Abstract
Context:
Chemical, biological, radiological and nuclear (CBRNs) disasters represent a disconcerting event for governments, health care providers, the public, and hospitals need to be prepared to cope with such disasters. Therefore, the present scoping review was conducted to identify and analyze the parameters and global experiences of hospital preparedness against CBRN disasters.Methods:
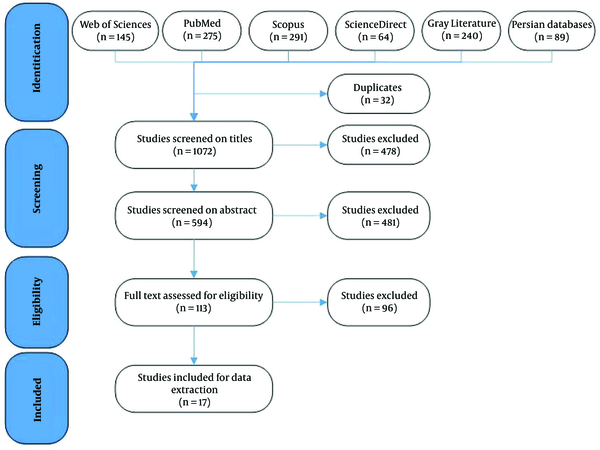
The study is a scoping review that examines English and Persian databases including PubMed, Scopus, Web of Science, Science Direct, Google Scholar, and Jihad Daneshgahi Scientific Information Database (SID), Iranian Research Institute for Information Science and Technology, Magiran, and Iranmedex. Reviewing the studies found on the search bases was carried out in three stages; title, abstract and full text. According to refined studies, the data were extracted in order to meet the objectives and respond to the research questions.Results:
In the initial search, 1104 articles were identified. First, the articles were reviewed in terms of duplication, year of publication, title, abstract, and relevance to the topic, and finally, 17 articles that met the inclusion criteria were incorporated in the systematic review process. Finally, 8 primary issues addressed in the articles, including (1) staff training, (2) planning to deal with disasters, (3) personal protection equipment, (4) risk perception, (5) decontamination of medical centers and wards, (6) detection of CBRN infection, (7) availability of drugs and antidotes, and (8) the presence of health professionals and staff were discussed. The review of findings reported by various studies revealed shortcomings in the above eight areas.Conclusions:
Most hospitals have begun to undertake activities to deal with CBRN and follow a special program for this purpose. However, due to the industrialization of human societies and the surge in CBRN events and other threatening activities, this level of preparedness is not satisfactory and further planning is warranted. However, the present study offers valuable insights and recommendations for policymakers and hospital managers to improve their hospital preparedness for the risks of CBRN disasters.Keywords
Hospital Preparation Chemical Accidents Biological Accidents Radiation Accidents Scoping Review
1. Context
The risk of chemical, biological, radiological and nuclear (CBRN) disasters is rising due to advances in technology and the growing tendency of terrorists to resort to unconventional weapons (1). Given the intangible nature of CBRN threats, they fall into the category of the "terrible" risks (2). Besides, the consequences of CBRN and its catastrophic power have not yet been full. Hence, they may be frightening to the general people and pose a major public concern. There are basic measures that, if taken swiftly, can alleviate the harms inflicted on the victims of such attacks and play a major role in mitigating the harmful effects of such events and their psychological consequences on public health (3, 4).
The repercussions of the CBRN have recently amplified in terms of human mortality and economic costs. Exposure to chemicals during terrorist acts or the transportation of a wide range of these materials by road, railway, sea or air can contribute to the intensification of such consequences (5). On the other hand, the prevalence of various diseases induced by biological events in recent decades, such as acute respiratory syndrome, influenza, Ebola, emerging infectious diseases, bioterrorism accidents and public health emergencies can be seen as hazardous threats to public health (6). In addition, today, with the expansion of nuclear technology in various industries worldwide, the risk of nuclear accidents and damage has been on the rise. In recent years, the risk of terrorist attacks and accidental radiation has also escalated. Hence, most countries in the world spend millions of dollars to fight terrorism (7).
In general, there are growing national and international concerns about CBRN disasters. The chief concerns are related to the unexpected nature of this type of disaster and their ensuring consequences due to poor public awareness, lack of resources and planning, and absence of preparation to cope with such accidents (8). Given that CBRN disasters are a disturbing event for governments, health care providers and the public, and considering that hospitals are often at the forefront of dealing with these disasters, they need to be more prepared to tackle CBRN disasters (9).
As hospitals are the main center for treating and monitoring CBRN accidents, preparation for early diagnosis and management of these disasters is essential. Therefore, special attention should be paid to the professional practice, available resources, and skills to deal with the CBRN accident in the hospital (9, 10). But previous studies have shown that hospitals are not prepared to deal with accidents (10-12). Therefore, the necessary actions need to be planned and prepared so that the hospital can respond to these disasters and mitigate their impact (13). In this regard, identifying the components of hospital preparedness for these disasters is the first step in assessing, planning, and improving hospital preparedness for CBRN disasters (9). The purpose of this study is to identify and analyze the parameters and global experiences of hospital preparedness against CBRN disasters. Therefore, in this study, a systematic literature review was conducted to discover research related to hospital preparedness for CBRN disasters in particular.
2. Methods
The present study is a review conducted systematically in 2021 with a scoping review approach. This study conducted based Arksey and O'Malley’s approach (2005) (10) to identify and analyze the parameters and global experiences of hospital preparedness against CBRN disasters.
2.1. Data Sources and Search Strategy
In the first stage, relevant keywords were identified by reading relevant articles and consulting experts in this field. The keywords including Hospital Assessment, Preparedness, Model proposing, Chemical, Biological, Radiological and Nuclear were searched using a combination of NOT, OR, AND commands in the mentioned databases.
In the second stage, online databases including PubMed, Scopus, Web of Science, Science Direct, Google Scholar as well as Iranian databases including Scientific Information Database (SID), Iranian Research Institute for Information Science and Technology, Magiran, IranMedex were reviewed based on the search strategy. Also, the Cochrane database was searched initially, to ensure that the study was not repeated. The literature search was done by a library specialist. The search results for screening were entered into the EndNote v.X8 software (Table 1).
Databases and Search Strategy
| Search Strategy | |
|---|---|
| PubMed | #1: (Chemical[Title] OR Biological[Title] OR radiological[Title] OR radiation[Title] OR Nuclear[Title] OR CBRN[Title] OR "Nuclear Accident"[Title] OR "Chemical Accident"[Title] OR "Biological Accident"[Title] OR "radiological Accident"[Title]) OR (Belgium OR chemical OR biological OR radiation OR nuclear [MeSH Terms]) |
| #2: Model[Title] OR Pattern[Title] OR plan[Title] OR Template[Title] | |
| #3: ("hospital preparedness"[Title] OR hospital[Title]) OR (disaster preparedness OR hospital preparedness [MeSH Terms]) | |
| #4: #1 AND #2 AND #3 | |
| Scopus | TITLE-ABS-KEY (Chemical OR Biological OR radiological OR radiation OR Nuclear OR CBRN OR "Nuclear Accident" OR "Chemical Accident" OR "Biological Accident" OR “radiological Accident") AND TITLE (Model OR Pattern OR plan OR Template) AND TITLE ("hospital preparedness" OR hospital) |
| Science Direct | Title: (Chemical OR Biological OR radiological OR radiation OR Nuclear OR CBRN OR “Nuclear Accident” OR “Chemical Accident” OR “Biological Accident” OR “radiological Accident”) AND (Model OR Pattern OR plan OR Template) AND (“Disaster preparedness” OR “hospital preparedness” OR hospital) |
| ISI Web of science | TS= (Chemical OR Biological OR radiological OR radiation OR Nuclear OR CBRN OR “Nuclear Accident” OR “Chemical Accident” OR “Biological Accident” OR “radiological Accident”) AND TI= (Model OR Pattern OR plan OR Template) AND TI= (“Disaster preparedness” OR “hospital preparedness” OR hospital) |
2.2. Study Selection: Inclusion Criteria, Screening
Reviewing the studies found on the search bases was carried out in three stages (title, abstract and full text) by two persons individually. In the event of disagreement, the final decision was reached through an agreement, but if no agreement was reached, a third-party’s comments were used. The inclusion criteria were: (1) Articles published between 2000 and 2021; (2) Full text of the article is available; (3) Subject related to CBRN, and (4) Articles in Persian or English. Also, in this study, no restriction was applied for the inclusion of articles based on the type of study. Exclusion criteria were: (1) Articles published before 2000; (2) The full text of the article is not available; (3) Articles published in languages other than Persian and English; (4) Articles irrelevant to the goal of the research. In addition, papers such as letters to the editor were also excluded. Since it was not conventional to do the quality assessment of the studies in scoping reviews (10), the quality of the selected articles was not assessed in this study.
2.3. Data Abstraction
For data extraction, the authors recorded the characteristics of each study in a standard form. This form contained the names of the authors, year of study, place of study, the purpose of study, type of study, population size and the major results achieved in the study. First, two reviewers evaluated the articles independently based on the inclusion criteria. Any disagreements between the authors were settled by a third reviewer.
Descriptive and content analysis methods were adopted for data analysis. Given the diversity of hospital plans for CBRN events and the importance of hospital preparedness, the initial synthesis of studies was undertaken separately for each paper. Descriptive and thematic analysis was run for all articles. To do so, initially one of the authors gathered data from the studies. Then, the accuracy and completeness of extracted data were assessed by another author and confirmed papers were included in Table 2.
Description of the Articled Studied
| Author | Title | Type of Study | Sample Size | Type of Incident | Method of Data Collection Interview | Main Purpose | Topics Studied | Most Important Findings |
|---|---|---|---|---|---|---|---|---|
| Treat et al. (11) | Hospital preparedness for weapons of mass destruction incidents: An initial assessment | Descriptive cross-section | 30 hospitals | Chemical, biological, radiation and nuclear (CBRN) | Interview with hospital director or head nurse | Assessment of hospital preparedness for WMD incidents | Understanding hospital preparedness, extensive decontamination capability and medical response, training of hospital staff, and issues related to hospital facilities | It seems that hospitals studied are not sufficiently prepared in terms of decontamination ability, advanced medical response, awareness of healthcare professionals, health communications and facility security. Therefore, further research is warranted. |
| Mortelmans et al. (12) | Preparedness of Belgian civil hospitals for chemical, biological, radiation, and nuclear incidents: are we there yet? | Descriptive cross-sectional | 138 hospitals | Chemical, biological, radiological and nuclear | A survey form was designed | Assessing the preparedness of Belgian hospitals for CBRN accidents | Hospital accident planning, risk perception, decontamination units, personal protective equipment, antidotes, radiation detection, infection specialists, isolation measures and staff training | Despite the perceived risk, there are still serious threats and gaps in the preparation of Belgian hospitals for CBRN events. However, there is concern that in times of financial crisis, current facilities will be inadequate. |
| Wetter et al. (8) | Hospital preparedness for victims of chemical or biological terrorism | Description-cross-sectional (cross-sectional questionnaire) | 224 hospitals | Chemical and biological | Questionnaire | Assessment of hospital preparedness for terrorism attacks | A study of administrative and training programs, physical resources and inventory of medicines required in emergency cases | The hospitals are generally unprepared to receive and treat victims of chemical or biological terrorism. Significant additional resources are needed locally to improve internal preparedness. |
| Jasper et al. (13) | Preparedness of hospitals to respond to a radiological terrorism event as assessed by a full-scale exercise | Descriptive-cross-sectional | 11 hospitals | Radiation and nuclear | Likert Questionnaire | Assessment of hospital preparedness to deal with the victims of terrorist attacks including chemical, biological and radiological elements | Exercising proper response to radiological incidents, assessing the quality of medical care, hospital preparedness, the importance of the training program and detection of radiation equipment in each of the hospitals studied. | The hospitals studied are not sufficiently prepared to manage the casualties of a radiological disaster. |
| Hsu et al. (14) | Critical assessment of statewide hospital pharmaceutical surge capabilities for chemical, biological, radiological, nuclear, and explosive incidents | Descriptive cross-sectional | 45 hospitals | Chemical, biological, radiation, nuclear and explosive | A survey form was designed | Assessing the hospital's drug response to CBRNE events and making recommendations for drug planning | (1) Developing special protocols and written agreements, accessing emergency supplies and support, implementing plans coordinated with SNS and other training, (2) Hospital drug response to specific biological, chemical and radiological scenarios, and (3) The amount and type of pharmaceutical supplies. | Limited sources of antibiotics are available for prevention or treatment, suggesting that hospitals may not have sufficient resources to deal with a large-scale disaster. |
| Bennett (15) | Chemical or biological terrorist attacks: an analysis of the preparedness of hospitals for managing victims affected by chemical or biological weapons of mass destruction | Descriptive cross-sectional | 102 Hospitals | Chemical and biological | Questionnaire | To assess the preparedness of Mississippi state hospitals to receive the victims of terrorist attacks including chemical weapons or biological weapons | To assess the availability of effective preparation programs, special preparedness training, disinfection facilities, pharmaceutical capacity and equipment, and laboratory diagnostic capabilities of hospitals | Mississippi state hospitals are not adequately prepared to cope with the victims of terrorist attacks, including weapons of mass destruction and chemical weapons. Thus, hospitals need substantial resources at the local, state, and national levels to be "truly" prepared. |
| Mortelmans et al. (16) | Are Dutch hospitals prepared for chemical, biological, or radionuclear incidents? a survey study | Descriptive cross-sectional | 93 hospitals | Chemical, biological, radiation and nuclear | Online survey | Assessing Dutch hospitals readiness for CBRN accidents | Hospital-specific data, information on hospital accident planning, risk perception, availability of decontamination units, personal protective equipment, antidotes, radiation diagnosis, infectious disease specialists, isolation measures and staff training. | Despite risk perception, there are serious gaps in the preparedness of Dutch hospitals to deal with patients involved in CBRN accidents. |
| Ahmadi Marzaleh et al. (17) | Developing a model for hospitals’ emergency department preparedness in radiation and nuclear incidents and nuclear terrorism in Iran | Analytical study | 32 specialists | Radiation and nuclear accident questionnaires | Pairwise comparison questionnaire | Creating a national model for emergency preparedness of hospitals (ED) in the face of radiation and nuclear accidents as well as nuclear terrorism in Iran | Evaluating three main groups of staff, clients and the system structure | Full-scale preparedness requires the promotion of cultural, social, economic and political levels synergistically. Hence, governments must formulate policies to deal with such incidents. |
| Azeem et al. (18) | Perception of preparedness of health care professionals in case of a nuclear, chemical, biological attack/emergency in a tertiary care hospital | Descriptive cross-sectional | 200 biochemical specialists and nurses | Chemical, biological and nuclear | Questionnaire | Assessing the preparedness of nuclear health care professionals perception in the event of an attack or CBN accident in a hospital | Access to a specialist center, access to ventilators, access to bed and laundry, access to staff program | The level of preparedness is associated with the number of training courses and programs passed by the participants and medical staff and those with a postgraduate degree were most prepared, followed by the medical graduates and the nursing staff. |
| Aminizadeh et al. (6) | Hospital preparedness challenges in biological disasters: A Qualitative Study | A qualitative study | Qualitative study-content analysis | 20 Specialists and experts working in the field of biological accidents. | Interview | Identifying the challenges of hospital preparedness for biological events. | Training and practice, resource management, safety and health, patient management, risk assessment, laboratory, monitoring | Iranian hospitals are not ready for biological disasters. Hence, it is recommended that hospital preparation programs be designed based on biological event preparation standards. |
| Eyison et al. (19) | Evaluation of the medical chemical, biological, radiological, and nuclear awareness level of emergency healthcare professionals serving on different centers | Descriptive-cross-sectional and comparative | 67 experts in health care departments | Chemical, biological, radiological and nuclear | Questionnaire | Chemical, biological, radiological and nuclear (CBRN) awareness | Hospital accident program, risk perception and evaluation of CBRN personnel, the status of hospital decontamination wards, the use of personnel protective equipment, antidotes, CBRN training, and demographic information | Emergency health professionals need to be prepared for CBRN events. The world has now recognized the importance of CBRN preparedness after the outbreak of COVID-19. |
| Luther et al. (20) | Issues associated in chemical, biological and radiological emergency department response preparedness | Qualitative study | 1 hospital | Chemical, biological, radiation, and nuclear | Interview | Preparedness of a newly established hospital’s emergency room to deal with chemical, biological, and radiation (CBRs) threats. | Staff protection equipment, mortalities associated with CBR Accidents, mass-casualty incidents (MCI), early detection of contamination and comprehensive biological disaster | Preparedness training must include regular training at the local and national levels, while testing and monitoring systems for automated and measured responses. In this case, emergency staff would be able to provide timely, proper and safe interventions for suspected CBR accidents to obtain the best possible outcome for all parties involved. |
| Candiotti et al. (21) | Emergency Preparedness for biological and chemical incidents: a survey of anesthesiology residency programs in the United States | Qualitative and descriptive | 135 specialist and expert | Chemical and biology | Electronic questionnaire | To assess the preparedness of specialists to tackle clinical problems related to patients exposed to hazardous chemicals and biocides, such as weapons of mass destruction (WMD). | Should this training be mandatory and be repeated every so often? The training programs offered to anesthesia personnel regarding the use of WMD and patient management in US programs | Despite the augmented training of anesthesia personnel to cope with the WMD since 2001, to ensure sufficient preparedness across the United States, further efforts are still warranted, including the possible involvement of The American Society of Anesthesiologists and the American Board of Anesthesiology |
| Mitchell et al. (22) | Are emergency care nurses prepared for chemical, biological, radiological, nuclear or explosive incidents? | Qualitative descriptive | 50 nurses | Chemical, biological, radiation, nuclear and explosive | Questionnaire | To foster nurses' preparedness for CBRN events | Waste management (including clinical waste, contaminated clothing, contaminated water and contaminated bodies management), triage, chain of command, awareness of a wide range of personal equipment protection, and their proper use, decontamination of people and equipment. | The need for a "standard" to evaluate the competency criteria for the role of individuals is essential for CBRN accidents. The assessment tools adopted in this study can help gauge the level of nursing staff preparedness and, if adopted properly, contribute to the preparedness of other health care professionals in general. |
| Alahmari and Khan (23) | Chemical, biological, radiological, and nuclear preparedness of public hospitals in Riyadh | Cross-sectional descriptive | 11 hospitals | Chemical, biological, | Checklist and questionnaire | The hospital preparedness for chemical, biological, radiological and nuclear disasters at Riyadh public hospitals | Basic considerations, planning, training and awareness, methods and modules for biological, chemical and radiological incident preparation | Hospital staff should be trained to handle CBRN emergencies and local exercises should be implemented to foster their preparedness. |
| Aminizadeh et al. (9) | Hospital management preparedness tools in biological events: A scoping review | Review | 20 articles | Biological events | Scoping review | Knowledge on hospital preparedness tools used in biological events and factors affecting hospital preparedness in such incidents | Planning, surge capacity, communication, training and education, medical management, surveillance and standard operation process. | Published evidences of hospital preparedness on biological events as well as the overall quality of the psychometric properties of most studies were limited. |
| Dowlati et al. (24) | Hospital preparedness measures for biological hazards: A systematic review and meta-synthesis | Review | 23 articles | Biological hazards | Systematic review and meta-synthesis | Investigate hospital preparedness measures for biological hazards | Administrative, specialized, and logistical issues regarding preparedness measures for biological hazards in hospitals. | Hospital preparedness for biological hazards is one of the most important hospital disaster plans. |
3. Results
In the preliminary search, 1104 articles were found. Initially, 32 duplicate articles were identified and removed by the authors. Then, the 1072 articles were reviewed based on their titles. In this stage, 478 articles were excluded. In the second phase, 594 studies were reviewed based on their abstracts. Thereby, 481 articles were excluded due to the lack of the inclusion criteria (113 studies were selected). Finally, reviewing the full texts of the remaining studies indicated that 17 studies were eligible for our research. Figure 1 shows the process of identifying and selecting articles. A summary of the features of those studies is presented in Table 2.
PRISMA Flow diagram for reviewing and selecting articles
Finally, 8 main topics discussed in the articles, including (1) training and staff, (2) planning to deal with accidents, (3) personal protective equipment (4) risk perception, (5) decontamination of centers and wards, (6) CBRN contamination detection, (7) availability of drugs and antidotes, and (8) presence of infectious disease specialists and health workers in the wards were discussed.
4. Discussion
4.1. Staff Training
Pre-disaster education and training are crucial for an effective response. Based on the review of previous studies, there is ample evidence that educational interventions for health care providers are crucial to expand knowledge and skills in the face of accidents (20). In this regard, in different wards of the hospital, staff training issues are prioritized, so that special training is provided to handle chemical, biological or radiation disasters relative to the type of activity of the ward. Workshops on the early detection of CBRN emergencies, accident control systems, triage of mass victims, and decontamination procedures for patients exposed to CBRN accidents must be carried out specifically. The training focused on general objectives and self-assessment fall short of inducing the expected results in all areas of the CBRN response. In addition, training courses should be developed in a way that prevents the boredom or exhaustion of staff, because it would subdue their interest in training topics, which can be counterproductive (25). Hence, it is recommended to offer training through senses because it not only promotes the learning process but also helps the retention of information. Research shows that 75% of what is heard is forgotten after 2 days. Moreover, only 10% of what is read, 20% of what is heard, 30% of what is seen, 50% of what is heard and seen, and 80% of what is heard, observed and practiced are retained in the human mind. Therefore, monosensory exercises may not always be effective. Therefore, exercising and participating in drills will most likely contribute to long-term learning. Therefore, to boost the efficiency of training topics, specialized training sessions and exercises should be developed (13). Moreover, the level of training for the staff dealing with such accidents should be tailored to their tasks and role. In light of the existing evidence, it is essential to design training programs and technical courses periodically, usually within 6-9 months, in order to bolster the efficiency of individuals in dealing with CBRN accidents. As a result, given the inevitability of natural disasters, terrorist acts, and CBR incidents in the future, regular training, competency-based training, and practical sessions can help alleviate CBR incidents (20). Therefore, training staff to take care of patients injured at CBRN events should be the top priority of health care managers and policymakers. In their 2001 review of 30 hospitals, Treat et al. reported that about a quarter of their hospital staff had been trained for massacre management. Therefore, they believed that specialized training on WMD is essential and helpful for all staff (11). Bennett also reported that 89.2% of Mississippi state hospitals had programs for staff training (15). The study of Azeem et al. (18) found that participants are not sufficiently prepared for a large-scale nuclear, biochemical and chemical (NBC) accident. In their work, the degree of preparedness was linked to the number of courses and training programs attended by the participants, so that the medical staff with a graduate degree had the maximum preparedness, followed by the medical graduates and the nursing staff. They argued that, in light of the inadequate level of preparedness for CBN disasters, large-scale emergency drills and seminars should be incorporated in undergraduate medical and nursing students' curricula to provide them with the necessary training (18, 20).
4.2. Planning and Preparedness to Deal with Accidents
Lessons learned from past chemical disasters can help hospital directors to make planning and preparation. Because disasters and chemical disasters are less frequent than natural disasters, scant attention has been paid to planning for these disasters in recent years. The CBRN hospital preparedness program must be consistent with other hospital disaster plans. By implementing such a plan, hospitals can protect their staff and victims and adopt appropriate measures at the right time (26). In addition, a specialized team for hospital planning in CBRN incidents, including personnel in charge of emergency planning, emergency services, emergency department staff and nurses, physicians, specialized units, public health, occupational health, environmental organization, water organization and the army is needed (27). A regular program for accidents and chemical disasters consists of all crucial elements such as the assessment of conditions and detection of hazardous materials, availability of essential resources and medicines, zoning, use of personal protective equipment, triage disinfection facilities and special medical services and treatments to ensure a more effective response to chemical events (28, 29). Training is probably the best way to assess preparedness and reaction to chemical events. Such training should include a variety of participants from diverse fields, including public health, firefighting, emergency management team, law enforcement, etc. (27, 30). The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) has made hospital accident maneuvers mandatory twice a year for organizations involved in chemical disasters (31). Preparedness varies from hospital to hospital. For example, Treat et al. (11) reported that 73% (22/30) of hospitals are not well prepared to deal with chemical weapons incidents and the same number of hospitals are not ready for a nuclear event. A study by Bennett found that, in general, Mississippi state hospitals in the United States are not thoroughly prepared to manage victims of terrorist attacks, including WMDs and chemical weapons, and therefore such a disaster may cost the lives of hundreds or even thousands. Thus, hospitals need considerable resources at the local, state and national levels to ensure "real" preparedness (15). Mortelmans et al. observed that in Belgium, university hospitals are significantly more prepared than public hospitals to face CBRN accidents. They posited that, even though 71 hospitals reported a risk of CBRN accidents, only 53 hospitals had contingency plans in their program. However, they pointed to serious gaps in hospital readiness for CBRN events in Belgium, citing poor funding as a major obstacle to desirable preparedness (12). Another study by Mortelmans et al. investigated CBRN preparedness in the Netherlands, one of the most populous countries in Europe. Given that there are several nuclear facilities in the Netherlands, the large petrochemical industry is vulnerable to terrorist targets, but it is not sufficiently prepared for CBRN events (16). Wetter et al. also showed that less than 20% of hospitals in their study had plans for biological or chemical weapons incidents (8).
4.3. Personal Protective Equipment
Personal protective equipment (PPE) is a major challenge facing medical staff at CBRN events. This equipment embraces a wide range of accessories, tools and gears that are designed, and manufactured to protect different parts of the body from a sundry of potential hazards in the workplace. Although health care professionals have extensive training and experience in dealing with general disasters and are prepared to control infection, the use of PPE to combat the CBRN threat represents a new work domain that aims to protect users from several hazardous elements that may be dispersed through air, contact and body secretions. The proper use of this equipment not only ensures the safety and security of employees but also helps augment the performance and efficiency of health care centers (22). Emergency nurses need to learn how to use CBR-specific protective equipment, as wearing PPE can be cumbersome and putting them on for a long time creates excessive heat, which causes fatigue and discomfort in medical staff. In the case of the SARS respiratory disease epidemic, findings suggested that the long-term use of PPE undermined the appeal of this equipment, reducing the number of staff and health care professionals who were initially eager to use such equipment. Given that nurses are not sufficiently familiar with different types of PPE, practical training on how to use this equipment is essential because the improper utilization of PPE may harm medical staff. For instance, in certain cases such as intravenous cannulation, wearing butyl rubber gloves requires extensive practice, let alone visual restrictions associated with certain devices (20). On the other hand, all emergency staff, including specialists, doctors and nurses, and even service workers may find themselves at the forefront of a major chemical or biological terrorist incident. Therefore, learning how to use PPE should be specifically addressed in the training program (12). Also, the individuals in charge of PPE and the decontamination process must be adequately prepared for the initial operation. Personal protection levels are labeled as A to D where levels A and D offer the highest and lowest protection, respectively. Research shows that most hospitals in the world have C-level PPE (5). A study by Bennett suggested that more than half (59.5%) of hospitals did not have the resources to improve the capacity of equipment including devices, staff, patient beds, etc., lacking appropriate laboratory diagnostic services (91.9%) for the analysis and identification of WMDs (15). In another study, Sansom (32) reported that the availability of personal equipment such as the N95 mask can considerably protect staff from all known biological and radiological chemical threats. Protection against serious injuries by wearing double-layered gloves, disposable clothing or gowns, eye protection, surgical mask and, ideally, a helmet and shoe cover can mitigate the effects of CBRN accidents (33). Mortelmans et al. reported that only 6 hospitals had adequate protective equipment for triage and decontamination teams (12). In another study, Mortelmans et al. found that 32% of Dutch hospitals had satisfactory personal protective equipment for triage and decontamination teams (16).
4.4. Risk Perception
How people react to an emergency depends on their risk perception and their degree of vulnerability. Risk perception is vital for health and risk communication because it reveals the type of risks observed by people and how they are dealt with (33). Risk perception of accidents is seen as behavior consistent with risks, which can undermine adverse consequences of accidents. Researchers in the field of social sciences describe risk perception as the process of gathering, selecting, and interpreting signals about the uncertain effects of events, activities, or technologies. Research exhibits that social, economic, cultural characteristics along with the ideology and worldview of the people shape their beliefs about risk perception, such that risk perception varies across societies and cultures. In recent years’ pandemics, which affected a broad spectrum of people worldwide, the adopted strategies and outcomes call for enhanced risk perception of people in those areas. For example, authorities and people in different countries displayed different reactions to the inhibitions and quarantines put in place in the wake of infectious diseases such as SARS, influenza pandemic, swine flu epidemic and Covid-19 (34, 35).
The theory of rational choice and bounded rationality are the most relevant in the field of risk perception. According to this theory, people ascertain risks based on cost-benefit analysis (36). Assessment of staff’s perceptions of risk in different wards of hospitals calls for the adoption of reliable equipment that takes into account various dimensions such as training and learning, job motivation, family and social integration, workplace integrity, safety awareness and accident experience (37). Early response teams comprise police, firefighters, ambulances, paramedics, rescue workers and other emergency staff who respond to emergency cases with massive injuries or casualties, whether natural or man-made. Therefore, risk mitigation exercises are crucial to coping manage accidents characterized by massive losses, whether induced by human factors or CBRN agents (1). Guiding risk-taking decisions, risk perception is a vital behavioral factor before, during, and after a disaster. Human behavior in emergency management is influenced by risk perception, risk attitude, communication and aspects of risk management (38). Risk perception also substantially affects risk management, thus determining the success of risk management and reducing vulnerability. As such, risk perception management is an integral part of the disaster management process (1). Eyison et al. investigated the level of emergency care specialists’ awareness in two different centers for CBRN risks. The results suggested that the mean score of participants’ knowledge was 7.62 ± 3.92. There was also a significant difference (P < 0.05) between the mean knowledge scores of teaching and research hospitals (6.75 ± 3.97) and public hospitals (8.64 ± 3.65). Therefore, they concluded that health emergency specialists should be prepared for CBRN events and the level of health professionals’ awareness is the most objective measure of CBRN medical emergency preparedness, just like the global response to the COVID-19 pandemic (19).
4.5. Decontamination Centers
Decontamination is probably the cornerstone of managing the victims of CBRN accidents (17). Equipment, training and preparedness for the decontamination of chemically-infected victims are of utmost importance. As past chemical events have demonstrated, most disaster victims refer to hospitals unaccompanied. For instance, after the release of a nerve-damaging agent in the Tokyo subway in 1995, 640 patients infected with chemicals drove personally to the health care centers in the first few hours. Accordingly, 23% of emergency department staff were consequently infected (39). In addition, despite biological hazards, such as the release of biological weapons, decontamination plays a vital role in patient management (40). Decommissioning has been strongly recommended for biological agents such as anthrax spores, which can survive in the environment for decades (41). The hospital staff that performs triage and stabilization of patients should be thoroughly cognizant of the cases of decontamination and receive the necessary training on this subject (42). The decontamination facility should supply shelter, hot water and clothing for winter operations along with other necessary equipment. Indoor decontamination stations are usually reinforced with protections against hot and cold weather, which can be helpful for patients in certain situations, but its main drawback is that it lets infected patients and victims in the hospital (43). On the same vein, Wetter et al., after reviewing 186 emergency departments of hospitals in four northwestern states reported that about half of the wards (45%) have an internal or external decontamination unit with separate ventilation systems and showers (8). Bennett reported specific facilities for decontamination (75.7%) (15). In the study of Mortelmans et al., of 138 hospitals studied, only 11 had decontamination facilities in the emergency department (12). In another research by Mortelmans et al., of 93 hospitals studied, only 40% had access to decontamination facilities (16). In Treat et al.’s (2001) paper, 4 out of 30 hospitals in rural areas did not have any decontamination program in place (11).
4.6. Detection of CBRN Infection
The possible use of WMDs such as CBRNs is one of the most terrifying scenarios today and in the future. Therefore, it is indispensable to develop a general strategy for countermeasures. Developments in recent decades have clearly exhibited that the prompt and reliable detection, identification and monitoring of CBRN agents and their effects are increasingly becoming an instrumental technology at the international scale for mitigating and managing CBRN risk (44, 45). State-of-the-art technology must provide genuine and reliable detection capability that covers a wide range of CBRN targets across multiple environmental matrices by deploying a compatible system. Therefore, a major challenge in the future is the introduction of wisdom based diagnostic systems as well as the implementation of the international standard for CBRN quality management (44). Reliable detection technologies are necessary before, during and after a CBRN accident. Prior to a CBRN event, detectors can be used for ongoing monitoring to prevent CBRNs or issue an early warning in the event of an accident. During the CBRN, accident detectors are vital to evaluate the nature and extent of the CBRN agents. Hence, CBRN accident detectors perform three main tasks: (1) confirm the results of the initial detection; (2) gather evidence for the use of internationally banned substances, and (3) verify the safety of a zone after decontamination (46). In the study of Mortelmans et al., 6% of the hospitals had radiation detection equipment with an alarm function (12). The mechanism of triage in biological accidents differs from regular methods of triage. In a 2020 study by Aminizadeh et al., the majority of interviewees noted that most hospitals lacked the infrastructure necessary for the triage of infectious patients and that patients were not screened properly (6).
4.7. Availability of Drugs and Antidotes
Developing a technological platform to produce antidotes for CBRN medical protection as a primary medical approach is of paramount importance. Treatment of severe bleeding, respiratory tract complications, and respiratory problems is a priority that should be addressed by antidotes. Therefore, prescribing certain antidotes can be particularly helpful in the early stages. Pharmaceutical laboratories required to produce antidotes include drug control and quality assurance laboratory, chemical synthesis of pharmaceutical materials laboratory, microbiology laboratory for analysis and administration of pharmacological microbiology tests, medical and biosafety laboratories, laboratory of analyzing and conducting in-vivo experiments on animals, and R&D centers to apply their findings in the field of pharmacy. The technological platform to produce antidotes for CBRN medical protection can be developed at three scales, minimum, medium or maximum, depending on the existing needs and facilities (47). In the study of Treat et al., there was only a single specialized pharmaceutical center for the victims of WMDs (11). Wetter et al. investigated a hypothetical sarin gas toxicity scenario, finding that only 6% of hospitals had the minimum physical resources recommended to tackle and control sarin gas (8).
Hospitals were also inquired about other pharmaceutical inventories, with the results suggesting that their sciprofloxacin or doxycycline stock for 64 hypothetical anthrax victims was less than 64%. Also, 29% of hospitals had sufficient atropine for 50 hypothetical sarin victims, but no centers had enough pralidoxime (8). In the study of Bennett, pharmaceutical supplies available in hospitals were at best estimated at 56.8% (15). In Hsu et al.’s work, all 45 acute care hospitals in Maryland were surveyed and responses collected from 80% of hospitals were collected. Accordingly, about 92% of hospitals were prepared for biological disasters, 92% for chemical agents, and 67% for radiological agents. In addition, only 64% of hospitals had dedicated reserves for biological events, 67% for chemical events, and 50% for radiation events, signifying that hospitals struggle with the shortage of resources in a large-scale event (14). In the study of Mortelmans et al., atropine was accessible in all centers, but specific antidotes such as hydroxycobolamine, thiosulfate, or pralidoxime were available to a lesser degree (47%, 47%, and 19%, respectively) (12). Another research by Mortelmans et al. in the Netherlands found that high doses of atropine were accessible in all hospitals, but specific antidotes that could be helpful to victims of CBRN events, such as hydroxycobolamine, thiosulfate, Prussian blue, diethylenediaminetetraacetic acid (DTPA) or pralidoxime were in shortage (74, 65, 18, 14, and 42%, respectively) (16).
4.8. Availability of Specialists (Infectious, Emergency, etc.) and Health Workers
In different countries, the composition of the hospital team for CBRN disasters is different. In general, there is a multidisciplinary team consisting of emergency physicians, emergency nurses, toxicologists, infectious disease physicians, epidemiologists, infection control physicians, security forces, safety agents, pharmacists, hospital administrators, public relations officials, installations engineers, mental health physicians, coordinators of voluntary services, and health educators oversee CBRN domains (39). In addition, a specialized team is required for hospital planning in chemical accidents including staff in charge of emergency planning, emergency services, senior medical and nursing staff of the emergency department, emergency care physicians, specialist units, public health, occupational health, department of environment, the water company and the armed forces to assist at the time of CBRN disasters (27, 30). Also, in the wake of the past chemical events in the world, psychologists have established their pivotal role in the medical team because many victims (around 25%) need counseling following a chemical disaster. CBRN staff are abundantly concerned that they may contract an infectious disease and transit it to family, friends, and colleagues. Victims of hazardous materials or terrorist incidents, including chemical, biological, or radiation agents, driven by the fear of quarantine and isolation, guilt, anger, anxiety and depression, may experience post-traumatic stress disorder. In this regard, preliminary psychology sessions and interviews with patients and staff by psychologists should be a high priority (27, 48). Mortelmans et al. reported that 14% of hospitals had nuclear specialists around the clock during the week, while infectious disease specialists were only available in 26% of all emergency departments surveyed (12). In another study, they found that in the event of CBRN accidents, about 22.5% of Dutch hospitals have a nuclear specialist on site 24 hours a week, and 60% of hospitals regularly have infectious disease specialists on standby (16).
4.9. Limitations of Study
The findings of this review are limited by searched databases, time and language of publication. There may be some studies in old literature or other languages that were not entered into this analysis.
5. Conclusions
In this study, 17 articles on the preparedness of hospitals around the world for CBRN disasters were evaluated and subjected to analysis. The results suggested that none of the hospitals surveyed in the literature were fully capable of dealing with CBRN accidents and needed improvement in a broad range of areas such as training and staffing, disaster planning, personal protective equipment, risk perception, decontamination of departments and wards, CBRN contamination detection, availability of drugs and antidotes, and the presence of health professionals and staff in the ward, among other things. Therefore, the present study can paint a clear picture of plans undertaken by officials and policymakers at the Ministry of Health to better handle CBRN incidents.
Acknowledgements
References
-
1.
Yücel H, Cengiz S. Assessment of the Relationship Between the Risk Perception and Preparedness Attitudes of Search & Rescue and Firefighting Teams Against Event Site Hazards in CBRN Events: Adana Province Case. Gumushane Univ J Soc Sci. 2020;11(Ek):347-54.
-
2.
Carter H, Drury J, Amlôt R. Recommendations for improving public engagement with pre-incident information materials for initial response to a chemical, biological, radiological or nuclear (CBRN) incident: A systematic review. Int J Disaster Risk Reduct. 2020;51:101796. https://doi.org/10.1016/j.ijdrr.2020.101796.
-
3.
Collins S, James T, Carter H, Symons C, Southworth F, Foxall K, et al. Mass Casualty Decontamination for Chemical Incidents: Research Outcomes and Future Priorities. Int J Environ Res Public Health. 2021;18(6). [PubMed ID: 33802722]. [PubMed Central ID: PMC8002470]. https://doi.org/10.3390/ijerph18063079.
-
4.
Carter H, Amlôt R. Mass Casualty Decontamination Guidance and Psychosocial Aspects of CBRN Incident Management: A Review and Synthesis. PLoS Currents. 2016. https://doi.org/10.1371/currents.dis.c2d3d652d9d07a2a620ed5429e017ef5.
-
5.
Tan GA, Fitzgerald MC. Chemical-biological-radiological (CBR) response: a template for hospital emergency departments. Med J Aust. 2002;177(4):196-9. [PubMed ID: 12175324]. https://doi.org/10.5694/j.1326-5377.2002.tb04732.x.
-
6.
Aminizadeh M, Farrokhi M, Ebadi A, Masoumi G, Kolivand P, Khankeh H. Hospital Preparedness Challenges in Biological Disasters: A Qualitative Study. Disaster Med Public Health Prep. 2020:1-5. [PubMed Central ID: PMC7900656]. https://doi.org/10.1017/dmp.2020.434.
-
7.
Ahmadi Marzaleh M, Rezaee R, Rezaianzadeh A, Rakhshan M, Haddadi G, Peyravi M. Emergency Department Preparedness of Hospitals for Radiation, Nuclear Accidents, and Nuclear Terrorism: A Qualitative Study in Iran. Iran Red Crescent Med J. 2019;21.
-
8.
Wetter DC, Daniell WE, Treser CD. Hospital preparedness for victims of chemical or biological terrorism. Am J Public Health. 2001;91(5):710-6. [PubMed ID: 11344876]. [PubMed Central ID: PMC1446687]. https://doi.org/10.2105/ajph.91.5.710.
-
9.
Aminizadeh M, Farrokhi M, Ebadi A, Masoumi GR, Kolivand P, Khankeh HR. Hospital management preparedness tools in biological events: A scoping review. J Educ Health Promot. 2019;8:234. [PubMed ID: 31867398]. [PubMed Central ID: PMC6905292]. https://doi.org/10.4103/jehp.jehp_473_19.
-
10.
Noorihekmat S, Rahimi H, Mehrolhassani MH, Chashmyazdan M, Haghdoost AA, Ahmadi Tabatabaei SV, et al. Frameworks of Performance Measurement in Public Health and Primary Care System: A Scoping Review and Meta-Synthesis. Int J Prev Med. 2020;11:165. [PubMed ID: 33312474]. [PubMed Central ID: PMC7716605]. https://doi.org/10.4103/ijpvm.IJPVM_34_19.
-
11.
Treat KN, Williams JM, Furbee PM, Manley WG, Russell FK, Stamper CJ. Hospital preparedness for weapons of mass destruction incidents: an initial assessment. Ann Emerg Med. 2001;38(5):562-5. [PubMed ID: 11679869]. https://doi.org/10.1067/mem.2001.118009.
-
12.
Mortelmans LJ, Van Boxstael S, De Cauwer HG, Sabbe MB, Belgian Society of E, Disaster Medicine S. Preparedness of Belgian civil hospitals for chemical, biological, radiation, and nuclear incidents: are we there yet? Eur J Emerg Med. 2014;21(4):296-300. [PubMed ID: 23978957]. https://doi.org/10.1097/MEJ.0000000000000072.
-
13.
Jasper E, Miller M, Sweeney B, Berg D, Feuer E, Reganato D. Preparedness of hospitals to respond to a radiological terrorism event as assessed by a full-scale exercise. J Public Health Manag Pract. 2005;Suppl:S11-6. [PubMed ID: 16205528]. https://doi.org/10.1097/00124784-200511001-00003.
-
14.
Hsu EB, Casani JA, Romanosky A, Millin MG, Singleton CM, Donohue J, et al. Critical assessment of statewide hospital pharmaceutical surge capabilities for chemical, biological, radiological, nuclear, and explosive incidents. Prehosp Disaster Med. 2007;22(3):214-8. [PubMed ID: 17894215]. https://doi.org/10.1017/s1049023x00004696.
-
15.
Bennett RL. Chemical or biological terrorist attacks: an analysis of the preparedness of hospitals for managing victims affected by chemical or biological weapons of mass destruction. Int J Environ Res Public Health. 2006;3(1):67-75. [PubMed ID: 16823078]. [PubMed Central ID: PMC3785681]. https://doi.org/10.3390/ijerph2006030008.
-
16.
Mortelmans LJM, Gaakeer MI, Dieltiens G, Anseeuw K, Sabbe MB. Are Dutch Hospitals Prepared for Chemical, Biological, or Radionuclear Incidents? A Survey Study. Prehosp Disaster Med. 2017;32(5):483-91. [PubMed ID: 28478772]. https://doi.org/10.1017/S1049023X17006513.
-
17.
Ahmadi Marzaleh M, Rezaee R, Rezaianzadeh A, Rakhshan M, Haddadi G, Peyravi M. Developing a Model for Hospitals' Emergency Department Preparedness in Radiation and Nuclear Incidents and Nuclear Terrorism in Iran. Bull Emerg Trauma. 2019;7(3):300-6. [PubMed ID: 31392231]. [PubMed Central ID: PMC6681888]. https://doi.org/10.29252/beat-0703014.
-
18.
Azeem AR, Sharif MW, Akhtar A, Sohail CS, Dar AA, Khan M, et al. Perception of Preparedness of Health Care Professionals in Case of a Nuclear, Chemical, Biological Attack/Emergency in a Tertiary Care Hospital. Cureus. 2019;11(5). e4657. [PubMed ID: 31328050]. [PubMed Central ID: PMC6634288]. https://doi.org/10.7759/cureus.4657.
-
19.
Eyison RK, Pakdemirli A, Aydin E, Sayin Ozturk A, Kiliç Z, Demirbag B, et al. Evaluation of the Medical Chemical, Biological, Radiological, and Nuclear Awareness Level of Emergency Healthcare Professionals Serving on Different Centres. J Basic Clin Health Sci. 2020;4(2):174-9. https://doi.org/10.30621/jbachs.2020.1037.
-
20.
Luther M, Lenson S, Reed K. Issues associated in chemical, biological and radiological emergency department response preparedness. Aust Emerg Nurs J. 2006;9(2):79-84. https://doi.org/10.1016/j.aenj.2006.03.007.
-
21.
Candiotti KA, Kamat A, Barach P, Nhuch F, Lubarsky D, Birnbach DJ. Emergency preparedness for biological and chemical incidents: a survey of anesthesiology residency programs in the United States. Anesth Analg. 2005;101(4):1135-40. [PubMed ID: 16192534]. https://doi.org/10.1213/01.ane.0000167642.11429.f5.
-
22.
Mitchell CJ, Kernohan WG, Higginson R. Are emergency care nurses prepared for chemical, biological, radiological, nuclear or explosive incidents? Int Emerg Nurs. 2012;20(3):151-61. [PubMed ID: 22726947]. https://doi.org/10.1016/j.ienj.2011.10.001.
-
23.
Alahmari AA, Khan AA. Chemical, biological, radiological, and nuclear preparedness of public hospitals in Riyadh. Research Square. 2020. https://doi.org/10.21203/rs.3.rs-104590/v1.
-
24.
Dowlati M, Seyedin H, Moslehi S. Hospital Preparedness Measures for Biological Hazards: A Systematic Review and Meta-Synthesis. Disaster Med Public Health Prep. 2021;15(6):790-803. [PubMed ID: 32713417]. https://doi.org/10.1017/dmp.2020.132.
-
25.
Eitzen EM. Education Is the Key to Defense Against Bioterrorism. Ann Emerg Med. 1999;34(2):221-3. https://doi.org/10.1016/s0196-0644(99)70233-7.
-
26.
Moradi Majd P, Seyedin H, Bagheri H, Tavakoli N. Hospital Preparedness Plans for Chemical Incidents and Threats: A Systematic Review. Disaster Med Public Health Prep. 2020;14(4):477-85. [PubMed ID: 31610820]. https://doi.org/10.1017/dmp.2019.91.
-
27.
Chan JT, Yeung RS, Tang SY. Hospital preparedness for chemical and biological incidents in Hong Kong. Hong Kong Med J. 2002;8(6):440-6. [PubMed ID: 12459601].
-
28.
Olivieri C, Ingrassia PL, Della Corte F, Carenzo L, Sapori JM, Gabilly L, et al. Hospital preparedness and response in CBRN emergencies: TIER assessment tool. Eur J Emerg Med. 2017;24(5):366-70. [PubMed ID: 27058684]. https://doi.org/10.1097/MEJ.0000000000000399.
-
29.
Watson A, Hall L, Raber E, Hauschild VD, Dolislager F, Love AH, et al. Developing Health-Based Pre-Planning Clearance Goals for Airport Remediation Following a Chemical Terrorist Attack: Decision Criteria for Multipathway Exposure Routes. Hum Ecol Risk Assess. 2011;17(1):57-121. [PubMed Central ID: PMC3046627]. https://doi.org/10.1080/10807039.2010.534722.
-
30.
Veenema TG. Chemical and biological terrorism preparedness for staff development specialists. J Nurses Staff Dev. 2003;19(5):218-25. quiz 226-7. [PubMed ID: 14581829]. https://doi.org/10.1097/00124645-200309000-00001.
-
31.
Joint Commission Resources I. Emergency management in health care: An all-hazards approach. Illinois, USA: Joint Commission Resources; 2012.
-
32.
Sansom GW. Emergency department personal protective equipment requirements following out-of-hospital chemical biological or radiological events in Australasia. GEmerg Med Australas. 2007;19(2):86-95. [PubMed ID: 17448093]. [PubMed Central ID: PMC7163549]. https://doi.org/10.1111/j.1742-6723.2007.00927.x.
-
33.
Eugene AR. White, Black, and Gray: Critical Dialogue with the International Risk Governance Council's Framework for Risk Governance. Global risk governance. 1. Netherlands: Springer; 2008. p. 101-18. https://doi.org/10.1007/978-1-4020-6799-0_5.
-
34.
Yeung NCY, Lau JTF, Choi KC, Griffiths S. Population Responses during the Pandemic Phase of the Influenza A(H1N1)pdm09 Epidemic, Hong Kong, China. Emerg Infect Dis. 2017;23(5):813-5. [PubMed ID: 28418300]. [PubMed Central ID: PMC5403031]. https://doi.org/10.3201/eid2305.160768.
-
35.
Farnoosh G, Alishiri G, Hosseini Zijoud SR, Dorostkar R, Jalali Farahani A. Understanding the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and Coronavirus Disease (COVID-19) Based on Available Evidence - A Narrative Review. Mil Med. 2020;22(1):1-11. https://doi.org/10.30491/jmm.22.1.1.
-
36.
Ejeta LT, Ardalan A, Paton D. Application of Behavioral Theories to Disaster and Emergency Health Preparedness: A Systematic Review. PLoS Curr. 2015;7. [PubMed ID: 26203400]. [PubMed Central ID: PMC4494855]. https://doi.org/10.1371/currents.dis.31a8995ced321301466db400f1357829.
-
37.
Soori S, Sebt MH, Ardeshir A. [Risk perception assessment and its related factors among construction workers]. J Safety Promot Injury Prev. 2017;4(4):261-8. Persian.
-
38.
Rohrmann B. Risk perception, risk attitude, risk communication, risk management: A conceptual appraisal. Melbourne, Australia: University of Melbourne; 2008.
-
39.
White S. Hospital and emergency department preparedness for biologic, chemical, and nuclear terrorism. Clin Occup Environ Med. 2002;2(2):405-25. https://doi.org/10.1016/s1526-0046(02)00028-6.
-
40.
Macintyre AG, Christopher GW, Eitzen EJ, Gum R, Weir S, DeAtley C, et al. Weapons of mass destruction events with contaminated casualties: effective planning for health care facilities. JAMA. 2000;283(2):242-9. [PubMed ID: 10634341]. https://doi.org/10.1001/jama.283.2.242.
-
41.
Lepler L, Lucci E. Responding to and managing casualties: detection, personal protection, and decontamination. Respir Care Clin N Am. 2004;10(1):9-21. https://doi.org/10.1016/s1078-5337(03)00046-7.
-
42.
Rinnert KJ. Local perspectives on bioterrorism. An approach to terrorism preparedness: Parkland Health and Hospital System. Proc (Bayl Univ Med Cent). 2001;14(3):231-5. [PubMed Central ID: PMC1305822].
-
43.
Schultz CH, Mothershead JL, Field M. Bioterrorism preparedness: The emergency department and hospital. Emerg Med Clin N Am. 2002;20(2):437-55. https://doi.org/10.1016/s0733-8627(02)00003-2.
-
44.
Hülseweh B, Marschall H, Rambousky R, Richardt A. Why Are Reliable CBRN Detector Technologies Needed? CBRN Protection: Managing the Threat of Chemical, Biological, Radioactive and Nuclear Weapons. Wiley; 2013. p. 167-78. https://doi.org/10.1002/9783527650163.ch6.
-
45.
Eubanks LM, Dickerson TJ, Janda KD. Technological advancements for the detection of and protection against biological and chemical warfare agents. Chem Soc Rev. 2007;36(3):458-70. [PubMed ID: 17325785]. https://doi.org/10.1039/b615227a.
-
46.
Reutter D, Schutzer SE, Craft CM, Fletcher J, Fricke FL, Holowachuk SA, et al. Planning for exercises of chemical, biological, radiological, and nuclear (CBRN) forensic capabilities. Biosecur Bioterror. 2010;8(4):343-55. [PubMed ID: 21142761]. https://doi.org/10.1089/bsp.2010.0023.
-
47.
Ordeanu V, Popescu D, Necsulescu M, Ionescu L, Popa A, Sandulovici R. Concepts for the implementation of a technological platform for the production of specific antidotes for CBRN medical protection. Rom J Mil Med. 2021;124(1):61-6. https://doi.org/10.55453/rjmm.2021.124.1.8.
-
48.
Loutfy MR, Wallington T, Rutledge T, Mederski B, Rose K, Kwolek S, et al. Hospital preparedness and SARS. Emerg Infect Dis. 2004;10(5):771-6. [PubMed ID: 15200807]. [PubMed Central ID: PMC3323236]. https://doi.org/10.3201/eid1005.030717.
