Abstract
Background:
Internationally previous publications confirmed that skin cancer could be categorized as one of the most common cancer among others.Objectives:
This study aimed to investigate skin cancer crude rate and incidence in Isfahan Province, Iran.Methods:
Data (2011 - 2015) was collected from the Isfahan Cancer Registry. The skin cancer was defined by topography code C43 and C44. Period prevalence and incidence was calculated per 100 000 persons.Results:
There were 3837 patients that corresponded to a period prevalence of 77.1. With a minimum of 5 and a maximum of 103, skin cancer in 67% was defined at the age between 60 and 70 years. Malignant melanoma of skin was reported in 8 out of total population in which all died from it at the age between 42 to 95 years. There was an increase in incidence from 17.4 to 22.3, in which the mean incidence in males (24) was significantly higher (P < 0.001) than females (14.3).Conclusions:
In total population there was death- reported-data in 2% of patients with skin cancer. A 28.2% increase in incidence and 69.1% higher crude rate of males (96.2) versus females (56.9), which recommends further research in this direction.Keywords
1. Background
By chronic sun exposure, the complex process leads to DNA damage and reactive oxygen species production associated to skin tumorigenesis. Basal cell, squamous cell, and melanoma are mentioned as three types of skin cancers. Exposure to ultraviolet radiation from the sunlight that causes mutations derived basal cell carcinomas, revealed in greater than 90% of cases. Eisemann et al. (1), reported that the age- and sex-standardized melanoma mortality ratio for 5.5 years of follow-up was 0.59. Due to an increase in incidence of melanoma there is constant requirement for dermatologic screening for those after non-melanoma produced in the skin by ultraviolet radiation from the sunlight protects against its oncogenic effects (2-4). Skin cancer diagnosis assumed augmented melanoma possibility (5). Related to head and neck cancer, proton therapy has been used for decades in the treatment of skull-base tumors (6). Antioxidants molecules could also reduce the effect of oxidative stress in such events. Selenoproteins, endogenous antioxidants, could reduce this effect by a defending role (7). The investigation based on a retrospective chart review on 656 patients highlighted an increased incidence of non-melanoma skin cancer in 1.4%, particularly in the 50 - 64 age range (2.8%) when compared with the general United States population (0.65% - 1.05%) (8). Non-melanoma Lozano et al. reported that skin cancers result in 80 000 deaths a year as of 2010, 49 000 of which are due to melanoma, and 31 000 of which are due to non-melanoma skin cancers (9). In the United States a report included 59 695 cases with melanoma in the year 2008 in which 8 623 people died from it (10). Australia has the highest per capita incidence of melanoma in the world, in which more than 12 500 new cases of melanoma are reported each year, out of which more than 1 500 die from the disease (11). Related to basal or squamous cell skin cancers, there is a report regarding the death of about 2 000 people each year in the United States (12). In regards to the Iranian population, a publication reported that the incidence of skin cancer was increasing and the trend was observed in all provinces (13). Razi et al. (14), detailed that the incidence of skin cancer is increasing in Iran, and more in men than women. There was a declining trend for basal cell carcinoma. Basal squamous cell carcinoma and melanoma had an increasing trend. The increase of skin cancer was related to squamous cell carcinoma (14). Skin cancer is also the maximum common category of second malignancy among childhood cancer survivors (15).
2. Objectives
Considering the economic burden for Iranian health services, it is necessary to explore the crude rate for skin cancers. Therefore, this study aimed to investigate the prevalence and incidence for such cancers in a general population of central Iran, Isfahan Province.
3. Methods
Cancer data from March 2011 to March 2015 were obtained from the Isfahan Cancer Registry, located at the Isfahan Deputy of Health. The study was conducted to the Isfahan Kidney Transplantation Research Center (IKTRC) and approved by the Isfahan Deputy of Research Committee via the ethics committee code number of 295115. The cancer sites studied were defined according to the international classification of diseases (ICD-O; 3rd edition). All skin cancers were defined by topography code C43 and C44. Data, with linkage to using of the de-identified patient name and surname, demographic such as age, gender, and date of reported cancer were recorded. The total population for Isfahan city was obtained from the Isfahan/Program and Budget Management Organization. Cancer period prevalence (CPP) was calculated as the proportion of total cases over the period of the years 2011 - 2015 to population at risk during the same time period × 100 000.
Cancer incidence rate (CIR) was calculated as dividing new cases of cancer during a given time period to population at risk during the same time period × 100 000.
The statistical analyses of d-Base was performed using Microsoft Excel and SPSS v. 20 (Chicago, IL, USA) for windows (16-18).
4. Results
Table 1 shows epidemiological data related to period prevalence and incidences in 3837 cases with skin cancer in the Isfahan province.
Demographic and Epidemiological Characteristics in Patients with Skin Cancer
| Total | Females | Males | |
|---|---|---|---|
| Period prevalence | 77.1 | 56.9 | 96.2 |
| Incidence 2011 - 2012 | 17.5 | 13.3 | 21.5 |
| Incidence 2012 - 2013 | 19.6 | 14.5 | 24.5 |
| Incidence 2013 - 2014 | 17.4 | 12.5 | 22.2 |
| Incidence 2014 - 2015 | 22.3 | 16.7 | 27.8 |
With a minimum of five and a maximum of 103, the mean age ± SD was 65 ± 13.9 years old. Figure 1 shows distribution of age in the population studied. Age related to skin cancer in 31% defined at the age between 5 to 60 and in the 67% ranged from 60 to 70 years old of life, respectively. Approximately 2% of skin cancer was diagnosed in patients between the age of under 90 and older.
Distribution of age in total population studied.

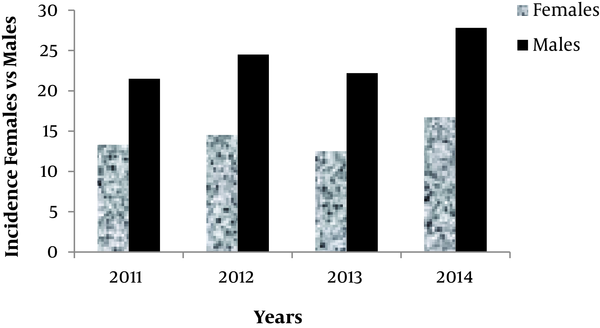
Incidence of skin cancer associated to each gender.
The study population was comprised of 1403 females and 2434 males. This corresponded to a total period prevalence of 77.1 per 100 000 persons in both genders. The period prevalence was significantly different (P < 0.001) between males (96.3) and females (57.2), per 100 000 persons.
Out of the total reported cases, 2% were related to the deceased population. With the minimum of 32 and the maximum of 92, the mean age ± SD was 71 ± 17 years old.
Malignant melanoma of skin was reported in 8 patients comprised of 5 females and 3 males, in which all died from it. That is corresponded to a period prevalence of 0.2 per 100 000 persons in both genders. Age at this population ranged from 42 to 95 years. Figure 2 shows the incidence rates (comprised females versus males) for skin cancer between the years 2011 to 2015, were as follow: 17.4 (13.3 versus 21.5) versus 19.6 (14.5 versus 25.5), versus 17.4 (12.4 versus 22.2), versus 22.3 (16.7 versus 27.7), per 100000 persons correspondingly.
5. Discussion
Skin cancer is one of the most common cancers in the world, particularly in the whites population. Previous publication reported an increase in skin cancer in the incidence of the disease (19). The occurrence rate of skin cancer, within the U.S. population is about 300 - 400 new cases for every 100 000 population per annum (20). Keyghobadi et al., mentioned that in Iran, about 15% of all cancer was skin cancer and this disease reflects as the most common cancer (13, 21). The trend of skin cancer incidence in men was increasing; on an average, it grew by 7.06% yearly. In women, this rate also raised from 12.01 in 2004 to 15.77 in 2008 per 100 000 persons (13, 14).
In agreement with previous publications, there was a 28.2% increase in incidence of skin cancer in both genders from 2011 (Ir: 17.5) to 2015 (Ir: 22.3) per 100 000 persons in Iran/Isfahan. According to previous publications, the incidence of skin cancer in men and women is dissimilar. Non-melanoma cancers in men were about 1.5 times higher than in women (20). This study also showed a similar non-melanoma skin cancer ratio with men, in which a 1.7 times value than women. The significant differences in crude rate between males (96.2) and women (56.9) were also in agreement with publication, which confirmed the highest incidence rate of skin cancer in males in Semnan, Isfahan, and Hamadan provinces (13, 17, 18, 20). Out of the total population studied, the mean age of patients with skin cancer was 65 year that in 67% age ranged from 60 to 70 years. This is in agreement with the publication that confirmed the occurrence of skin cancer mainly in the sixth, seventh, and later decades of life. Previous publications confirmed that skin cancers occur mainly in sun-exposed regions and in the face and neck areas of the body (1-26). In agreement with previous publications in most skin cancers, the sites were reported in the lip, scalp, and neck, which exhibit the major consequence of sunlight on the progress of skin cancers.
In this study, from 2011 to 2015, there was malignant melanoma of skin in eight out of 3 837 patients with skin cancer. This is in agreement with the study conducted in Isfahan in 1998 that found that basel cell carcinoma could be accounted for about 74% of skin cancers (23). Skin could be exposed to ecological issues such as pollutants, chemicals, and ultra violet exposure, which can induce untimely skin aging and increase the risk of skin cancer (7). Thus, further study toward these directions, seem to be advantageous in Iranian population with skin cancer.
5.1. Conclusions
The incidence of skin cancer was increased from 17.4 to 22.3 between 2011 and 2015. There was a higher incidence of skin cancer in males when compared to females (24 versus 14.3) per 100 000 persons associated to each gender. In the population there were death reported data in 2% of patients with skin cancer.
Acknowledgements
References
-
1.
Eisemann N, Waldmann A, Holleczek B, Katalinic A. Observed and expected mortality in the German skin cancer screening pilot project SCREEN. J Med Screen. 2018;25(3):166-8. [PubMed ID: 29169295]. https://doi.org/10.1177/0969141317734003.
-
2.
Cakir BO, Adamson P, Cingi C. Epidemiology and economic burden of nonmelanoma skin cancer. Facial Plast Surg Clin North Am. 2012;20(4):419-22. [PubMed ID: 23084294]. https://doi.org/10.1016/j.fsc.2012.07.004.
-
3.
Gallagher RP, Lee TK, Bajdik CD, Borugian M. Ultraviolet radiation. Chronic Dis Can. 2010;29 Suppl 1:51-68. [PubMed ID: 21199599].
-
4.
Bijlsma MF, Roelink H. Skin-derived vitamin D3 protects against basal cell carcinoma. J Invest Dermatol. 2017;137(12):2469-71. [PubMed ID: 29169462]. https://doi.org/10.1016/j.jid.2017.07.816.
-
5.
Chen ST, Li X, Han J. Personal history of non-melanoma skin cancer diagnosis and death from melanoma in women. Int J Cancer. 2018;142(8):1536-41. [PubMed ID: 29171018]. https://doi.org/10.1002/ijc.31176.
-
6.
Blanchard P, Gunn GB, Lin A, Foote RL, Lee NY, Frank SJ. Proton therapy for head and neck cancers. Semin Radiat Oncol. 2018;28(1):53-63. [PubMed ID: 29173756]. https://doi.org/10.1016/j.semradonc.2017.08.004.
-
7.
Jobeili L, Rousselle P, Beal D, Blouin E, Roussel AM, Damour O, et al. Selenium preserves keratinocyte stemness and delays senescence by maintaining epidermal adhesion. Aging (Albany NY). 2017;9(11):2302-15. [PubMed ID: 29176034]. [PubMed Central ID: PMC5723688]. https://doi.org/10.18632/aging.101322.
-
8.
Sturgeon A, Pate DA, Patel R, Snodgrass K, Tarbox M, Prabhu F, et al. Incidence of non-melanoma skin cancer in the Uninsured. J Health Care Poor Underserved. 2017;28(4):1327-32. [PubMed ID: 29176098]. https://doi.org/10.1353/hpu.2017.0117.
-
9.
G. B. D. Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1345-422. [PubMed ID: 28919119]. [PubMed Central ID: PMC5614451]. https://doi.org/10.1016/S0140-6736(17)32366-8.
-
10.
Baldwin J, Janitz AE, Erb-Alvarez J, Snider C, Campbell JE. Prevalence and mortality of melanoma in Oklahoma among racial groups, 2000 - 2008. J Okla State Med Assoc. 2016;109(7-8):311-6. [PubMed ID: 27885301]. [PubMed Central ID: PMC5119754].
-
11.
Reichrath J. The challenge resulting from positive and negative effects of sunlight: how much solar UV exposure is appropriate to balance between risks of vitamin D deficiency and skin cancer? Prog Biophys Mol Biol. 2006;92(1):9-16. [PubMed ID: 16603232]. https://doi.org/10.1016/j.pbiomolbio.2006.02.010.
-
12.
Wang DM, Morgan FC, Besaw RJ, Schmults CD. An ecological study of skin biopsies and skin cancer treatment procedures in the United States Medicare population, 2000 to 2015. J Am Acad Dermatol. 2018;78(1):47-53. [PubMed ID: 28947293]. https://doi.org/10.1016/j.jaad.2017.09.031.
-
13.
Razi S, Enayatrad M, Mohammadian-Hafshejani A, Salehiniya H, Fathali-Loy-Dizaji M, Soltani S. The epidemiology of skin cancer and its trend in Iran. Int J Prev Med. 2015;6:64. [PubMed ID: 26288708]. [PubMed Central ID: PMC4521305]. https://doi.org/10.4103/2008-7802.161074.
-
14.
Razi S, Rafiemanesh H, Ghoncheh M, Khani Y, Salehiniya H. Changing trends of types of skin cancer in Iran. Asian Pac J Cancer Prev. 2015;16(12):4955-8. [PubMed ID: 26163621].
-
15.
Apalla Z, Sotiriou E, Lallas A, Lazaridou E, Vakirlis E, Ioannides D. Basal cell carcinoma in a childhood cancer survivor: What neurosurgeons should avoid. Skin Appendage Disord. 2017;3(4):202-4. [PubMed ID: 29177149]. [PubMed Central ID: PMC5697514]. https://doi.org/10.1159/000476070.
-
16.
Tolou Ghamari Z. Prevalence of lung cancer in Isfahan province, Iran. J Egypt Natl Canc Inst. 2018;30(2):57-9. [PubMed ID: 29691096]. https://doi.org/10.1016/j.jnci.2018.03.001.
-
17.
Tolou-Ghamari Z, Palizban AA, Michael Tredger J. Clinical monitoring of tacrolimus after liver transplantation using pentamer formation assay and microparticle enzyme immunoassay. Drugs R D. 2004;5(1):17-22. [PubMed ID: 14725486].
-
18.
Horsham C, Auster J, Sendall MC, Stoneham M, Youl P, Crane P, et al. Interventions to decrease skin cancer risk in outdoor workers: update to a 2007 systematic review. BMC Res Notes. 2014;7:10. [PubMed ID: 24397996]. [PubMed Central ID: PMC4028889]. https://doi.org/10.1186/1756-0500-7-10.
-
19.
Thieu K, Ruiz ME, Owens DM. Cells of origin and tumor-initiating cells for nonmelanoma skin cancers. Cancer Lett. 2013;338(1):82-8. [PubMed ID: 22579650]. [PubMed Central ID: PMC3422447]. https://doi.org/10.1016/j.canlet.2012.05.008.
-
20.
Keyghobadi N, Rafiemanesh H, Mohammadian-Hafshejani A, Enayatrad M, Salehiniya H. Epidemiology and trend of cancers in the province of Kerman: southeast of Iran. Asian Pac J Cancer Prev. 2015;16(4):1409-13. [PubMed ID: 25743807].
-
21.
Noorbala MT, Kafaie P. Analysis of 15 years of skin cancer in central Iran (Yazd). Dermatol Online J. 2007;13(4):1. [PubMed ID: 18318998].
-
22.
Carucci JA, Leffell DJ. Intralesional interferon alfa for treatment of recurrent lentigo maligna of the eyelid in a patient with primary acquired melanosis. Arch Dermatol. 2000;136(11):1415-6. [PubMed ID: 11074712].
-
23.
Asilian AE. [Skin cancer evaluation in center of Iran]. Pajoohesh Med Sci J. 1998;2:65-7. Persian.
-
24.
Tolou-Ghamari Z, Najafi MR, Mehavari Habibabadi J, Zare M. Preliminarily Analysis of Carbamazepine (CBZ) C0 in Patients Visited Isfahan Epileptic Clinics. Int J Prev Med. 2013;4(Suppl 2):S343-S346. [PubMed ID: 23776749]. [PubMed Central ID: PMC3678243].
-
25.
Shaygannejad V, Rezaei Dehnavi S, Ashtari F, Karimi S, Dehghani L, Meamar R, et al. Study of Type A and B Behavior Patterns in Patients with Multiple Sclerosis in an Iranian Population. Int J Prev Med. 2013;4(Suppl2):S279-S283. [PubMed ID: 23776738]. [PubMed Central ID: PMC3678232].
-
26.
Tolou-Ghamari Z, Palizban AA. Laboratory Monitoring of Cyclosporine Pre-dose Concentration (C0) After Kidney Transplantation in Isfahan. Iran J Med Sci. 2015;28(2):81-85.
