Abstract
Background:
In medicine, obesity is considered as one of the health-threatening factors in the world, which is referred to as the disease of the century. Many diseases, including pulmonary disease, are directly related to obesity and cause a significant percentage of annual mortality.Objectives:
The purpose of this study was to investigate the effect of selected exercise training on pulmonary function indices of inactive overweight and obese women.Methods:
This quasi-experimental study was performed on 26 obese and overweight women with the age range of 40 - 50 years and a BMI of 30.16 ± 3.26 who met the inclusion criteria in the study. After purposeful selection and measurement of anthropometric indices and pulmonary function, subjects were randomly assigned to two equal groups of control (n = 13) and experimental (n = 13). During the sport exercise protocol, an intervention was performed for eight weeks, three sessions per week, and each session 50 to 60 minutes in the indoor courtyard. On the other hand, no intervention was performed on the control group. The data gathered were then analyzed. To perform the intergroup comparison, correlated t-test was used and to compare the intergroup comparison an independent sample t-test, at the significant level of P < 0.05, was used.Results:
The results showed that owing to the sport exercise there was a significant reduction in the experimental group regarding body weight (P < 0.016), body mass index (P < 0.002), and waist to hip ratio (P < 0.001), while the subjects’ maximum oxygen consumption (Vo2max) significantly increased (P < 0.001). In addition, comparing the two groups of study, the results of the independent sample t-test revealed that TV (P = 0.001), FVC (P = 0.001), FEV1 (P = 0.041), FEV1/FVC (%) (P = 0.001), and FEF 25% - 75% (P = 0.001) in the experimental group showed a significant improvement compared to the control group.Conclusions:
Generally, it can be concluded that eight weeks of sport exercise program with weight loss has an effective role in improving the pulmonary indices in obese and overweight women; therefore, continuous physical activity can improve the performance of the pulmonary system.Keywords
1. Background
Obesity is one of the serious medical issues, as the WHO has identified obesity as a global epidemic and the disease of the century. Obesity is one of the greatest health challenges in the world due to the growing trend of obesity and weight gain (1). This phenomenon leads to an increased risk of diseases such as metabolic syndrome, cardiovascular disease, respiratory disruption, and cancer (2). Obesity is one of the epidemic and growing problems in Iran, and national estimates shows that being overweight and obese in the age group of 15 to 35 years are 22% and 16%, respectively (3). There is a lot of evidence that obesity is associated with respiratory problems, as it has been shown that the prevalence of respiratory problems in obese and overweight people is higher than that of normal people (4). Furthermore, the body mass index is positively related to the severity of respiratory problems (5). In animal studies, the association between obesity and pulmonary disorders has been confirmed (6). The possible mechanism for the correlation between being overweight or obese (BMI > 26 kg/m2) and respiratory indices is that excessive abdominal fat stores or the waist-to-hip ratio (WHR) adds to the amount of pressure on the chest and reduces the respiratory dynamic capacities of FVC and FEF, which means that during deep inhalation maneuvering, the diaphragm muscle efficacy, and pulmonary compliance are limited (7). Such structural modifications in the respiratory system are likely to be associated with declines in forced expiratory flow (FEF 25% - 75%) and forced vital capacity (FVC). Accordingly, one of the most important indices of vital respiratory function is FVC. In addition, one of the strongest ventilation indices is forced expiratory volume in the first second (FEV1), which indicates the volume of air that is vigorously released from the lungs within one second after a complete respiration. FVC and FEV1 are among the strongest pulmonary function indicators that decline due to obesity and sedentary lifestyle (8). Reduction in these indices may indicate an increase in the strength or closure of the respiratory tract (9). In his study, Jones examined the effect of obesity and fat distribution on pulmonary function, and concluded that body mass index, fat distribution, waist circumference, and shoulder to hip ratio had a significant negative correlation with FVC and FEV1 (10). Mahajan et al., in their study of 200 obese and non-obese men, reported that FVC and FEV1 were lower in obese subjects than non-obese subjects (11).
Epidemiologic evidence reveals the effect of obesity on decreasing changes in the depth of breath, the narrowing of the airway, and the prevalence of asthmatic syndrome (12). Based on the current research evidence, obesity is considered to be a health risk factor due to the connection with metabolic and hormonal disruptions such as impaired fat metabolism, cardiovascular diseases, and respiratory diseases. The importance of physical activity in maintaining and promoting health, in particular reduced obesity, increased cardiovascular fitness and enhanced muscle strength has been demonstrated, however, the effects of these activities on respiratory testing are not well understood. Some studies have shown that continuous physical activity can improve lung function (13). Research has shown that sport exercises have beneficial effects on tolerance, capacity, as well as ventilation efficacy and lung function (13). Scientific evidence suggests that sport exercise can be beneficial for strengthening the respiratory system and improving the level of ventilation. Since most of the research on the ventilation system in the medical field has been conducted on the individuals with obstructive diseases, and in the field of sport physiology, the contribution of studies on the effect of physical activity on pulmonary function is more likely to be allocated to athletes and championship training programs, and a small proportion of research associated within the women community. In this regard, since middle-aged women make up a significant percentage of the world’s population, their number is increasing, and their health needs require considerable budgets, all countries have to inevitably take them into consideration in their planning. In the same vein, in this research, it was attempted to investigate the effects of a selected sport exercise period on pulmonary function indices of inactive obese and overweight women.
2. Objectives
This study aimed to investigate the effects of selected exercise training on pulmonary function indices of inactive obese and overweight women.
3. Methods
3.1. Subjects
The research method of the current study is semi experimental and research design is pre-test-post-test with control group. The statistical population of this study comprised all middle-aged women of Yasuj city who were overweight and obese. Three weeks after the public call announcement, 64 overweight and obese women volunteered to participate in the study. Among all volunteers, 26 participants with a range of 35 - 50 years, and the mean BMI of 30.16 ± 3.26 kg/m2 by were selected through purposeful sampling. Criteria for inclusion in the study consisted of no smoking history, lack of cardiovascular and respiratory diseases (asthma, pulmonary tuberculosis), liver disease, renal disease, and lack of any physical and orthopedic lesions that interfere with exercise, lack of musculoskeletal problems, not regularly exercising within the past six months and not using certain medications that disrupt the exercise process. After preparation, the questionnaire for cooperation and personal information, physical activity readiness questionnaire (PAR-Q), and consent form were submitted to the participants. The participants were fully acquainted with the objectives of this study and received oral and written training in relation to the method of work. After signing informed consent, volunteers were randomly divided into two groups of exercise (n = 13) and control (n = 13).
3.2. Measuring Anthropometric Indicators
Before starting the first session, anthropometric indices of height (cm) and weight (kg) were taken using height gauge and digital weight gauge (Seca, Germany). The body mass index (kg/m2) and body fat percentage were measured using the advanced body logic body fat analyzer (Model 603, Korea). Resting heart rate and active heart rate were measured by the Polar pulse meter (Sweden). The participants’ maximum oxygen consumption (Vo2max) was measured using Bruce’s oxygen consumption protocol attached on the treadmill labelling Technogym (made in Italy), with a reliability of 0.96, so that the warm-up and the Bruce protocol were controlled by the device as a comprehensive training protocol; the results were recorded.
3.3. Spirometry Test
To measure respiratory indices, participants were first asked to become familiar with the device, and then, each subject was asked to practice with a spirometry device several times.
The subject was asked to rest while sitting on a chair, with a perfectly flat back and spine posture, thus, after a few normal sucks and blows on the spirometer, the subject did an immediate and deep inhalation to the extent that the lungs were completely filled with air and afterward, did a strong and maximal exhalation. In this kinetic maneuver, a FVC curve was obtained by which the indices of FVC (L), FEV 1% (percent) TV, FEF 25% - 75% (liter per second), FEV1/FVC% were measured. Each subject performed this operation in three steps, the best of which was calculated. Thus, to determine the indices mentioned, after a strong inhalation, an immediate exhalation was performed at maximum intensity. In Table 1, the definitions of pulmonary function indices are presented.
| Index | Definition of Index |
|---|---|
| TV | Tidal volume |
| FVC | Forced vital capacity |
| FEV1 | Forced expiratory volume in the first second |
| FEF 25% - 75%, L/s | Forced expiratory flow between 25 and 75 percent of vital capacity |
| FEV1/FVC% | Forced expiratory volume in the first second to forced vital capacity ratio |
3.4. Exercise Protocol
The exercise protocol consisted of eight weeks of moderate intensity aerobic training with a treadmill, three sessions a week and 60 minutes of training sessions, consisting of 15 minutes of warming, 30 minutes of treadmill walking at an intensity of 55% - 75% of maximum heart rate, and at the end, 15 minutes of strain-breathing exercises. The beginning of the training was at 60% of the maximum heart rate in the first two weeks, and the gradual increase in the intensity of exercise during the subsequent sessions comprised simple stepping (5% increase in the heart rate up to 75% of the heart rate) in terms of slope increase and treadmill speed. Exercise intensity was controlled using a digital pulse meter (Polar model, Sweden). The exercises were conducted under the supervision of an instructor and sports expert in an indoor salon. In order to implement the training program, the required strategies for maintaining the health of the subjects were conducted in accordance with the American College of Sport Medicine (ACSM) (14).
3.5. Statistical Method
In this research, Kolmogorov-Smirnov statistical method was used to determine the normality of the data, and descriptive statistics (mean and standard deviation) were used to describe the data.
Since the pre-test showed no significant difference between the groups in terms of different factors, parametric tests were used. The t-test was used to analyze the hypotheses for intra-group changes and independent t-test was used for intergroup variations. The data obtained in this study were analyzed at the significance level of P < 0.05 using SPSS software (version 21).
4. Results
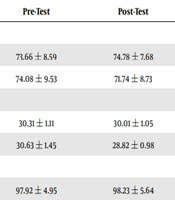
Findings on anthropometric and pulmonary indices of subjects are presented in Table 2. Analysis of data showed that there is a significant difference between body mass index (P < 0.001), waist to hip ratio (P < 0.033), maximum oxygen consumption (P < 0.001), TV (P = 0.001), FVC (P = 0.001), FEV1 (P = 0.041), FEV1/FVC (%) (P = 0.001), and FEF 25% - 75% (P = 0.001) in the two groups at the end of the study.
| Variable | Pre-Test | Post-Test | P Intragroup | P Intergroup |
|---|---|---|---|---|
| Weight, kg | 0.001b | |||
| Control | 73.66 ± 8.59 | 74.78 ± 7.68 | 0.327 | |
| Training | 74.08 ± 9.53 | 71.74 ± 8.73 | 0.016c | |
| BMI, kg/m2 | 0.001b | |||
| Control | 30.31 ± 1.11 | 30.01 ± 1.05 | 0.389 | |
| Training | 30.63 ± 1.45 | 28.82 ± 0.98 | 0.002c | |
| WHR | 0.033b | |||
| Control | 97.92 ± 4.95 | 98.23 ± 5.64 | 0.165 | |
| Training | 98.21 ± 5.32 | 96.37 ± 4.76 | 0.001c | |
| VO2max, mL/kg.min | 0.001b | |||
| Control | 34.54 ± 2.11 | 34.01 ± 1.98 | 0.41 | |
| Training | 35.24 ± 2.34 | 38.64 ± 2.67 | 0.001c | |
| FVC | 0.001b | |||
| Control | 2.45 ± 0.276 | 2.46 ± 0.295 | 0.982 | |
| Training | 2.46 ± 0.34 | 2.67 ± 0.21 | 0.028c | |
| FEV1 | 0.041b | |||
| Control | 2.33 ± 0.43 | 2.37 ± 0.24 | 0.438 | |
| Training | 2.41 ± 0.59 | 2.81 ± 0.67 | 0.001c | |
| FEV1/FVC, % | 0.001b | |||
| Control | 86.12 ± 11.16 | 85.23 ± 11.24 | 0.190 | |
| Training | 85.53 ± 13.43 | 82.82 ± 9.87 | 0.021c | |
| FEF 25% - 75%, L/s | 0.001b | |||
| Control | 2.58 ± 0.74 | 2.61 ± 0.81 | 0.183 | |
| Training | 2.54 ± 0.65 | 2.84 ± 0.79 | 0.012c | |
| TV | 0.001b | |||
| Control | 0.96 ± 0.36 | 0.97 ± 0.43 | 0.190 | |
| Training | 0.97 ± 0.26 | 1.11 ± 0.33 | 0.001c |
The results of the correlated t-test showed that the mean of all variables in the experimental group, after 8 weeks of selected sport exercise, was significantly reduced compared to the pretest. Therefore, sport exercise has been able to improve weight, fat percentage, body mass index, maximum oxygen consumption, and pulmonary function indices in obese and overweight women.
5. Discussion
In this study, the effects of eight weeks of selected sport exercise on anthropometric and pulmonary function indices in obese and overweight women were evaluated. These types of exercise significantly reduced body weight, BMI, WHR, and improved Vo2max in overweight and obese women compared to the pre-test in the experimental group. In addition, there was a significant difference between other anthropometric variables in both experimental and control groups. Similar research findings suggest that visceral fat decreases significantly in the event of weight loss following sport exercise, and can be a major factor in reducing the WHR.
Since WHR is a reliable index of visceral fat expression in humans, a small reduction in body weight can be the reason for this issue. One of the reasons for the reduction of visceral fat, due to the exercise, is increased visceral adipocyte susceptibility to the stimulation of lipolysis, which occurs in response to the released catecholamine’s from exercise. According to the findings of the present study, eight weeks of sport exercise showed a significant increase in the pulmonary function indices. Similar studies have shown that obesity reduces lung volumes and capacities (15). The findings of this study showed that eight weeks of exercise increased FVC significantly in non-obese women; it also significantly increased FEV1 in overweight and obese women. Therefore, the increase in FVC, following the sport exercise in this study, may be attributed to improvements in the development of respiratory muscles and body fat loss in obese women. In the present study, FEV1 in the subjects had a significant increase. It seems that the adipose tissue around the chest, abdomen, and visceral cavity increases chest loads and causes changes in lung volumes, respiratory patterns, and airways. Therefore, weight loss can reverse many changes in the pulmonary function indices induced by obesity (16).
Abdominal fat deposits in obese people reduce the diaphragm workload relative to abdominal adipocyte with weight gain on the chest wall, therefore, obese individuals can’t have a good pulmonary function, as reported by Hong et al. (17).
In different studies, there has been an inverse correlation between pulmonary function and adipose tissue, which suggests that as the adipose tissue of the body increases, pulmonary function can’t be optimal, and hence the normal pulmonary function is impaired. The findings of the study by Koraddi et al., showed that the performance of respiratory parameters measured in obese women and men was significantly lower than non-obese subjects (18).
Sport exercise is the first line of treatment and the observation of special medical care is a convenient and inexpensive device for tracking and treating metabolic diseases (19, 20). Glycemic control, weight control, cardiovascular fitness, and ultimately increased muscle strength are the positive effects of exercise on health promotion (13). Thus, in the treatment of respiratory diseases, in order to maintain the existing pulmonary function and to remove or reduce the respiratory problem, it is necessary to increase the strength and tolerance of the respiratory system (20). As a result, sport activities stimulate the organs to provide oxygen to the body’s cells, this oxygen is supplied through the bloodstream to the active muscles. Therefore, in order to create this type of aerobic metabolism in the cell, sport exercises should be performed at sub-maximal level and long-term period.
Following aerobic exercises, valuable changes and structural adaptations occur in the lungs and blood vessels. In other words, by performing aerobic exercises, more oxygen enters the lungs and more carbon dioxide is released from the lungs, thus, ultimately, oxygen transfer to muscle cells improves (21).
The training program had an effective role in improving the FEV1, FVC, and PEF functional indices. One of the mechanisms of the effect of exercise on improving lung function is the improvement of respiratory muscles (22).
Shaw et al., showed that the combination of aerobic training and special diaphragmatic exercises is more effective in improving FVC and FEV1. They stated that the increase of these two variables could indicate a decrease in airway obstruction, which results from an increase in the effective breathing force due to the strengthening of the elasticity of the main and ancillary intercostal muscle fibers (23).
The findings of this study are consistent with the results of Afshunpour and Mehdizadeh on the effect of sport exercise on pulmonary function indices in obese individuals. Afshunpour et al., reported an increase and improvement in FEV1, %FEV1 following sport exercises in 30 to 50-year-old men with type 2 diabetes (24). The study of Mehdizadeh et al., examined the effect of central resistance exercises for 12 weeks on pulmonary function indices in obese women with type 2 diabetes and showed that these exercises significantly increase the pulmonary indices of FVC and FEV1, which is consistent with the findings of this research.
In the current study, aerobic exercise was performed on the treadmill by inhalation from the nose and exhalation from the mouth. The beneficial effect of breath-taking from the nasal route compared to the breath-taking from the oral route on increasing pulmonary volume has been reported (25). Therefore, in the present study, the increasing role of respiratory training, along with aerobic exercises, may contribute to the improvement of pulmonary function indices (26).
5.1. Conclusions
Based on the results of the research, the exercises provided in the present study can be effective therapeutic interventions for overweight and obese women, since this level of exercise, without manipulating the diet of the subjects, leads to weight loss and obesity indicators that are risk factors for recognized metabolic disease. Since reducing body fat, especially abdominal and breast fat in obese people, can be effective in reducing pulmonary complications, sport exercise programs that can reduce body fat are important therapeutic interventions to improve pulmonary function; hence, overweight and obese individuals are recommended to follow long-term exercises as low-cost, safe, and effective treatments, parallel with other clinical trials, in order to prevent or treat lung complications.
Acknowledgements
References
-
1.
Tabatabayi Molazi O, Larijani B. [A survey on the prevalence of obesity and its administration in Iran]. Iran J Diabetes Lipid. 2013;12(5). Persian.
-
2.
Abdi J, Eftekhar H, Mahmoodi M, Shojayzadeh D, Sadeghi R, Saber M, et al. [The effect of theory and new communication technologies based lifestyle intervention on the weight control of the employees with overweight and obesity]. Iran J Health Educ Health Promot. 2015;3:188-97. Persian.
-
3.
Salehi-Abargouei A, Abdollahzad H, Bameri Z, Esmaillzadeh A. Underweight, overweight and obesity among zaboli adolescents: A comparison between international and iranians' national criteria. Int J Prev Med. 2013;4(5):523-30. [PubMed: 23930162]. [PubMed Central: PMC3733182].
-
4.
Spathopoulos D, Paraskakis E, Trypsianis G, Tsalkidis A, Arvanitidou V, Emporiadou M, et al. The effect of obesity on pulmonary lung function of school aged children in Greece. Pediatr Pulmonol. 2009;44(3):273-80. doi: 10.1002/ppul.20995. [PubMed: 19208374].
-
5.
Varraso R, Siroux V, Maccario J, Pin I, Kauffmann F; Epidemiological Study on the Genetics, et al. Asthma severity is associated with body mass index and early menarche in women. Am J Respir Crit Care Med. 2005;171(4):334-9. doi: 10.1164/rccm.200405-674OC. [PubMed: 15557134].
-
6.
Johnston RA, Theman TA, Shore SA. Augmented responses to ozone in obese carboxypeptidase E-deficient mice. Am J Physiol Regul Integr Comp Physiol. 2006;290(1):R126-33. doi: 10.1152/ajpregu.00306.2005. [PubMed: 16002559].
-
7.
Fairshter RD, Carilli A, Soriano A, Lin J, Pai U. The MVV/FEV1 ratio in normal and asthmatic subjects. Chest. 1989;95(1):76-81. doi: 10.1378/chest.95.1.76. [PubMed: 2642414].
-
8.
Garcia-Aymerich J, Lange P, Benet M, Schnohr P, Anto JM. Regular physical activity modifies smoking-related lung function decline and reduces risk of chronic obstructive pulmonary disease: A population-based cohort study. Am J Respir Crit Care Med. 2007;175(5):458-63. doi: 10.1164/rccm.200607-896OC. [PubMed: 17158282].
-
9.
Simoes RP, Deus AP, Auad MA, Dionisio J, Mazzonetto M, Borghi-Silva A. Maximal respiratory pressure in healthy 20 to 89 year-old sedentary individuals of central Sao Paulo State. Rev Bras Fisioter. 2010;14(1):60-7. [PubMed: 20414563].
-
10.
Jones RL, Nzekwu MM. The effects of body mass index on lung volumes. Chest. 2006;130(3):827-33. doi: 10.1378/chest.130.3.827. [PubMed: 16963682].
-
11.
Mahajan S, Arora A, Gupta P. Obesity and spirometric ventilatory status correlation in adult male population of Amritsar. Natl J Physiol Pharm Pharmacol. 2012;2(2):93. doi: 10.5455/njppp.2012.2.93-98.
-
12.
Tantisira KG, Weiss ST. Complex interactions in complex traits: Obesity and asthma. Thorax. 2001;56 Suppl 2:ii64-73. [PubMed: 11514709]. [PubMed Central: PMC1765987].
-
13.
Pelkonen M, Notkola IL, Lakka T, Tukiainen HO, Kivinen P, Nissinen A. Delaying decline in pulmonary function with physical activity: A 25-year follow-up. Am J Respir Crit Care Med. 2003;168(4):494-9. doi: 10.1164/rccm.200208-954OC. [PubMed: 12791579].
-
14.
Lippincott W. ACSM's guidelines for exercise testing and prescription. 33. 9th ed. Philadelphia: American College of Sports Medicine; 2014. p. 1-5.
-
15.
Mehrabi E, Kargarfard M, Kelishadi R, Mojtahedi H. Effects of obesity on pulmonary function in obese, overweight, and normal students. J Isfahan Med Sch. 2012;30(183):1-9.
-
16.
van Huisstede A, Cabezas MC, Birnie E, van de Geijn GJ, Rudolphus A, Mannaerts G, et al. Systemic inflammation and lung function impairment in morbidly obese subjects with the metabolic syndrome. J Obes. 2013;2013:131349. doi: 10.1155/2013/131349. [PubMed: 23509614]. [PubMed Central: PMC3595660].
-
17.
Hong Y, Ra SW, Shim TS, Lim CM, Koh Y, Lee SD, et al. Poor interpretation of pulmonary function tests in patients with concomitant decreases in FEV1 and FVC. Respirology. 2008;13(4):569-74. doi: 10.1111/j.1440-1843.2008.01274.x. [PubMed: 18410263].
-
18.
Koraddi ST, Bagali S, Aithala M. Effect of body fat distribution on pulmonary functions in young healthy obese students. J Krishna Inst Med Sci. 2015;4(4):18-26.
-
19.
Kadoglou NP, Vrabas IS, Kapelouzou A, Lampropoulos S, Sailer N, Kostakis A, et al. The impact of aerobic exercise training on novel adipokines, apelin and ghrelin, in patients with type 2 diabetes. Med Sci Monit. 2012;18(5):CR290-5. doi: 10.12659/msm.882734. [PubMed: 22534708]. [PubMed Central: PMC3560628].
-
20.
Krist J, Wieder K, Kloting N, Oberbach A, Kralisch S, Wiesner T, et al. Effects of weight loss and exercise on apelin serum concentrations and adipose tissue expression in human obesity. Obes Facts. 2013;6(1):57-69. doi: 10.1159/000348667. [PubMed: 23429279]. [PubMed Central: PMC5644751].
-
21.
Ferdowsi MH, Saiiari A, Valizadeh R, Gholamie A. The effect of eight week aerobic exercise on airway trachea indexes (FEV1, FVC, FEV1.FVC & FEF25-75) and vo2max level in overweighed male students of Ahvaz Payam Noor University. Procedia Soc Behav Sci. 2011;15:2848-52. doi: 10.1016/j.sbspro.2011.04.201.
-
22.
Zolaktaf V, Ghasemi GA, Sadeghi M. Effects of exercise rehab on male asthmatic patients: Aerobic verses rebound training. Int J Prev Med. 2013;4(Suppl 1):S126-32. [PubMed: 23717762]. [PubMed Central: PMC3665018].
-
23.
Shaw I, Shaw BS, Brown GA. Role of diaphragmatic breathing and aerobic exercise in improving pulmonary function and maximal oxygen consumption in asthmatics. Sci Sports. 2010;25(3):139-45. doi: 10.1016/j.scispo.2009.10.003.
-
24.
Ghalavand A, Shakeryan S, Nikbakht M, Mehdipour A, Monazamnezhad A, Delaramnasab M. The effect of resistance training on cardio-metabolic factors in males with type 2 diabetes. Jundishapur J Chronic Dis Care. 2014;2(2):8-17. doi: 10.17795/jjcdc-23346.
-
25.
Allen R. The health benefits of nose breathing. Nurs Gen Pract. 2017:40-2.
-
26.
Multani NK. Comparison of breathing exercises and aerobic exercise in asthmatic children. J Exerc Sci Physiother. 2012;6(2):112.