Abstract
Background:
Attention deficit hyperactivity disorder (ADHD) is often associated with other psychological problems.Objectives:
The present study aimed to study the prevalence of comorbid psychiatric disorders in children and adolescents with ADHD who admitted to Golestan Hospital in Ahvaz.Patients and Methods:
This was a descriptive/analytic cross-sectional study carried out on 118 outpatient children and adolescents who were selected by convenient sampling. The data were collected using the questionnaire, designed by authors, and were analyzed through descriptive statistics and chi-square test.Results:
The prevalence of comorbid disorders were as follows: anxiety disorders (48.3%); depression (20.33%); bipolar disorder (17.79%); obsessive-compulsive (47.45%); tic and tourette (35.59%), oppositional defiant disorder (43.22%); conduct disorder (11.01%); urinary incontinence (58.47%); communication disorder (9.32%); and learning disorder (21.18%). There was no significant difference between females and males with respect to the prevalence of comorbid disorders.Conclusions:
Similar to previous studies, we found some comorbid psychiatric disorders with ADHD. The treatment of the disorder can be improved, by more attention to comorbid psychiatric disorders, early diagnosis of them, and using distinct and specific treatment for everyone.Keywords
Prevalence Comorbidity Attention Deficit/ Hyperactivity Disorder Child Adolescent
1. Background
Attention deficit hyperactivity disorder (ADHD) is one of the most common neurobehavioral and psychiatric disorders in children and adolescents. About 3% - 7% of school age children and adolescents have been reported to be affected by ADHD (1). It is a persistent disorder and often causes impairment in academic performance and interpersonal relationships (2). It is often associated with other psychological problems (3). And research indicates comorbid psychiatric disorders in patients with ADHD (1).
Long-term course and chronic nature of the disorder, various adjustment difficulties attributable to the cumulative effects of ADHD-related impairments, negative environmental circumstances, general propensity for psychiatric disorder, and or genetic factors shared between the two disorders may contribute to concurrence of ADHD and other psychiatric disorders. The comorbid conditions may also reflect harmful effects of ADHD medications (3-5).
Comorbidity with ADHD often causes more treatment-resistant, and patients have lower performance (6). Therefore, treatment of the disorder can be improved, by more attention to comorbid psychiatric disorders.
Some studies pointed to comorbidity of ADHD with obsessive-compulsive disorder (OCD) (7), tourette (7, 8) substance abuse (7, 8), conduct disorder (CD) (7, 9), personality disorder (8, 10), oppositional defiant disorder (ODD) (8, 11), and learning disorder (LD) (8, 11). Mood disorders have been also addressed as comorbid disorders in some research (8, 12).
Some Iranian investigations have been also conducted in this regard. Alaghband-Rad and Shahrivar (3) found that children with ADHD experience more LD compared to children without ADHD. Amiri et al. (13) reported that ODD (29.4%), specific phobia (21.9%), and enuresis (17.5%) were the most common comorbidities in primary school students with ADHD.
Some studies reported gender differences in the prevalence of comorbid psychiatry disorders. For example, in the study conducted by Habrani and Bahdani et al. (14), males more than females were diagnosed with concurrent disorders. But Salehi et al. (15) did not find significant differences between females and males in comorbid disorders in their study; ODD was the most prevalent concurrent disorder in the patients.
2. Objectives
Because of these controversial findings and little knowledge about the prevalence of comorbid psychiatric disorders in patients with ADHD in Ahvaz city, the present study aimed to determine the prevalence of comorbid psychiatric disorders in the patients with ADHD referred to the outpatient clinic of child and adolescent psychiatry of Golestan Educational Hospital in Ahvaz.
3. Patients and Methods
This study is a descriptive epidemiology investigation. The sample of the study consisted of all outpatient children and adolescents diagnosed with ADHD referred to the outpatient clinic of child and adolescent psychiatry of Golestan Educational Hospital in Ahvaz, Iran from March, 20th 2008 to March, 19th 2010. Diagnosis of psychiatric disorders was performed by a clinical psychologist and a psychiatrist following the DSM-IV-TR criteria.
After explaining the procedure and the purpose of the study, informed consent was obtained from the patients’ parents. They were also asked to complete a form to obtain demographic data about their ethnicity, gender, age, date of diagnosis, and so on.
Inclusion criteria included age range of 2 - 17 years. Patients (or their parents) who were not satisfied with participation in the study were excluded. The study was approved by the Ethics Committee of the university (No: IR.AJUMS.REC.1394.30).
Data were analyzed using descriptive statistics and Chi-square test. Odds ratios (OR) with 95% confidence intervals (CI) were also determined. P < 0.05 was considered significant. Statistical analyses were carried out using SPSS v16 software.
4. Results
Frequencies of the participants’ demographic features are listed in Table 1.
| Variable | Values |
|---|---|
| Age, y | |
| 2 - 6 | 68 (57.6) |
| 7 - 12 | 29 (24.6) |
| 13 - 17 | 21 (17.8) |
| Gender | |
| Female | 42 (35.6) |
| Male | 76 (64.4) |
| Ethnicity | |
| Persian (Fars) | 59 (50) |
| Arab | 28 (23) |
| Lur | 31 (27) |
| Others | 0 (0) |
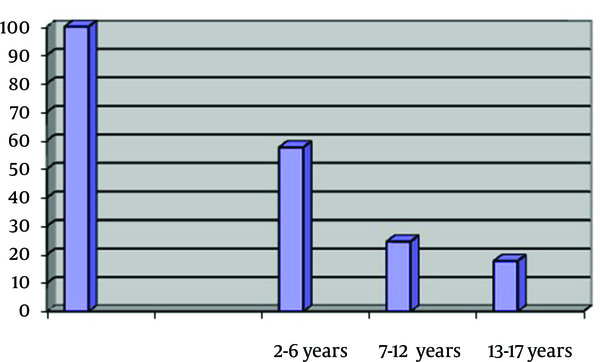
Percentage of Patients, Based on Age
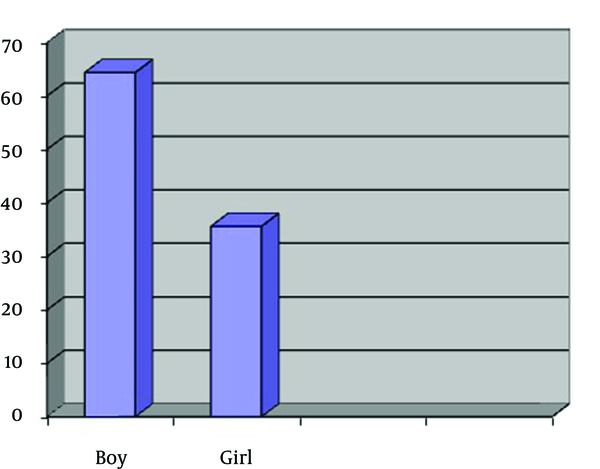
Percentage of Patients, Based on Gender
As shown in Table 2, the prevalences of comorbid disorders were as fallow: anxiety disorders (48.3%); depression (20.33%); bipolar disorder (17.79%); obsessive-compulsive (47.45%); tic and tourette (35.59%), ODD (43.22%); conduct disorder (11.01%), urinary incontinence (58.47%), communication disorder (9.32%), and learning disorder (21.18%). There were no differences in the prevalences of comorbid disorders based on gender (all P > 0.05; Table 2).
| Comorbid Disorder | Frequency c | Frequency Based on Gender | ||||
|---|---|---|---|---|---|---|
| Female | Male | OR | CI | P Value | ||
| Anxiety disorders (phobia, GAD, PTSD, acute stress disorder, separation anxiety) | 57 (48.3) | 22 (18.7) | 35 (29.7) | 1.09 | 0.54 - 2.21 | 0.7 |
| Obsessive compulsive disorder | 56 (47.45) | 33 (27.9) | 23 (19.5) | 1.55 | 0.71 - 3.36 | 0.2 |
| Tic and tourette disorders | 42 (35.59) | 20 (16.9) | 22 (18.6) | 0.92 | 0.39 - 2.14 | 0.8 |
| Depression | 24 (20.33) | 9 (7.6) | 15 (12.8) | 0.59 | 0.19 - 1.75 | 0.3 |
| Bipolar disorder | 21 (17.79) | 10 (8.4) | 11 (9.3) | 0.78 | 0.25 - 2.45 | 0.6 |
| ODD | 51 (43.22) | 25 (21.2) | 26 (22.1) | 0.91 | 4.19 - 2 | 0.8 |
| Conduct disorder | 13 (11.01) | 3 (2.5) | 10 (8.5) | 0.29 | 0.05 - 1.5 | 0.1 |
| Learning disorder | 25 (21.12) | 17 (14.4) | 8 (6.8) | 0.2 | 0.05 - 1.5 | 0.1 |
| Communication disorder | 11 (9.32) | 7 (5.9) | 4 (3.4) | 1.2 | 0.2 - 5.8 | 0.7 |
| Enuresis | 69 (58.47) | 31 (26.3) | 38 (32.2) | 0.74 | 0.36 - 1.52 | 0.41 |
Of 118 patients, 42 (35.6%) were females and 76 (64.4%) were males. Sixty-eight participants (57.6%) were in the age range of 2 - 6 years, 24.6% of individuals were in the age range of 7 - 12 years and 21 patients (17.8%) were in the age range of 13 - 17 years (Table 1, Figures 1 and 2).
5. Discussion
The present study aimed to study the prevalence of comorbid psychiatric disorders in children and adolescents with ADHD. The most prevalent comorbid psychiatric disorders were enuresis, anxiety disorders, OCD, and ODD, respectively.
Our study was carried out in an outpatient child and adolescent psychiatry clinic, so the prevalence of comorbid disorders were higher than some studies in which the sample were drawn from general population (11, 13, 15).
According to our findings, the prevalence of enuresis in patients with ADHD was 58.74%. The prevalence of enuresis in ADHD patients in the study conducted by Amiri et al. (13) was 17.5% and in the study by Khemakhem et al. (16) was 13.72 %.
Our finding showed that anxiety disorders were the second most common disorder in children with ADHD (48.3 %). Different studies have shown high but various prevalences of anxiety disorders in patients with ADHD. In Chutko et al.’s study (7) 27.5 %, in Habrani and Bahdani et al.’s study (14) 44%, in Khemakhem et al.’s study (16) 31.37 %, and in the study of Amiri et al. (13) 42% of patients with ADHD were reported to have anxiety disorders. Therefore, anxiety disorders are common problems in children with ADHD that may affect its treatment.
Results of the current study showed that 47.45% of patients have obsessive compulsive disorder.
Although oppositional defiant disorder was not the first common disorder in patients, it was one of the most prevalent comorbid disorders. Amiri et al. (13), Elia et al. (17), Souza et al. (18), congruent with our result, reported high prevalence of concurrent oppositional defiant disorder, i.e., 29.4%, 40%, and 39%, respectively in patients with ADHD.
All comorbid disorders but OCD and LD were more prevalent in males than females. But the differences were not statistically significant. In contrast to our results, Amiri et al. (13) and Habrani and Bahdani et al.’s study (14) did not find gender related differences in the prevalence of any psychiatric comorbidity.
The discrepancies between our study and previous investigations may be due to the selection of samples from different healthy and clinical populations, and differences in the instruments and diagnostic criteria used to assess ADHD and comorbid psychiatry disorders.
Our research has some limitations. First, the participants were children and adolescents and they were selected from clinical population which means the findings should be generalized to adults with ADHD, and general population with caution. Secondly, we did not compare different subtypes of ADHD in comorbid psychiatric disorders. Therefore study on adults with ADHD and investigation of comorbid disorders in subtypes of ADHD are suggested for the future research.
In spite of these limitations, our findings have some important implications for therapists in the management of their patients. Awareness about comorbidity of psychiatric disorders with ADHD can help them to improve clinical outcomes. The treatment of the disorder can be improved by more attention to comorbid psychiatric disorders, early diagnosis of them, and using distinct and specific treatment for everyone.
In conclusion our research suggests that patients with ADHD experience some comorbid psychiatric disorder. This fact requires treatment and multidimensional interventions.
Acknowledgements
References
-
1.
Riahi F, Tehrani-Doost M, Shahrivar Z, Alaghband-Rad J. Efficacy of reboxetine in adults with attention-deficit/hyperactivity disorder: A randomized, placebo-controlled clinical trial. Human Psychopharmacol: Clin Experiment. 2010;25(7-8):570-6. https://doi.org/10.1002/hup.1158.
-
2.
Ek U, Westerlund J, Holmberg K, Fernell E. Academic performance of adolescents with ADHD and other behavioural and learning problems -a population-based longitudinal study. Acta Paediatr. 2011;100(3):402-6. [PubMed ID: 21054512].
-
3.
Alaghband-Rad J, Shahrivar Z. relationship between attention deficit and learning disorder. Iranian J psych clin psychol. 2000;6:32-6.
-
4.
Kwak YS, Jung YE, Kim MD. Prevalence and correlates of attention-deficit hyperactivity disorder symptoms in Korean college students. Neuropsychiatr Dis Treat. 2015;11:797-802. [PubMed ID: 25848277]. https://doi.org/10.2147/NDT.S80785.
-
5.
Skoglund C, Chen Q, Franck J, Lichtenstein P, Larsson H. Attention-deficit/hyperactivity disorder and risk for substance use disorders in relatives. Biol Psychiatry. 2015;77(10):880-6. [PubMed ID: 25457227]. https://doi.org/10.1016/j.biopsych.2014.10.006.
-
6.
Riahi F, Tashakori A, Izadi-Mazidi S, Salehi-Veysi M. Effectiveness of reboxetine in treatment of outpatient children and adolescents with attention deficit-hyperactivity disorder with comorbid anxiety disorders. Iran J Psychiatry. 2013;8(4):195-200. [PubMed ID: 25628714].
-
7.
Chutko LS, Surushkina S, Bondarchuk Iu L. [Emotional disorders in children with attention deficit hyperactivity disorder]. Zh Nevrol Psikhiatr Im S S Korsakova. 2014;114(9):112-5. [PubMed ID: 25473664].
-
8.
Biederman J, Newcorn J, Sprich S. Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. Am J Psychiatry. 1991;148(5):564-77. [PubMed ID: 2018156]. https://doi.org/10.1176/ajp.148.5.564.
-
9.
Modestin J, Matutat B, Wurmle O. Antecedents of opioid dependence and personality disorder: attention-deficit/hyperactivity disorder and conduct disorder. Eur Arch Psychiatry Clin Neurosci. 2001;251(1):42-7. [PubMed ID: 11315518].
-
10.
Williams ED, Reimherr FW, Marchant BK, Strong RE, Halls C, Soni P, et al. Personality disorder in ADHD Part 1: Assessment of personality disorder in adult ADHD using data from a clinical trial of OROS methylphenidate. Ann Clin Psychiatry. 2010;22(2):84-93. [PubMed ID: 20445835].
-
11.
Zorlu A, Unlu G, Cakaloz B, Zencir M, Buber A, Isildar Y. The Prevalence and Comorbidity Rates of ADHD Among School-Age Children in Turkey. J Atten Disord. 2015. [PubMed ID: 25846229]. https://doi.org/10.1177/1087054715577991.
-
12.
Meinzer MC, Pettit JW, Viswesvaran C. The co-occurrence of attention-deficit/hyperactivity disorder and unipolar depression in children and adolescents: A meta-analytic review. Clin Psychol Rev. 2014;34(8):595-607. [PubMed ID: 25455624]. https://doi.org/10.1016/j.cpr.2014.10.002.
-
13.
Amiri S, Shafiee-Kandjani AR, Fakhari A, Abdi S, Golmirzaei J, Akbari Rafi Z, et al. Psychiatric comorbidities in ADHD children: an Iranian study among primary school students. Arch Iran Med. 2013;16(9):513-7. [PubMed ID: 23981153].
-
14.
Habrani P, Bahdani F. Gender differences in comorbid disorders with attention-deficit/hyperactivity disorder (ADHD). Ofogh-e-Danesh J. 2006;11(4):55-61.
-
15.
Salehi B, Ebrahimi S, Moradi SH. Comparing psychiatric co morbidity in female and male primary school children with attention deficit hyperactivity disorder, Arak, Iran. Bimon J Hormozgan Univ Med Scie. 2012;16(1):49-59.
-
16.
Khemakhem K, Ayedi H, Moalla Y, Yaich S, Hadjkacem I, Walha A, et al. [Psychiatric comorbidity related to children with attention deficit hyperactivity disorder at schools in Sfax, Tunisia]. Encephale. 2015;41(1):56-61. [PubMed ID: 25439858]. https://doi.org/10.1016/j.encep.2012.08.009.
-
17.
Elia J, Ambrosini P, Berrettini W. ADHD characteristics: I. Concurrent co-morbidity patterns in children & adolescents. Child Adolesc Psychiatry Ment Health. 2008;2(1):15. [PubMed ID: 18598351]. https://doi.org/10.1186/1753-2000-2-15.
-
18.
Souza I, Pinheiro MA, Denardin D, Mattos P, Rohde LA. Attention-deficit/hyperactivity disorder and comorbidity in Brazil: comparisons between two referred samples. Eur Child Adolesc Psychiatry. 2004;13(4):243-8. [PubMed ID: 15365895]. https://doi.org/10.1007/s00787-004-0402-2.