Abstract
Background:
Out-of-pocket payments for medical services may undermine access to medical services and equity in healthcare financing.Objectives:
The present study aimed to determine the distribution of the burden of out-of-pocket payments for healthcare services among the households in Qazvin province, Iran.Methods:
This descriptive-analytical study was conducted on the urban and rural households in Qazvin province, Iran during 2019 - 2020. Data were obtained from the Statistics Center of Iran (2019 - 2020). The optimal sample size was calculated to be 992 households, and the households were selected via three-stage random cluster sampling. Data were collected using a valid questionnaire and via face-to-face interviews with the household owners. The fair financial contribution index (FFCI), concentration index, and Kakwani index were estimated in the Stata software.Results:
The estimated parameters indicated that during the study period (March 21, 2019-March 20, 2020), the FFCI value of the rural and urban households was 0.782 and 0.854, respectively. The out-of-pocket payment concentration index based on income rank was estimated at 0.188 in rural households (P < 0.05) and 0.031 in the urban households. In addition, the Kakwani index of the urban and rural households was calculated to be -0.165 and -0.84, respectively.Conclusions:
According to the results, out-of-pocket payments were unequally distributed among the households in Qazvin province in 2019 - 2020. These payments were mostly concentrated on the 5th - 7th deciles of urban households. On the other hand, the out-of-pocket payments during the study period were regressive. To promote financial equity, Qazvin health policymakers must run payment exemptions for low-income groups and also expand the medical insurance coverage and universal coverage of healthcare services.Keywords
Equity in Financing Out-of-Pocket, Health Expenses Concentration Index Kakwani Index Fair Financial Contribution Index
1. Background
Out-of-pocket payments are a common approach to the financing of the health sector in developing countries. Any payment made by an individual upon receiving a healthcare service or health product is referred to as an out-of-pocket payment (1). Out-of-pocket financing accounts for a larger share of poor household income than non-poor households. If low-income individuals pay a larger share of their income as out-of-pocket expenses than well-paid individuals, health financing becomes regressive (2).
High levels of out-of-pocket payments for healthcare expose households to the financial risks of severe illnesses. On the other hand, excessive reliance on out-of-pocket payments for healthcare may jeopardize the normal living standards of households and disrupt wellbeing (3, 4). High out-of-pocket payments may also deter some individuals from seeking the healthcare and create barriers to access healthcare in underprivileged groups (5, 6). These payments are known to be associated with the underutilization of healthcare services (7-10).
According to the World Health Organization (WHO) in 2015, the average share of out-of-pocket payments in the current health expenditures in the Eastern Mediterranean countries was close to 41% (11). Empirical studies have also indicated a strong correlation between the incidence of catastrophic and impoverishing health expenditures and the share of out-of-pocket payments of the current health expenditures (12). In Iran, patients pay part of the medical expenditure upon receiving medical services as an out-of-pocket payment.
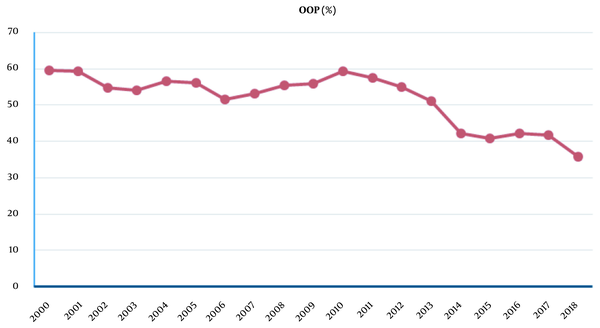
According to the World Bank data, the average percentage of out-of-pocket payments during 2000 - 2018 in Iran was 51.72% (13). As is depicted in Figure 1, the trend of out-of-pocket payments declined during this period. In a health system, the percentage of out-of-pocket payments and its distribution modality among various income groups are important indicators for assessing the financial equity of the system. The first step in moving the health sector toward equity in financing is that policymakers have credible empirical evidence on the distribution of health spending among various populations. Before taking any remedial action, health policymakers must be aware of the exact distribution of out-of-pocket payments. An appropriate method for determining the progressivity of financing systems is the use of the indicators that represent payments based on the proportion of income (14).
Trend of household out of pockets percentage
Research in different countries has shown that the most direct payments for health services are imposed on poor, low-income, marginalized, and rural groups. To confirm this claim, a study was conducted in Turkey to evaluate the distribution of inequality in healthcare financing in different deciles of the community using the relevant indicators. According to the obtained results, the distribution of direct out-of-pocket payment placed more pressure on vulnerable community groups (15). In India, those living in urban slums and rural households receive more direct out-of-pocket payments compared to other community groups while receiving healthcare services (16).
In Iran, Darvishi et al. conducted a systematic review of the studies published during 2008 - 2018 using the fair financial contribution index (FFCI), reporting more inequalities in the distribution of direct out-of-pocket payments in rural areas compared to urban areas before and after the implementation of the health system transformation plan (17). In another study performed in Qazvin province (Iran), Keshavarz et al. estimated the direct out-of-pocket payments for treatment costs, estimating the average out-of-pocket payments for total medical expenses to be 59.7%. In the mentioned study, low-income deciles (first decile) accounted for a significant percentage of household income (19%) (18).
2. Objectives
After the implementation of the health system transformation plan, this is the first study conducted in Qazvin province (Iran) to comprehensively evaluate the distribution of direct out-of-pocket payments for healthcare services in urban and rural households. The present study aimed to address the following questions:
- What is the value of Rials and percentage of out-of-pocket payments in the households of Qazvin province?
- What is the status of the fair financial participation index in the out-of-pocket payments of the households in Qazvin province?
- What is the concentration index in the out-of-pocket payments of the households in Qazvin province?
- What is the role of economic and social factors in the out-of-pocket payments of the households in Qazvin province?
- Are out-of-pocket payments higher in the rural households or urban households?
The contributions of our study could be summarized, as follows:
- Our study is the first investigation of payment equity in Qazvin province.
- We investigated the equity of out-of-pocket payments in the households in Qazvin province by estimating various indicators.
Our findings could lay the groundwork for determining the level of direct out-of-pocket payment justice in the households of Qazvin province and establishing correct strategies and policymaking based on the awareness of the current state of health system managers.
3. Methods
The present study aimed to investigate the equity of out-of-pocket payments in the urban and rural households of Qazvin province during 2019 - 2020. Initially, a sample of 992 households was selected from the urban and rural population of Qazvin province based on the data obtained from the Statistics Center of Iran (SCI) via three-stage random cluster sampling.
Data were collected using the valid expenditure and income questionnaire of SCI. The samples were selected in three stages using probabilistic sampling methods. In the first step, sample clusters were selected in each base sample class via simple random sampling. At the second stage, rotation groups were formed in each sample cluster based on the rotation pattern and determined for counting. In the third step, the sample households within each rotation group were selected. To calculate the sample size, we used the SCI formula, as follows:
In the formula above, t is the index of the province, c shows the index of the interest variable (i.e., health expenditures), n is the number of the samples, Z0.975 shows the 0.975 quintile of standard normal distribution (= 1.96), S is the standard deviation, Nr represents the assumed sample loss rate (= 0.1), r is the relative error accepted for estimating the mean,
For data collection, the technicians of the SCI interviewed an eligible member of the selected households in a face-to-face manner and completed the questionnaire. Data analysis was performed in the Stata software, and the values of the FFCI, concentration index (CI), and Kakwani index (KI) were calculated separately for the rural and urban populations in cost quintiles. Percentage, frequency, mean, and standard deviation were used for the descriptive analysis of the demographic data and the calculation of the FFCI and KI.
3.1. Index Calculation
The FFCI reflects the inequality in household financing contribution, as well as the distribution of the out-of-pocket expense share of the household. The range of FFCI change is 0 - 1; if its value is equal to one, it indicates that the out-of-pocket payment share is perfectly equal among the sample households, while the zero value indicates complete inequality (19). In the present study, the FFCI was calculated using the following formula:
OOPCTPh shows the total direct payments of the households for healthcare services (OOPh), divided by the capacity to pay (CTPh) and oopctp0=∑whooph ∑whctph.
The size of the CI is twice the area enclosed between the concentration curve and the 45-degree line. The concentration curve shows the distribution of the cumulative out-of-pocket share among the households as sorted by income, literacy level, and age of the household head. The range of CI is -1-+1; if the CI is equal to +1, 100% of the out-of-pocket expenditure is paid by high-income households. If it is equal to -1, it indicates that 100% of out-of-pocket payments are concentrated on the poorest households, and the zero value shows the completely equal distribution of out-of-pocket payments (20).
The KI measures the progressiveness of out-of-pocket payments for healthcare services. The KI value is within the range of -2-+1; if the value is closer to -2, out-of-pocket payments are more regressive. If the value of the index is equal to one, it indicates that out-of-pocket payments are fully progressive. The KI is measured by doubling the area of the distance between the Lorenz curve and the concentration curve (21).
The standard CI is the least-squares estimate of α1 in the following model:
where
4. Results
Table 1 shows the demographic characteristics of the urban and rural households. Out of the 420 urban households, 87.38% were managed by men, and 12.62% were managed by women. Out of the 572 rural households, 85.11% were managed by men, and 14.89% were managed by women. Among the urban households, 86.90% of the heads were married, and 13.10% were single. As for the rural households, 83.92% of the heads were married, and 16.08% were single.
Demographic Characteristics of Household’s Head Economic Characteristics of Households (in Rial 2019/2020) a
| Variable | Urban | Rural |
|---|---|---|
| Gender | ||
| Male | 367 (87.38) | 487 (85.11) |
| Female | 53 (12.62) | 85 (14.89) |
| Marital status | ||
| Married | 365 (86.90) | 480 (83.92) |
| Single | 55 (13.10) | 92 (16.08) |
| Employment status | ||
| Employed | 272 (64.76) | 401 (70.10) |
| Unemployed | 148 (35.24) | 171 (20.90) |
| Literacy | ||
| Literate | 356 (84.76) | 402 (70.28) |
| Illiterate | 64 (15.24) | 170 (29.72) |
| Size of household | 3.18 ± 1.24 | 3.21 ± 1.37 |
| Age of head | 50 ± 15.67 | 52 ± 16.14 |
Among the urban households, 64.76% of the heads were employed, and 35.24% were unemployed. As for the rural households, 70.10% of the heads were married, and 29.90% were single. Among the urban households, 84.76% of the heads were literate, and 15.24% were illiterate. As for the rural households, 70.10% of the heads were literate, and 29.90% were illiterate. The mean size of the urban and rural households was 3.18 ± 1.24 and 3.21 ± 1.37, respectively, and the mean age of the household head was 50 ± 15.67 and 52 ± 16.14 years, respectively.
Table 2 shows the economic status of the studied households. The mean out-of-pocket payment of the urban and rural households was 1,450,000 and 1,137,804 Rials, respectively. In addition, the urban and rural households paid 1.19% and 5.65% of their monthly income out-of-pocket for healthcare services, respectively. The share of the out-of-pocket payments from the monthly expenditure of the urban and rural households was estimated at 2.3% and 8.35%, respectively.
Economic Characteristics of Households (in Rial 2019/2020)
| Variable | Mean | |
|---|---|---|
| Urban | Rural | |
| Income per month | 121,308,300 | 20,113,317 |
| Total expenditure per month | 48,631,421 | 13,629,269 |
| OOP expenditure per month | 1,450,000 | 1,137,804 |
| OOP/TE (%) | 2.3 | 8.35 |
| OOP/I (%) | 1.19 | 5.65 |
According to the information in Table 3, the FFCI value of the rural and urban households was 0.782 and 0.854, respectively. Among the urban households, the highest FFCI value belonged to the first quintile (0.902), while it belonged to the third quintile (0.848) in the rural households. On the other hand, the lowest FFCI value in the urban households was in the fourth quintile (0.831), while it was in the fourth quintile (0.796) in the rural households. Among the rural households, the highest value (-0.350) of this index was in the first quintile, and the lowest value (-0.036) was in the second quintile. As for the urban households, the highest value of KI (-1.218) was observed in the second quintile, and the lowest value (-0.299) was in the fifth quintile.
Equity Indices by Expenditure Quintile
| Indices | Total | 1st Quintile | 2nd Quintile | 3rd Quintile | 4th Quintile | 5th Quintile |
|---|---|---|---|---|---|---|
| Rural households | ||||||
| FFCI | 0.782 | 0.821 | 0.799 | 0.848 | 0.796 | 0.811 |
| KI | -0.165 | -0.350 | -0.036 | -0.272 | -0.206 | -0.232 |
| Urban households | ||||||
| FFCI | 0.854 | 0.902 | 0.830 | 0.855 | 0.831 | 0.876 |
| KI | -0.84 | -0.433 | -1.218 | -0.36 | -0.381 | -0.299 |
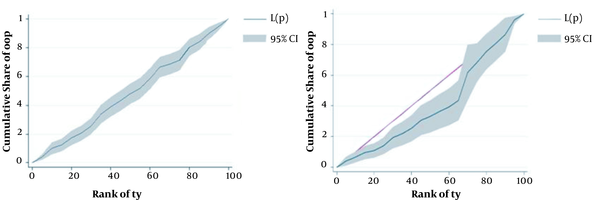
According to the information in Table 4, the CI of the out-of-pocket payments of the rural households was 0.188 (P < 0.05). As for the urban households, the CI value was calculated to be 0.031. Figure 2 illustrates the out-of-pocket payment concentration curves of the urban and rural households. In the rural households, the distribution of the cumulative out-of-pocket share based on the income status was dominant in the deciles 5 - 7 (households with above average income; P < 0.05), while the distribution was rather symmetric in the urban households.
Concentration Indices by Household Type
| Indices | N | Value | Std. Error | P-Value | |
|---|---|---|---|---|---|
| Rural households | CIy | 572 | 0.188 | 0.085 | 0.027 |
| Urban households | CIy | 420 | 0.031 | 0.041 | 0.461 |
Distribution of cumulative share of out-of-pocket payments based on the income rank of the household (Left: Urban households and right: Rural households)
5. Discussion
The present study aimed to assess the equity of out-of-pocket payments in the households of Qazvin province. The obtained results regarding the FFCI indicated mild inequality in the out-of-pocket payments of the rural and urban households. Notably, the intensity of inequality was below average, while inequality was higher in the rural households compared to the urban households.
Ample empirical evidence is available regarding the out-of-pocket payments of the households in Iran. In line with our findings, Na’emani et al. calculated the FFCI of a 10 year period to be above 0.5 in Iran, indicating slight inequality in the household health expenditure (19). In the study conducted by Mehrara et al., the estimation of the FFCI demonstrated that inequality was mild in urban and rural households during the study period, while the value of the index decreased and led to higher inequality (22). Mohammadzadeh et al in their study in 2017 indicated the small inequality in out-of-pocket payments among Iranian households (23).
Contrary to our findings, the results of the study by Darvishi et al. indicated that inequality in the distribution of household health expenditures was high in 2009 and 2010 (17). However, the mentioned study confirmed that after the implementation of the health transformation plan, inequality decreased and reached a low level. In line with the results of the present study, Na’emani et al. also observed that the inequality of health expenditures in rural households was higher compared to urban households (19). Meanwhile, Yahyavidizaj et al. also confirmed this inequality between urban and rural areas (24). One of the reasons for the greater inequality in rural areas may be that rural households have a poor coverage by medical insurance.
In Iran, changes in the health system have been implemented through the health system development plan, which consists of eight healthcare packages and initiated in 2014 to advance targets (the first aid package in the project) and decrease payments by patients in the hospitals affiliated to the Iranian Ministry of Health and Medical Education (25). In the law of the Fourth National Development Plan, the distribution of resources and healthcare facilities should not involve an increase of more than 30% in people’s share in the total health expenditures (26). Our findings and the previous studies in this regard indicate that the health sector has not yet been able to achieve the goal of the Fourth National Development Plan and the implicit purpose of the Health Transformation Plan. Evidently, the rate of household out-of-pocket payments has decreased in recent years, which could facilitate achieving the goal of the Fourth Development Plan. Conclusions must be drawn cautiously since the decline in out-of-pocket payments may be due to a drop in the real demand for medical services. Furthermore, analyzing the trend of the actual consumption data of healthcare services may clarify the issue.
In the present study, the estimates of the CI in the urban households showed that the share of out-of-pocket payments was unequally distributed among the income deciles, while the inequality was not considered significant. Notably, the CI varied among the expenditure quintiles. The cumulative share of out-of-pocket payments was also unequally distributed among the rural households. In other words, the cumulative out-of-pocket share was concentrated on deciles 5 - 7. In these households, the highest inequality based on the CI was observed in the second quintile. In this regard, Ghafoori et al. also concluded that the distribution of inpatient payments among the households in Tehran (Iran) imposed no financial burden on privileged social classes (27).
In line with the results of the present study, another research in the Iran showed that in 2015, more medical expenditures were paid by high-income households (28). In addition, the results obtained by Nakovics et al. indicated a positive correlation between wealth quarters and out-of-pocket payments (29). Contrary to our findings, Rezapour et al. estimated the CI of the households in Kerman (Iran), concluding that the least privileged classes paid a higher percentage of health expenditures (30). The results obtained by Ghafoori et al. also revealed that outpatient expenditures were concentrated on below average income deciles (27). According to the study by Dalui et al. in India, the concentration of catastrophic expenditure was higher among poorer households (31). One of the reasons for the discrepancy between our findings and the aforementioned studies may be the difference in medical insurance coverage between the studied populations. Poor medical insurance coverage imposes the burden of out-of-pocket payments on the lower income deciles. Differences in demanded services may be another reason for the differences between the findings in this regard.
In the current research, the estimation of the KI indicated that in the rural and urban households, out-of-pocket payments were regressive during the study period, which signifies a vertical inequity in the out-of-pocket payments for medical services. In the urban households, payment regression was more severe compared to the rural households. Consistent with our findings, the results obtained by Kazemian et al. showed that out-of-pocket payments for medical services were regressive in 2014 (21). Contrary to our findings, the results obtained by Yahyavidizaj et al. indicated that in rural and urban areas, the out-of-pocket payments for medical services were progressive during 2015 - 2016 (24). One of the possible reasons for the progressiveness of payments could be the short-term impact of the Health Transformation Plan since user fees decreased after the implementation of this plan, especially for rural residents. In another study, Pourasghari et al. reported that out-of-pocket payments were regressive in urban areas and progressive in rural areas during 2006 - 2011 (32). In addition, Zare et al. concluded that household health expenditures were progressive during 1984 - 2010 (33).
Comparison of the aforementioned studies with our findings shows that household payments for healthcare services in Iran have become regressive in recent years, which may be due to the effect of inflation on healthcare expenditures. Rising inflation, along with declining effective medical insurance coverage, have caused low-income populations to pay more of their medical costs out-of-pocket. A general approach to improving equity in household healthcare payments is to reduce out-of-pocket payments. Evidence on the distribution of out-of-pocket payments among social and economic subgroups could help health policymakers adopt effective policies to promote the equity of health sector financing; such examples are payment exemptions, targeted health subsidies, and targeted healthcare coverage. Furthermore, health policymakers could make out-of-pocket payments more equitable through the comprehensive development of prepayment mechanisms, payment exemptions for vulnerable groups, targeted subsidies for low-income groups, and the control of health sector inflation.
5.1. Limitations of the Study
Due to the lack of valid data on the actual use of medical services, we were unable to examine the distribution of out-of- pocket payments by matching demand quantity among households, which is one of the limitations of our study. In addition, we could not investigate the role of separate factors affecting the inequality of payments due to the lack of access to comprehensive data on the socioeconomic characteristics of the households. Since we did not have access to all the demographic characteristics of the households, only a few demographic variables were analyzed. Further studies could provide stronger evidence by considering these limitations.
5.2. Conclusions
According to the results, a slight inequality occurred in the distribution of out-of-pocket payments during March 21, 2019-March 20, 2020. Inequality was higher in the rural areas compared to the urban areas, while the rate varied among different expenditure quintiles. In the rural households, the distribution of the cumulative out-of-pocket share was concentrated on deciles 5 - 7. Meanwhile, the cumulative share of out-of-pocket payments was almost equally distributed in the urban households. In the study period, out-of-pocket payments were regressive, and the regression was more severe in the urban areas compared to the rural areas. Therefore, the health policymakers of Qazvin should identify low-income deciles, implement out-of-pocket payment exemptions for these deciles, and improve the insurance coverage and universal coverage of medical services in order to make the distribution of out-of-pocket payments more equitable, especially in rural households.
Acknowledgements
References
-
1.
World Health Organization. The world health report, health systems: Improving performance. Geneva: World Health Organization; 2000. 215 p p.
-
2.
Wagstaff A, Flores G, Smitz M, Hsu J, Chepynoga K, Eozenou P. Progress on impoverishing health spending in 122 countries: A retrospective observational study. Lancet Glob Health. 2018;6(2):e180-92. https://doi.org/10.1016/s2214-109x(17)30486-2.
-
3.
Wagstaff. The economic consequences of health shocks: evidence from Vietnam. J Health Econ. 2007;26(1):82-100. [PubMed ID: 16905205]. https://doi.org/10.1016/j.jhealeco.2006.07.001.
-
4.
van Doorslaer E, O'Donnell O, Rannan-Eliya RP, Somanathan A, Adhikari SR, Garg CC, et al. Catastrophic payments for health care in Asia. Health Econ. 2007;16(11):1159-84. [PubMed ID: 17311356]. https://doi.org/10.1002/hec.1209.
-
5.
Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, Evans T. Protecting households from catastrophic health spending. Health Aff (Millwood). 2007;26(4):972-83. [PubMed ID: 17630440]. https://doi.org/10.1377/hlthaff.26.4.972.
-
6.
Chen WY. The welfare effect of co-payment adjustments on emergency department visits in medical centers: Evidence from Taiwan. Health Policy. 2020;124(11):1192-9. [PubMed ID: 32653233]. https://doi.org/10.1016/j.healthpol.2020.03.013.
-
7.
Sia D, Dondbzanga BDG, Carabali M, Bonnet E, Enok Bonong PR, Ridde V. Effect of a free healthcare policy on health services utilisation for non-malarial febrile illness by children under five years in Burkina Faso: An interrupted time series analysis. Trop Med Int Health. 2020;25(10):1226-34. [PubMed ID: 32686252]. https://doi.org/10.1111/tmi.13468.
-
8.
Calhoun LM, Speizer IS, Guilkey D, Bukusi E. The effect of the removal of user fees for delivery at public health facilities on institutional delivery in urban kenya. Matern Child Health J. 2018;22(3):409-18. [PubMed ID: 29288407]. [PubMed Central ID: PMC5845052]. https://doi.org/10.1007/s10995-017-2408-7.
-
9.
Pot H, de Kok BC, Finyiza G. When things fall apart: Local responses to the reintroduction of user-fees for maternal health services in rural Malawi. Reprod Health Matters. 2018;26(54):126-36. [PubMed ID: 30388957]. https://doi.org/10.1080/09688080.2018.1535688.
-
10.
Ravit M, Audibert M, Ridde V, de Loenzien M, Schantz C, Dumont A. Removing user fees to improve access to caesarean delivery: A quasi-experimental evaluation in western Africa. BMJ Glob Health. 2018;3(1). e000558. [PubMed ID: 29515916]. [PubMed Central ID: PMC5838396]. https://doi.org/10.1136/bmjgh-2017-000558.
-
11.
WHO. World health statistics 2015. World Health Organization; 2015.
-
12.
Khan JAM, Ahmed S, Evans TG. Catastrophic healthcare expenditure and poverty related to out-of-pocket payments for healthcare in Bangladesh-an estimation of financial risk protection of universal health coverage. Health Policy Plan. 2017;32(8):1102-10. [PubMed ID: 28575415]. https://doi.org/10.1093/heapol/czx048.
-
13.
WHO. Out-of-pocket expenditure (% of current health expenditure). 2018. Available from: https://data.worldbank.org/indicator/SH.XPD.OOPC.CH.ZS.
-
14.
Almasiankia A, Kavosi Z, Keshtkaran A, Jafari A, Goodarzi S. Equity in health care financing among Iranian households. Shiraz Med J. 2015;16(11-12). https://doi.org/10.17795/semj28653.
-
15.
Cinaroglu S. Poverty effects of public health reforms in Turkey: A focus on out-of-pocket payments. J Eval Clin Pract. 2021;27(1):53-61. [PubMed ID: 32131143]. https://doi.org/10.1111/jep.13383.
-
16.
Kalke P, Mundhe D, Dubey DK. Determinants and distribution of out of pocket expenditure for health care services in a district of western Maharashtra, India: An observational study. Res Sq. 2021. https://doi.org/10.21203/rs.3.rs-207143/v1.
-
17.
Darvishi A, Amini-Rarani M, Mehrolhassani MH, Yazdi-Feyzabadi V. Fairness in household financial contribution to the healthcare system; the evidence of Iran from 2008 to 2018. BMC Res Notes. 2021;190:14. https://doi.org/10.21203/rs.3.rs-154691/v1.
-
18.
Keshavarz A, Kalhor R, Javadi A, Asefzadeh S. [Estimation of direct out-of-pocket payments for treatment costs in Qazvin in 2009]. Hospital. 2011;16(2):1-22. Persian.
-
19.
Na'emani F, Tofighi S, Yahyavi Dizaj J, Safaei Lari M, Noorizade P. [Assessment of the fairness in financial contribution index in iranian health system from 2007 to 2017]. Iran J Health Insur. 2019;2(1):1-6. Persian.
-
20.
Ebadi Fardazar F, Rezapour A. The way of health. Economics of Health Care. Tehran: Ebadifar; 2011.
-
21.
Kazemian M, Abolhalaj M, Nazari H. [Assessment of equity in public health care financing in 2013]. J Clin Nurs Midwifery. 2017;6(1):64-72. Persian.
-
22.
Mehrara M, Fazaeli AA, Fazaeli AA. [Health finance equity in Iran: An analysis of household survey data (1382-1386)]. J Health Adm. 2010;13(40):51-62. Persian.
-
23.
Mohammadzadeh Y, Dizaj JY, Mosadeghrad AM, Kazemi A, Yusefzadeh H. [The impact of government subsidy programs on equity in health financing]. 2020. Persian. https://doi.org/10.21203/rs.3.rs-87034/v1.
-
24.
Yahyavidizaj JY, Anbari Z, Karyani AK, Mohammadzade Y, Anbari Z, Karyani AK, et al. [Targeted subsidy plan and kakwani index in Iran health system]. J Edu Health Promot. 2019. Persian. https://doi.org/10.4103/jehp.jehp_16_19.
-
25.
Sadeghi M, Rahimi M, Poornoroz N, Jahromi FF. Patient satisfaction with hospital services after the implementation of the health system. Arch Pharm. Pract. 2021;12(1):31-6. https://doi.org/10.51847/tzWsa4CPAf.
-
26.
Raghfar H, Vaez Mahdavi Z, Sangari Mohazab K. [Impact of incomplete implementation of the fourth development plan on health catastrophic- payment mediated of population under poverty line]. Econ Res. 2016;16(2):1-22. Persian.
-
27.
Ghafoori MH, Ebadifard Azar F, Arab M, Mahmoodi M, Yusef Zadeh N, Rezapour A. [Inequality in the distribution of health expenditures in 22 districts of Tehran]. J Community Health Res. 2014;3(2):132-44. Persian.
-
28.
Fazaeli AA, Fazaeli AA, Hamidi Y, Moeini B, Valinejadi A. [Analysis of Iranian household financial participation in the health system: Decomposition of the concentration index approach]. Koomesh. 2018;20(2):358-65. Persian.
-
29.
Nakovics MI, Brenner S, Bongololo G, Chinkhumba J, Kalmus O, Leppert G, et al. Determinants of healthcare seeking and out-of-pocket expenditures in a "free" healthcare system: evidence from rural Malawi. Health Econ Rev. 2020;10(1):14. [PubMed ID: 32462272]. [PubMed Central ID: PMC7254643]. https://doi.org/10.1186/s13561-020-00271-2.
-
30.
Rezapour A, Baghi A, Adham D, Ebadi FardAzar F, bagheri S. Inequality in health expenditure and impoverishment impacts resulting from it in Kerman. health and hyginie. 2016;7(2):146-57.
-
31.
Dalui A, Banerjee S, Roy R. Determinants of out-of-pocket and catastrophic health expenditure in rural population: A community-based study in a block of purba barddhaman, west bengal. Indian J Public Health. 2020;64(3):223-8. [PubMed ID: 32985421]. https://doi.org/10.4103/ijph.IJPH_848_20.
-
32.
Pourasghari H, Jafari M, Bakhtiari M, Keliddar I, Irani A, Afshari M. Analysis of equality in Iranian household healthcare payments during Iran's fourth development program. Electron Physician. 2016;8(7):2645-9. [PubMed ID: 27648192]. [PubMed Central ID: PMC5014504]. https://doi.org/10.19082/2645.
-
33.
Zare H, Trujillo AJ, Driessen J, Ghasemi M, Gallego G. Health inequalities and development plans in Iran; an analysis of the past three decades (1984-2010). Int J Equity Health. 2014;13:42. [PubMed ID: 24885492]. [PubMed Central ID: PMC4046006]. https://doi.org/10.1186/1475-9276-13-42.