families and the government countless psychological and economic problems (10-12). Despite etiologic and pathogenic advancements, about 22% cases of neonatal deaths are caused by major congenital anomalies. Such internal malformations as renal, cardiovascular and pulmonary anomalies may not be identified at birth but later in life (13); that is why the prevalence of congenital anomalies reaches 3% - 4% at exactly 1 years old while it equates 5% - 6% at the age of five (14). Congenital anomalies range from mild to severe defects and are classified into single and multiple body involvement. Severe anomalies are easy to diagnose while the mild ones require more accurate clinical examinations. The significance of mild anomalies is due to the fact that they may be a part of a specific syndrome, whose detection facilitates the diagnosis of the syndrome (15-19). Various outbreaks of anomalies have been proven in different races. Research has shown that nearly 15% of neonatal deaths are attributed to severe anomalies. The prevalence of anomalies in LBW (low birth weight) newborns, preterm infants and both fourth-time mothers and those older than 35 years is respectively 3 times, 4 times and twice as much as the total cases of anomalies at live births. Family medical history, patients’ sex and disease severity affect the recurrence of anomalies in subsequent children. The overall prevalence of congenital anomalies has got a descending trend in different countries (20-22).
2. Objectives
The present study intended to determine the risk factors for congenital anomalies of newborns in Hamadan province in order to accentuate the significance of pre- and post-marriage genetic testing so as to prevent births with potential severe malformations through early prenatal diagnosis.
3. Methods
The present case-control study was conducted on the hospitals affiliated with both Hamadan University of Medical Sciences and the Social Security Organization as well as private hospitals in Hamadan for 6 months in 2017. The inclusion criteria targeted all the infants born in the hospitals of Hamadan province whereas exclusion criteria involved Hamadan non-residents and incomplete questionnaires. Case refers to all newborns with congenital anomalies while control denotes infants who were born in the same hospitals and without any clinically observed congenital anomalies. One control was intended per each case with homogeneous neonatal sex, maternal age, and place of residence (city or town). Data collection tool was a standard inventory retrieved from the website (Child Death Care System tab) of Children Department in the Ministry of Health. The questionnaire was composed of 8 sections including demographic information, delivery information, neonatal medical history, and neonatal examination and pertaining anomalies, diagnostic interventions, family medical history, pregnancy history (exposure to risk factors) and maternity lifestyle. The exposure variables used to compare the case and control groups included maternal medications, smoking habit, drug and alcohol abuse, parental consanguineous marriage, history of abortion, history of or exposure to eruptive diseases associated with fever during pregnancy, preterm delivery, maternal underlying diseases, exposure to X-ray or chemicals, surgery during pregnancy, stress, hormonal contraception and infertility therapies. Sampling was carried out using census method. Neonatal cases with congenital anomalies (minor and major) were identified. The sample size encompassed all births with congenital anomalies during the research time. A report sheet was assigned to a healthy newborn, as a control, per each case of congenital anomalies born on the same day and in the same hospital. Data were collected through neonatal physical examination, interviewing the mothers, reviewing medical dossiers and completing the registration form by the interviewer.
3.1. Statistical Analysis
To analyze data, we used Independent-sample t-test and chi-square test to assess the associations. Moreover, to control confounding factor, logistic regression was used. A P value less than 0.05 was considered statistically significant. SPSS version 16 was used for analysis.
3.2. Definition of the Key Terms
3.2.1. Congenital Anomalies
Congenital anomalies refer to any anatomic defects at birth, which are diagnosed based on clinical examinations on the delivery day by a pediatrician using fetal or neonatal radiography, ultrasonography and echocardiography which are recorded.
3.2.2. Consanguineous Marriage
Consanguineous marriage is the union between two individuals of the same kinship i.e. the matrimony between either third-degree relatives (coefficient of relationship, R = 12.5%) such as cousins or fourth-degree relatives (R = 6.25%) such as cousins’ children or fifth-degree relatives (R = 3.13) such as grandchildren of uncles and aunts.
4. Results
About 135 out of 15,901 live births were reported with congenital anomalies, i.e. 0.85% of the total newborns. For the purpose of the present study, 270 subjects were selected and assigned to two groups of case with 135 congenital anomalies and control with 135 healthy infants. There was not any statistically significant difference between the case and control groups in terms of mean neonatal weight, mean parental age, maternal occupation, paternal occupation, place of residence, chronic maternal disease, maternal drug intake, pregnancy problems, radiography during pregnancy, preterm delivery, use of fertility assisted therapy, surgery during pregnancy, stressful pregnancy, exposure to chemicals and family medical history of congenital anomalies (P > 0.05). Moreover, there was a significant relationship between congenital anomalies and variables such as consanguineous marriage, pregnancy despite the use of contraceptive methods, emergency C-section delivery and male-sex ratio (P < 0.05). Since both case and control groups were sexually homogeneous, the ratio of male/female sex of all births was compared with the cases of anomalies in order to investigate the relationship between sex ratio and congenital anomalies. The results showed that the sex ratio of male infants was higher than the female ones. There was also a significant relationship between congenital anomalies and such disorders as nutritional and respiratory problems (Table 1).
| Variable | Case Group | Control Group | P Value |
|---|---|---|---|
| Mean neonatal weight, gr | 2800 | 2900 | 0.68 |
| Mean maternal age | 28.6 | 28.5 | 0.89 |
| Mean paternal age | 32.1 | 32.8 | 0.75 |
| Maternal occupation | 0.99 | ||
| Employed | 9 (6.7) | 9 (7.4) | |
| Housewife | 126 (93.3) | 125 (92.6) | |
| Paternal occupation | 0.09 | ||
| Employed | 28 (20.7) | 18 (13.3) | |
| Self-employed | 68 (50.4) | 87 (64.4) | |
| Worker | 38 (28.1) | 29 (21.5) | |
| Unemployed | 1 (0.7) | 1 (0.7) | |
| Place of residence | 0.99 | ||
| City | 84 (62.2) | 85 (62.9) | |
| Town | 51 (37.7) | 50 (37.1) | |
| Acute maternal disease | 0.18 | ||
| Yes | 10 (7.4) | 3 (2.2) | |
| No | 51 (37.7) | 132 (97.8) | |
| Consanguineous marriage | 10 (7.4) | 6 (4.4) | 0.001 |
| 3rd-degree | 25 (18.5) | 3 (2.2) | |
| 4th-degree | 1 (0.7) | 1 (0.7) | |
| 5th-degree | 1 (0.7) | 2 (1.4) | |
| Maternal drug intake | 0.3 | ||
| Yes | |||
| A. Folic acid | 112 (83) | 116 (85.9) | |
| B. Other drugs | 7 (5.2) | 2 (1.5) | |
| No | 16 (11.9) | 17 (12.6) | |
| History of pregnancy problems | 6 (4.4) | 1 (0.7) | 0.12 |
| Oligohydramnios | 1 (0.7) | 0 (0.0) | |
| Myoma | 2 (1.5) | 0 (0.0) | |
| Intrauterine death | 1 (0.7) | 0 (0.0) | |
| Frequent abortion | 2 (1.5) | 1 (0.7) | |
| Radiography during pregnancy | 1 (0.7) | 1 (0.7) | 0.99 |
| Preterm delivery | 37.9 | 38.3 | 0.15 |
| Hormonal contraception | 6 (4.4) | 0 (0.0) | 0.03 |
| Use of contraceptive methods | 1 (0.7) | 2 (1.4) | 0.99 |
| Maternal surgery during pregnancy | 2 (1.4) | 0 (0.0) | 0.06 |
| Stressful pregnancy | 4 (3) | 0 (0.0) | 0.14 |
| Exposure to chemicals | 1 (0.7) | 6 (4.4) | 0.14 |
| Family medical history of congenital anomalies | 10 (7.4) | 5 (3.7) | 0.28 |
| Type of delivery | 0.008 | ||
| Vaginal | 54 (40) | 59 (43.7) | |
| Assisted vaginal | 1 (0.7) | 0 (0) | |
| Elective C-section | 26 (19.3) | 43 (31.9) | |
| Emergency C-section | 54 (40) | 33 (24.4) | |
| Neonatal Disorders | |||
| Nutritional problems | 20 (14.8) | 5 (3.7) | 0.002 |
| Respiratory distress | 4 (10.4) | 1 (0.7) | 0.001 |
| Sexb | 0.02 | ||
| Female | 42 (31) | 7739 (48.7) | |
| Male | 93 (69) | 8162 (51.3) |
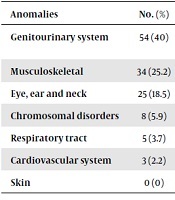
According to the results of the present study, the most prevalent congenital anomaly belonged to genitourinary system (40%) and the least one was related to cardiovascular system (2.2%). None of newborns had skin anomalies (Table 2).
Prevalence of Anomalies in the Intended Newborns
| Anomalies | No. (%) | Type of Anomaly, No. (%) |
|---|---|---|
| Genitourinary system | 54 (40) | Hypospadias: 20 (14.8); undescended testis: 15 (11.1); hydronephrosis: 7 (5.2); kidney dysgenesis: 5 (3.7); epispadias: 2 (1.5); polycystic kidney: 1 (0.7); renal octopi: 1 (0.7) |
| Musculoskeletal | 34 (25.2) | Clubfoot: 21 (15.6); polydactyly: 5 (3.7); limb shortness: 5 (3.7); syndactyly: 3 (2.2) |
| Eye, ear and neck | 25 (18.5) | Cleft lip: 13 (9.6); cleft palate: 3 (2.2); anophthalmia: 2 (1.5); microphthalmia: 2 (1.5); hypertelorism: 1 (0.7); other: 4 (3) |
| Chromosomal disorders | 8 (5.9) | Down syndrome: 5 (3.7); trisomy 13: 1 (0.7); other: 2 (1.5) |
| Respiratory tract | 5 (3.7) | Diaphragmatic hernia: 2 (1.5); other: 3 (2.2) |
| Cardiovascular system | 3 (2.2) | Transposition of great vessels: 1 (0.7); other: 2 (51.5) |
| Skin | 0 (0) |
5. Discussion
Based on the results of the present study, the highest rate of anomalies was respectively observed in Tuyserkan (2.4%), Hamedan (1.3%), and Nahavand (0.4%), while Kaboudarhang (0.2%) and Razan (0.2%) had the least prevalence. However, a part of the observed data on the prevalence of congenital anomalies in Hamedan encompassed the referrals from other towns due to the high frequency of high-risk pregnancy referrals to the provincial capital. The prevalence of congenital anomalies was 0.85% (8.5 per 1,000 live births) in the present study. According to various studies over Iran and other countries, there has been different statistics (1% - 10%) on the prevalence of congenital anomalies. Such cities as Zanjan had the highest prevalence (5.5%) while Arak was least prevalent (0.82%) in Iran. Amongst foreign countries, Uganda was reported to have the highest rate of congenital anomalies (7.6%) in the world (23). The contradictory statistics on the prevalence of congenital anomalies in Iran over other countries may contribute to the genetic, racial, cultural, social and economic differences as well as diverse neonatal assessment methods and distinct types of anomalies. It should be noted, however, that some studies have only targeted observable anomalies. In addition to the distinctive characteristics (live or dead births) of the intended statistical population in each study, the use of different diagnostic methods is conductive to the emergence of different findings.
The most common congenital anomaly was related to the genitourinary system (40%), with hypospadias ranking first, while musculoskeletal system (25.2%) scored second, with clubfoot as highly prevalent amongst the observed anomalies. Khoshhal-Rahdar et al. (24) and Alijahan et al. (25) found musculoskeletal anomalies as the most common congenital defects. In the Hosseini et al. (26) study, anomalies of eye, ear and face ranked first followed by nervous system disorders. According to Jalali et al. (23), the most and the least prevalent congenital anomalies were respectively linked to musculoskeletal and genitourinary abnormalities. The contrasting rate of prevalence reported by various studies may be attributed to the significant role of underlying factors in disease development and the basis for the diagnostic methods of congenital anomalies since most inherited defects are mainly recognized on the basis of clinical examinations. Despite precise initial physical examinations by pediatricians, some congenital anomalies were not initially diagnosed due to their specific nature (unobservable at birth) while other defects required radiography and echocardiography.
Considering the relationship between the occurrence of congenital anomalies and the potential risk factors, the most significant risk factors affecting congenital anomalies were recognized to be consanguineous marriage, concomitant use of contraceptive methods, emergency C-section delivery, and male-sex ratio in the present study. Moreover, congenital anomalies were highly observable in male than female newborns, which was consistent with findings of Mohammadzadeh et al. (27), Shokouhi and Mani Kashani (28), and Golalipour et al. (29). The prevalence of anomalies in male newborns may be due to the fact that female births undergo more lethal congenital anomalies and are less likely to survive than the male infants (30).
The present findings showed that the risk of malformed births was 4.5 times higher in parents with consanguineous marriage, with the third-degree marriages (92.5%) ranking first. Alijahan et al. (25) and Kushaki and Zeyghami (31) indicated that parental consanguinity significantly surged the risk of abnormal births to respectively 2.3 and 8.7 time more than other factors. The prevalence of consanguineous marriage ranges from 17 to 31 percent in Iran (31), the differing range of which may contribute to its diverse frequency in different districts of Iran.
Moreover, emergency C-section delivery was the most common risk factor for congenital anomalies amongst various types of delivery. Nevertheless, since the presence of a potential congenital abnormality may necessitate an emergency C-section, they present more association than vaginal delivery; this is in line with the findings of Sarkar et al. (30).
The significant relationship between hormonal contraceptive methods and the risk of congenital anomalies in the intended newborns highlights the importance of healthy fertility care.
Since such variables as parental age, parental occupation and place of residence (city or town) did not significantly correlated with congenital anomalies, they were not recognized as risk factors for anomalies. Parental age, however, was considered as an identified agent for fetal chromosomal disorders; accordingly, most birth cases with Down’s syndrome were prenatally aborted through early diagnostic screening during pregnancy and those born with Down’s syndrome constitute only a little percentage of abnormal cases. This is why maternal age was not found to be a potential risk factor for congenital anomalies.
According to the findings of the present study, such risk factors as acute maternal disease (7.4% vs. 3.3%), maternal drug intake (5.2% vs. 1.5%), family medical history of congenital anomalies (7.4% vs. 3.7%), history of pregnancy problems (3.4% vs. 0.7%) and stressful pregnancy (3% vs. 0%) were apparently observed while insignificantly different, in abnormal births.
Besides, nutritional problems and respiratory distress were most common in the abnormal group that can be assignable to congenital anomalies.
5.1. Conclusions
The results of the present study identified various types and prevalence of congenital anomalies in Hamedan province. Regular prenatal examination and early diagnosis are recommended for prevention, early intervention and scheduled termination of pregnancy. Besides, public awareness of the disadvantages of consanguineous marriage and other pertaining risk factors affecting the incidence of congenital anomalies is also recommended.
Acknowledgements
References
-
1.
Ahmadzadeh A, Safikhani Z, Abdulahi M, Ahmadzadeh A. [Congenital malformations among live births at Arvand Hospital, Ahwaz, Iran: A prospective study]. Pakistan J Med Sci. 2008;24(1):33. Persian.
-
2.
Dolk H, Loane M, Garne E. The prevalence of congenital anomalies in Europe. Adv Exp Med Biol. 2010;686:349-64. [PubMed ID: 20824455]. https://doi.org/10.1007/978-90-481-9485-8_20.
-
3.
Bowles D, Wasiak R, Kissner M, van Nooten F, Engel S, Linder R, et al. Economic burden of neural tube defects in Germany. Public Health. 2014;128(3):274-81. [PubMed ID: 24559770]. https://doi.org/10.1016/j.puhe.2013.12.001.
-
4.
Corsello G, Giuffre M. Congenital malformations. J Matern Fetal Neonatal Med. 2012;25 Suppl 1:25-9. [PubMed ID: 22356564]. https://doi.org/10.3109/14767058.2012.664943.
-
5.
Rahbar M, Ahmadi M, Lornejad HR, Habibelahi A, Sanaei-Shoar T, Mesdeaghinia AR. Mortality causes in children 1–59 Months in Iran. Iran J Pub Health. 2013;42(Supple1):93.
-
6.
Bateni A, Dastgiri S, Mosaferi M, Heidarzadeh M. Applications of spatial analysis in congenital anomalies registries. J Clin Res Govern. 2013;2(2):70-2. https://doi.org/10.13183/jcrg.v2i2.23.
-
7.
Golalipour MJ, Mirfazeli A, Mobasheri E. Incidence and pattern of congenital malformations in Gorgan-North of Iran. J Med Sci. 2013;13(8):834-8. https://doi.org/10.3923/jms.2013.834.838.
-
8.
Abdi-Rad I, Khoshkalam M, Farrokh-Islamlou HR. [The prevalence at birth of overt congenital anomalies in Urmia, Northwestern Iran]. Arch Iran Med. 2008;11(2):148-51. Persian.
-
9.
Dastgiri S, Kalankesh LR, Heidarzadehe M, Tajahmad A, Rezaian E. A new registry of congenital anomalies in Iran. J Registry Manag. 2010;37(1):27-9.
-
10.
Sadler TW. Langman's medical embryology. 12th ed. Philadelphia, United States: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2012.
-
11.
Dastgiri S, Stone DH, Le-Ha C, Gilmour WH. Prevalence and secular trend of congenital anomalies in Glasgow, UK. Arch Dis Child. 2002;86(4):257-63. [PubMed ID: 11919098]. [PubMed Central ID: PMC1719147]. https://doi.org/10.1136/adc.86.4.257.
-
12.
Mozafari Kermani R, Nedaeifard L, Nateghi M, Fazeli S, Ebrahim A, Ahmadi M, et al. Congenital anomalies in infants conceived by assisted re-productive techniques. Arch Iran Med. 2012;15(4):228-31.
-
13.
Parmar A, Rathod SP, Patel SV, Patel SM. A study of congenital anomalies in newborn. NJIRM. 2010;1(1):13-7.
-
14.
Carlson BM. Human embryology and developmental biology. 2nd ed. Baltimore: Mosby Company; 1998. p. 128-95.
-
15.
McLean SD,. Congenital anomalies. In: Avery GB, Fletcher MA, MacDonald MG, editors. Neonatology: Pathophysiology and management of the newborn. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 1999.
-
16.
Mohammed YA, Shawky RM, Soliman AAS, Ahmed MM. Chromosomal study in newborn infants with congenital anomalies in Assiut University Hospital: Cross-sectional study. Egypt J Med Hum Gen. 2011;12(1):79-90. https://doi.org/10.1016/j.ejmhg.2011.02.003.
-
17.
Marden PM, Smith DW, McDonald MJ. Congenital anomalies in the newborn infant, including minor variations: A study of 4412 babies by surface examination for anomaliesand buccal smear for sex chromatin. J Pediatr. 1964;64(3):357-71. https://doi.org/10.1016/s0022-3476(64)80188-8.
-
18.
Shajari H, Mohammadi N, Karbalai Aghai M. [Prevalence of congenital malformations observed in neonates in Shariati Hospital (2000-2003)]. Iran J Pediatr. 2006;16(3). Persian.
-
19.
Pober BR. Overview of epidemiology, genetics, birth defects, and chromosome abnormalities associated with CDH. Am J Med Genet C Semin Med Genet. 2007;145C(2):158-71. [PubMed ID: 17436298]. [PubMed Central ID: PMC2891729]. https://doi.org/10.1002/ajmg.c.30126.
-
20.
Erickson JD. Racial variations in the incidence of congenital malformations. Ann Hum Genet. 1976;39(3):315-20. [PubMed ID: 776064]. https://doi.org/10.1111/j.1469-1809.1976.tb00135.x.
-
21.
Rosano A, Botto LD, Botting B, Mastroiacovo P. Infant mortality and congenital anomalies from 1950 to 1994: An international perspective. J Epidemiol Community Health. 2000;54(9):660-6. [PubMed ID: 10942444]. [PubMed Central ID: PMC1731756]. https://doi.org/10.1136/jech.54.9.660.
-
22.
Obu HA, Chinawa JM, Uleanya ND, Adimora GN, Obi IE. Congenital malformations among newborns admitted in the neonatal unit of a tertiary hospital in Enugu, South-East Nigeria--a retrospective study. BMC Res Notes. 2012;5:177. [PubMed ID: 22472067]. [PubMed Central ID: PMC3393607]. https://doi.org/10.1186/1756-0500-5-177.
-
23.
Jalali S, Fakhraie S, Afjaei S, Kazemian M. [The incidence of obvious congenital abnormalities among the neonates born in Rasht hospitals in 2011]. J Kermanshah Univ Med Sci. 2011;19(2):109-7. Persian.
-
24.
Khoshhal-Rahdar F, Saadati H, Mohammadian M. [The prevalence of congenital malformations in Dezful 2012]. Genet 3rd Millennium. 2014;12(3):3622-31. Persian.
-
25.
Alijahan R, Mirzarahimi M, Ahmadi Hadi P, Hazrati S. Prevalence of congenital abnormalities and its related risk factors in Ardabil, Iran, 2011. Iran J Obstet Gynecol Infertil. 2013;16(54):16-25.
-
26.
Hosseini S, Nikravesh A, Hashemi ZS, Rakhshi N. [Race of apparent abnormalities in neonates born in Amir-Almomenin Hospital of Sistan]. J North Khorasan Univ Med Sci. 2014;6(3):573-9. Persian. https://doi.org/10.29252/jnkums.6.3.573.
-
27.
Mohammadzadeh I, Sorkhi H, Alizadeh-Navaei R. [Prevalence of external congenital malformations in neonates born in Mehregan Hospital, North of Iran]. Iran J Neonatol. 2013;11(1):2990-5. Persian.
-
28.
Shokouhi M, Mani Kashani KH. [Prevalance of obvious congenital anomalies and some related factors in newborns in Fatemieh Hospital of Hamedan during March to September 1999]. J Mazandaran Univ Med Sci. 2002;12(35):42-7. Persian.
-
29.
Golalipour MJ, Ahmadpour-Kacho M, Vakili MA. Congenital malformations at a referral hospital in Gorgan, Islamic Republic of Iran. East Mediterr Health J. 2005;11(4):707-15.
-
30.
Sarkar S, Patra C, Dasgupta MK, Nayek K, Karmakar PR. Prevalence of congenital anomalies in neonates and associated risk factors in a tertiary care hospital in eastern India. J Clin Neonatol. 2013;2(3):131-4. [PubMed ID: 24251257]. [PubMed Central ID: PMC3830148]. https://doi.org/10.4103/2249-4847.119998.
-
31.
Kushki AM, Zeyghami B. [The effect of consanguineous marriages on congenital malformation]. J Res Med Sci. 2005;10(5):298-301. Persian.