1. Background
Takayasu’s arteritis is a rare form of large vessel vasculitis of unknown cause. It is more common in young Asian women and most commonly affects the aortic artery and its branches (1). Takayasu’s arteritis is a chronic, recurrent, and progressive disease, and almost 20% of the patients have a self-limited disease, while most patients have recurrent-progressive or progressive process that requires immunosuppressive therapy. The long-term prognosis depends on the presence of arterial complications and its progressive course (2). Of note, 15-year survival for patients with and without Takayasu’s arteritis complications was 66.3% and 96.4%, respectively. To date, the highest prevalence of this disease has been reported to be 40 per million in Japan (3). A study conducted in Norway on a population of different races reported a higher prevalence of the disease, 78 per million of Asian populations descent and 108 per million in Africans descent. Also, the annual incidence of this disease in European lineages is 1 to 2 per million, 6.4 per million in Asian descent, and 13.1 per million in African descent (4). In Iran, the prevalence of Takayasu’s arteritis was reported to be 6% of vasculitis, which is consistent with the report of the American College of Rheumatology (ACR) (5). The ACR classification criteria (91% sensitivity and 98% specificity) require at least three of the following indicators for Takayasu’s arteritis: (1) Upper and lower extremities, (2) decreased brachial artery pulse, (3) lame one limb, (4) onset at age less than or equal 40, claudication of an extremity, decreased brachial artery pulse, > 10 mmHg difference in systolic blood pressure between arms, bruit over the subclavian arteries or aorta and arteriographic evidence of narrowing or occlusion of entire aorta, its primary branches, or large arteries in the proximal upper and lower extremities (6). Due to the fact that the standard imaging or laboratory method for diagnosis of this disease with sufficient sensitivity and specificity has not been determined, the ACR places more emphasis on physical examination of patients to classify this disease (7). Most Takayasu’s arteritis patients have gradual and subacute clinical manifestations that delay diagnosis and can last for months or years. Non-specific symptoms of arthralgia and myalgia are present in 13 to 41% of patients and may be difficult to distinguish from other rheumatic patients. Transient ocular manifestations and vision loss were reported in 4 to 8% of patients, which is associated with narrowing and obstruction of the carotid or vertebral arteries. The presence of limbs claudication in the limbs, lack of brachial pulse, difference in Limb’s systolic blood pressure and arterial bruit are clinical features of Takayasu’s arteritis patients. Takayasu’s arteritis classification criteria are based on the diagnosis of arterial stenosis or obstruction using angiography, but angiography cannot examine changes in the vessel wall and carries the risk of complications such as allergic reactions, hematoma, embolism, and arterial dissection. Therefore, angiography has been replaced by novel imaging techniques. The role of imaging techniques such as ultrasound, MRI and CT scan, and PET scan has been emphasized in several studies in recent years (7). The basis of treatment of this disease is based on glucocorticoid administration, like other vasculitis disorders; however, the effectiveness of such treatment has not been studied in any study (8). Cohort studies have examined the efficacy of drugs such as methotrexate, azathioprine, leflunomide, mycophenolate mofetil, and cyclophosphamide in controlling disease activity (9). Biological compounds can also be used in patients with glucocorticoid-dependent or drug-resistant Takayasu’s arteritis (8). Disability due to rheumatic diseases has negative impacts on the living and working conditions of patients (10).
2. Objectives
The aim of this study was to provide a descriptive study of patients with Takayasu’s arteritis in Arak, influencing factors in the development of the disease, clinical manifestations, diagnostic methods, and treatment models for reporting on the status of these patients to plan and strategy for early identification, appropriate management and social support in the community. The general plan of this project is a descriptive study of patients with Takayasu’s arteritis in Arak city from 2009 to 2019.
3. Methods
3.1. Design
All patients with Takayasu’s arteritis referred to the rheumatology office, and specialized and sub-specialized clinic of Amir Al-Momenin were studied from 2009 to 2019. After obtaining the code of ethics from the ethics committee in medical sciences research of Arak University of Medical Sciences, the research was conducted as a case series study.
3.2. Ethical Consideration
All procedures performed in studies, involving human participants, were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This research has an ethics code from the Ethics Committee in Medical Sciences Research of Arak University of Medical Sciences. Data recording without mentioning patients’ identities is completely confidential, and informed consent was obtained from all participants in the study. The ethics code of the project is (IR.ARAKMU.REC.1398.294).
3.3. Patient Selection
Patients with Takayasu’s arteritis disease based on 1990 criteria for classification of Takayasu. were considered, and the informed consent form by patients announcing readiness to cooperate in conducting research has been completed. Patients with lack of cooperation in conducting the research and lack of information were excluded from this study.
3.4. Data Collection
Objective details such as determining the demographic characteristics of patients, clinical features, physical examination findings, treatment patterns of patients, imaging methods used for diagnosis, mean time interval between onset of symptoms and medical visit, mean time between the onset of symptoms and diagnosis, the average dose of glucocorticoid prescribed is the interval between the initiation of treatment and the initiation of tumor necrosis factor-alpha inhibitors (anti-TNFα) drugs, the pattern of laboratory disorders associated with acute phase reactants (ESR, CRP, hemoglobin) were evaluated in Takayasu’s arteritis patients. These demographic data can be useful in the early diagnosis of the disease.
3.5. Statistical Analysis
All statistical analyses were performed using SPSS software version23. The mean and standard deviation were used to present continuous variables, while categorical variables were shown as frequency and percentage. Univariate analysis was done using non-parametric tests (chi-square). Estimating odds ratios was also done using logistic regression, the charts and receiver operating characteristic (ROC) curve were used to calculate sensitivity, specificity, negative and positive predictive value using SPSS software version23. P-values < 0.05 were considered significant.
4. Results
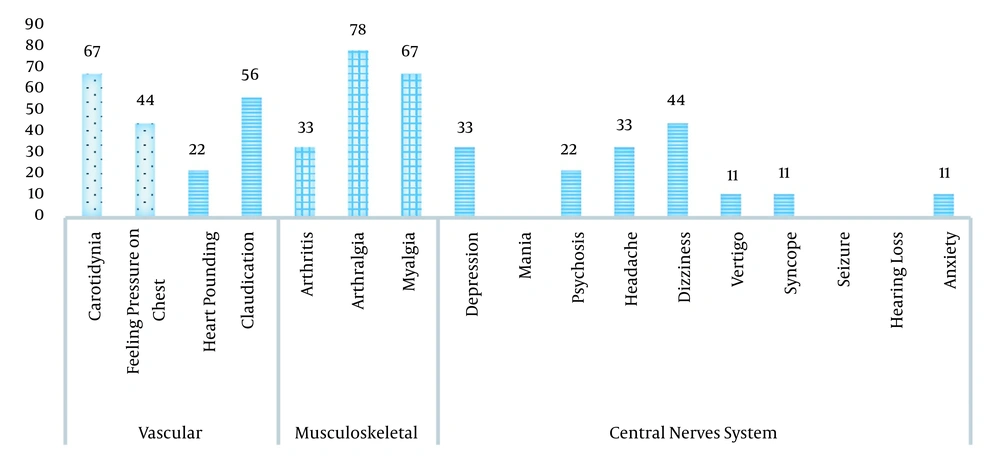
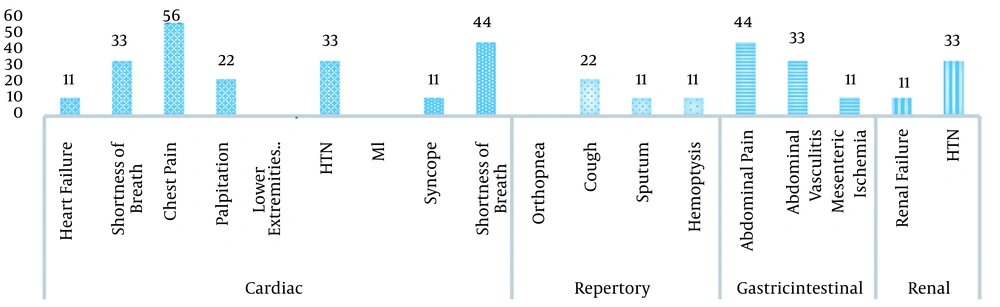
We studied nine patients, including eight women (88.9%) and one man (11.1%). The mean age of these patients was 28.5 years (range: 7 - 46) at the time of diagnosis. In this study, two patients (22.2%) met six criteria of the American College of Rheumatology, and seven patients (77.8%) met more than three criteria. As we know, the clinical manifestation of Takayasu has two phases: The prepulseless phase in which the patient complains of constitutional symptoms such as fever, weight loss, fatigue, arthralgia, and myalgia. The second phase, which appears months or years later, includes end-organ ischemia such as limb claudication, decreased or absent pulses, vascular bruit, and aortic regurgitation. Twenty-four non-specific signs and symptoms in the first phase led to delayed diagnosis and caused organ or life-threatening complications. In this study, the delay between the onset of symptoms and the diagnosis of the disease was between 2 - 108 months. Figure 1 indicates the main clinical manifestations in Takayasu’s arteritis patients. Seven out of nine patients (77.8%) had non-specific symptoms at the time of the onset of the disease; details are presented in Table 1. In terms of vascular symptoms, carotidynia is the most common symptom reported in six patients (66.7%). To clarify these figures, we present some examples, 44% of Takayasu’s arteritis patients suffered from feeling pressure on the chest, and 22% of Takayasu’s patients suffered from heart pounding. Details of the percentage of the clinical symptoms in Takayasu’s arteritis patients are presented in Figures 1 and 2. Table 2 presents the frequency of pulse examination findings index in Takayasu’s arteritis. Lack of pulse was found in seven patients (77.8%), the blood pressure difference in limbs in six patients (66.7%), and vascular bruit in six patients (66.7%). One patient had bruit in six vascular regions, and the most common site of bruit was the right common carotid artery. Table 3 presents the frequency distribution of limb blood pressure index in Takayasu’s arteritis patients. The most common imaging method used at the initiation of the disease was magnetic resonance angiography (66.7%). Complete information about the imaging method is given in Table 4. In Table 5, we present the type of vascular lesion observed in imaging based on number and percentage.
| Feature | No. (%) |
|---|---|
| Fatigue | 5 (55.6) |
| Anorexia | 3 (33.3) |
| Malaise | 4 (44.4) |
| Night sweat | 3 (33.3) |
| Fever | 5 (55.6) |
| Weight loss | 3 (33.4) |
| Absent | Normal | Decrease | |
|---|---|---|---|
| Radial-right | 2 (22.2) | 7 (77.8) | 0 |
| Ulnar-right | 2 (22.2) | 6 (66.7) | 1 (11.1) |
| Brachial-right | 2 (22.2) | 6 (66.7) | 1 (11.1) |
| Carotid-right | 0 | 9 (100) | 0 |
| Femoral-right | 1 (11.1) | 8 (88.9) | 0 |
| Dorsalis-pedis-right | 1 (11.1) | 8 (88.9) | 0 |
| Posterior-tibia-right | 1 (11.1) | 8 (88.9) | 0 |
| Abdominal aorta | 0 | 9 (100) | 0 |
| Radial-left | 3 (33.3) | 5 (55.6) | 1 (11.1) |
| Ulnar-left | 3 (33.3) | 5 (55.6) | 1 (11.1) |
| Brachial-left | 3 (33.3) | 5 (55.6) | 1 (11.1) |
| Carotid-left | 0 | 9 (100) | 0 |
| Femoral-left | 1 (11.1) | 8 (88.9) | 0 |
| Dorsalis-pedis-left | 2 (22.2) | 6 (66.7) | 1 (11.1) |
| Posterior-tibia-left | 2 (22.2) | 7 (77.8) | 0 |
a Values are expressed as No. (%).
| Absent | Decreased | Normal | |
|---|---|---|---|
| Right-arm | 2 (22.2) | 1 (11.1) | 6 (66.7) |
| Left-arm | 4 (44.4) | 1 (11.1) | 4 (44.4) |
| Right-leg | 2 (22.2) | 0 | 7 (77.8) |
| Left-leg | 1 (11.1) | 0 | 8 (88.9) |
a Values are expressed as No. (%).
| No. (%) | |
|---|---|
| CT angio | 5 (55.6) |
| MR angio | 6 (66.7) |
| Conventional angio | 4 (44.4) |
| Doppler US | 6 (66.7) |
| PET scan | 0 |
| Vessel | Normal | WT | Occlsion | Stenosis |
|---|---|---|---|---|
| Hand distal vessels | 7 (77.8) | 0 | 1 (11.1) | 1 (11.1) |
| Radial artery | 6 (66.7) | 0 | 1 (11.1) | 2 (22.2) |
| Ulnar artery | 6 (66.7) | 0 | 1 (11.1) | 2 (22.2) |
| Brachial artery | 6 (66.7) | 0 | 1 (11.1) | 2 (22.2) |
| Subclavian artery | 2 (22.2) | 0 | 5 (55.6) | 2 (22.2) |
| Carotid | 3 (33.3) | 3 (33.3) | 0 | 3 (33.3) |
| Aortic arc | 8 (88.9) | 1 (11.1) | 0 | 0 |
| Descending aorta | 8 (88.9) | 1 (11.1) | 0 | 0 |
| Abdominal aorta | 7 (77.8) | 7 (77.8) | 0 | 1 (11.1) |
| Mesenteric artery | 6 (66.7) | 2 (22.2) | 0 | 1 (11.1) |
| Celiac artery | 7 (77.8) | 0 | 0 | 2 (22.2) |
| Renal artery | 7 (77.8) | 0 | 1 (11.1) | 1 (11.1) |
| Iliac artery | 7 (77.8) | 0 | 0 | 2 (22.2) |
| Femoral artery | 5 (55.6) | 0 | 1 (11.1) | 3 (33.3) |
| Tibial artery | 6 (66.7) | 0 | 1 (11.1) | 2 (22.2) |
| Peroneal artery | 6 (66.7) | 0 | 2 (22.2) | 1 (11.1) |
| Foot distal vessels | 6 (66.7) | 0 | 1 (11.1) | 2 (22.2) |
| Other | 9 (100) | 0 | 0 | 0 |
a Values are expressed as No. (%).
5. Discussion
Takayasu’s arteritis is a rare form of large vessel vasculitis that mainly affects the aorta and its branches (1). Takayasu’s arteritis incidence is reported to be about 1 - 2 per million in Japan (3) and 3.4 per million in Turkey (11). In this study, the demographic characteristics of patients in terms of gender ratio (women to men) was 8 : 1, which is comparable to other studies, including a study of Takayasu’s arteritis in Italy. The mean age of onset of the disease in our patients was 28.89 years (range: 9 - 45 years), which is similar to the study conducted in Italy (12) and a study conducted by Malek Mahdavi et al. in Iran (13). One of the most important points in the diagnosis of Takayasu’s arteritis was the delay between the onset of symptoms and the diagnosis. This delay may lead to irreversible complications and increased morbidity. In the present study, the delay between the onset of symptoms and the diagnosis of was 2 - 108 months (mean: 29.2), which was longer than the study conducted in Italy, which was 15.5 months (12), as well as the study conducted by Kerr et al. (14). Illiteracy was associated with further delays in diagnosis, a finding that emphasizes that Takayasu’s arteritis disease should always be considered in the differential diagnosis of constitutional signs and symptoms, especially in young women. Constitutional signs and symptoms (fatigue, loss of appetite, lethargy, fever, and weight loss), which indicate an inflammatory process, were reported in 77.78% of the patients in our study at the time of diagnosis, which is similar to a study conducted by Vanoli et al. in Italy (12), and more than the Norwegian report (4). These complaints can be before the onset of vascular symptoms or at the same time. In this study, all patients met the criteria of the ACR for Takayasu’s arteritis. Two people (22.22%) had all six criteria, and seven people (77.78%) had more than three criteria. These results are close to the results of the Gudbrandsson et al. study in Norway, in which 85.9% of the patients had the ACR criteria (4), and in a study conducted in Italy, 25% of the patients met all six criteria of the Takayasu classification (27%) (12).
Carotid pain (carotidynia) was the most common vascular symptom in our study, 66.67% of the nine patients and 55.56% had claudication. In a study conducted in Italy (12), vascular claudication was reported in 58% of patients, and it was reported in 59% of patients in a study conducted by Gudbrandsson et al. in Norway (4). In terms of angiographic distribution of the disease, type V was the most common type of vascular involvement found in 55.56%, arterial stenosis was the most common lesion similar to the Takayasu’s study in Italy, only one patient (11.11%) had an arterial aneurysm (12). Similar to the other forms of vasculitis, glucocorticoids are the basis of remission in Takayasu’s arteritis (14). In this study, all patients in our study received glucocorticoids as initial treatment, except for one patient who received prednisolone methyl pulse and one patient who initially had low activity and received 5 mg/day of prednisolone. Other patients received 1 mg/kg/day. All patients in this study received a glucocorticoid sparing agent as part of the treatment. Methotrexate was the most commonly used drug in all patients at the outset. One patient discontinued due to side effects. Five patients (55.56%) did not respond well to methotrexate and three patients were still taking this drug until the preparation of this report. In a study conducted by Mutoh et al. in 2019, the most common drug used as a steroid-sparing agent was methotrexate, which was used in 75% of patients (15). The second steroid-sparing agent used in this study was mycophenolate mofetil that 66.67% of patients received this drug, and four patients did not respond to the drug and stopped taking the drug base on the physician’s recommendation. According to some studies, among all disease-modifying drugs, mycophenolate mofetil seems to be one of the most promising disease control therapies in Takayasu’s Arteritis (16). Among TNFα inhibitors, infliximab was the only drug used in 33.33% of the patients in this study; one patient did not continue treatment with this drug, and one patient relapsed after 25 months. Shuai et al., who conducted a systematic review and meta-analysis, reported the efficacy and safety of biological drugs were examined and published in 2021. The rate of remission in individuals undergoing antibody treatment was reported to be 65%, and the recurrence rate was 28% (17). One of the most important reasons for the low use of biologics drugs in our patients was the high cost of medication and insurance coverage issues, so we cannot provide a correct pattern of use of these drugs and compare it with other studies. One patient used Tocilizumab until the presentation of this report, which had a good clinical response, but discontinued the drug after 12 months due to high cost and lack of insurance coverage.
5.1. Limitations
The small number of patients is one of the limitations of this study, which can be due to the rarity of the disease and the single-center condition of the study.
5.2. Conclusions
The present report described the characteristics of patients with Takayasu’s Arteritis in Arak, Iran. Although the number of patients in this study is small, these results can inform our physicians about the signs, symptoms, and complications of delayed diagnosis of Takayasu’s arteritis disease and paying attention to timely diagnosis, especially in patients with structural symptoms, diagnostic guidelines, and the treatment of this disease.