Abstract
Background:
During the outbreak of COVID-19 in developing countries such as Iran, the management of healthcare waste has become a very important issue. It is necessary to investigate the risk of virus transmission through direct contact, inhalation, and environmental pollution to reduce transmission risk. The Hazard Analysis of Critical Control Points framework is used to simplify quick responses of waste management for facing the novel infectious disease.Objectives:
The aim of this study was to use risk analysis frameworks to describe hazard critical control points (HACCP) and make recommendations and corrective actions for staff who work in healthcare facilities and communities experiencing the COVID-19 outbreak.Methods:
In the present descriptive-analytical study, a team of environmental health experts identified the critical control points of healthcare waste produced in Razi Hospital and divided them into three categories and six steps. A tested and verified hazard analysis flow diagram was prepared to determine critical points in different steps of healthcare waste management. Critical control points were identified and analyzed by the team at each step. Recommendations and corrective actions were made for each control point.Results:
The production rate significantly increased from 580 to 1,733 kg per day, probably caused by the increased use of disposable waste during the pandemic. Transportation, disinfection, and storage appeared to be associated with an individually high level of transmission risk of COVID-19 virus. Also, direct contact with infectious waste was often associated with a high risk of virus transmission. In the final disposal of healthcare waste, people were exposed to a lower level of risk.Conclusions:
Training staff in different wards of the hospital to use proper personal protective equipment (PPE), hand washing, disinfectants, and ventilation could reduce the risk of COVID-19 transmission through healthcare waste. Using the HACCP method for providing recommendations and corrective actions could simplify responses to reduce the transmission risk of COVID-19 during pandemics.Keywords
1. Background
Infectious diseases have become a great threat to human societies (1). On January 11, 2020, the World Health Organization (WHO) announced the sixth public health emergency in the world, which caused acute respiratory syndrome called COVID-19 (2, 3). In a short time, it spread to different countries all over the world, such as Thailand, Japan, Taiwan, and Iran (4-6). In February 19, 2020, the first case in Iran was officially announced, but it can be said that it was probably later than the real one (7). By March 2021, approximately 124,313,054 cases were confirmed in 221 countries, with more than 2,735,707 deaths (8). Given the importance of the issue, the pandemic caused unexpected challenges for local governments concerning how to deal with it (9). One of these progressive challenges, especially in populated cities, was how to safely dispose of healthcare waste (10). At the time of the outbreak of COVID-19 in Isfahan city, Iran, more than 1.49 and 2.98 million pieces of masks and gloves were disposed of as waste per day (11). Various types of medical and hazardous waste such as contaminated masks, gloves, and other protective equipment are producing every day, and proper waste management could cause a positive effect on health and the environment (12).
For the first time, the risk analysis method and critical control points were used to control healthcare waste and showed that this method provides a comprehensive and complete response in the shortest time to reduce the problems of landfilling, with the lowest cost (13). Also, the results showed that using HACCP risk analysis of four steps of chemical disinfection, personal protection, internal and external environment management, and life and medical waste management during the H1N1 influenza virus epidemic could lead to a rapid response and help reduce healthcare waste problems (14). Another study have shown that if the HACCP method per-formed continuously from the critical control point could done a proper management in shortest possible time (15). Implementing the HACCP method reduces the environmental load by modifying the waste segregation method (13). Due to the increasing use of disposable materials in these countries, the production rate of hazardous, infectious, and toxic waste has shown tremendous growth (16, 17). On the other hand, most test equipment such as nasopharyngeal test kits, personal protective equipment, and disinfectants are disposable and eventually change to waste (18). Disposal of COVID-19 contaminated waste is challenging. A study in India found that incineration of contaminated waste is the best option for disposal - if it does not lead to environmental pollution (19). Healthcare wastes generated in a hospital in Sari- Iran, was 184,125 kg per day before the outbreak of COVID-19 (20). In Tehran-Iran, some healthcare waste is collected and treated, but in most cases, landfilled. According to the order of the relevant authorities Burning and preparing compost is prohibited (21). According to protocols collection of municipal solid waste and hospitals altogether considered as hazardous waste (22). About 75 & 25% of the wastes that have been generated in hospitals considered as public and hazardous waste, respectively (23, 24). Healthcare wastes in five hospitals- Iran increases 9%, compared to before the pandemic (25). One of the most important environmental issues for healthcare waste is to provide an efficient and reliable management system (26), which categorized into six steps such as identification, collection, separation, storage room, transportation, and disposal (27, 28). Plastic bags or containers with high-resistance is the best way to classifying healthcare waste (29). Steam incineration and sterilization (900 and 1200°) has been recommended by WHO for healthcare waste (30). Important production sources of healthcare waste in hospitals are diagnostics, laboratories, and research wards (31), Hazardous wastes included sharp, contaminated, genotoxic, heavy metals, chemicals and drugs, amputated organs, chemical-pharmaceutical, radioactive and household, and other infectious wastes (32-35), which In developing countries, the production of infectious waste has become a problem (36, 37). Hazardous pathogens in healthcare waste causes many problems for health and environment (38). The WHO stated in 2020 that the route of COVID-19 transmission to the human respiratory system is through respiratory drop-lets and aerosols in the air (39). Health care workers such as doctors, nurses, laboratory technicians, waste collection staff, and people exposed to droplets are prone to COVID-19 Infection (40). Given that few studies conducted on the HACCP process and healthcare waste, it often used to analyze the risks of food safety (41). Over the past two decades, with the introduction of appropriate health measures the HACCP system has been used more than ever (42). In the present study, we used the critical control points risk analysis method to describe critical points in health care waste management and to generate recommendations and corrective actions to give simplify responses for reducing the transmission risk of COVID-19 during pandemics at Razi Hospital in Ghaemshahr.
2. Objectives
With the spread of emerging infectious diseases and other threats to public health, healthcare systems and local governments face unexpected challenges. Existing health systems do not have a good solution to the emerging disease. Few studies have been conducted on healthcare waste management during the pandemic of COVID-19 in 2020. To begin the analysis, we divided the waste management steps into six basic steps: Production, collection, transportation, storage room, decontamination, and final disposal. In this regard, we analized the risk levels of transmission routes such as direct contact, inhalation, and environmental pollution. The purpose of this study was to describe critical points in healthcare waste management of the studied hospital with the HACCP method.
3. Methods
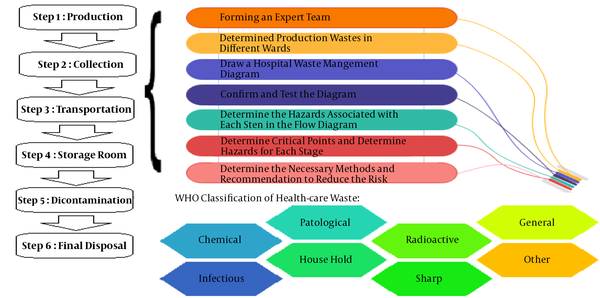
To analyze the risk at critical points, we first reviewed past studies, and then reviewed the guidance in studying HACCP development history and used examples of practical applications (43, 44). Based on the WHO guidelines, we referred to the 12 steps of the HACCP method. In the present descriptive-analytical study, we used the six-step HACCP method to describe critical control points for healthcare waste management, similar to the study of recommendations for dealing with Ebola-contaminated waste (10). The six steps of the research were as follows: (1) gathering a team of environmental health experts with proper experience to analyze the risk of critical control points; (2) identifying healthcare waste in different wards of the hospital with acceptance of COVID-19 disease; (3) constructing a flow-diagram to determine critical points in different steps of healthcare waste management (Figure 1); (4) authenticating and testing the accuracy of the flow-diagram; (5) making a list of the types of healthcare waste and risk levels at critical points for staff (high, medium, and low-risk) associated with each step and running the analysis; (6) specifying critical control points for each step; and (7) making recommendations and corrective actions for each critical point.
Hazard analysis diagram and determination of critical points in different steps of healthcare waste management.
3.1. Team
Our information was gathered via sending emails from environmental health experts to the research team. The analysis started when the members from the Universities of two provinces (Golestan and Mazandaran) feedbacked.
3.2. Process
In the present study, a systematic approach used to combine the opinions of experts and previous studies and the guidelines of WHO. After flow-diagram validation was fully examined, healthcare wastes were divided into three categories: Infectious, chemical-pharmaceutical, and sharp waste. In the initial steps of the study, we identified the most important healthcare wastes in terms of the type of waste and the risk levels in critical control points for employees (high, medium, and low risk). The risk of hazardous waste was calculated by previous studies, and the authors emailed the flow-diagram to a group of environmental health experts. They sent their recommendations and corrective actions to resolve problems in the shortest time. Also, for making the best recommendations and corrective actions, two health professionalists who worked in the Health Ministry of Iran (a faculty and an environmental health expert) gathered WHO guidelines’ information and categorized emailed feedbacks. Critical virus transmission control points were identified, and recommendations and corrective actions were determined to reduce the risks.
3.3. Recommendations
We used the results of the HACCP method to describe critical points in the healthcare waste management of Razi Hospital, Iran, to make recommendations and corrective actions during the COVID-19 pandemic in 2020.
4. Results
4.1. Quantity of Healthcare Waste
Razi Hospital is one of the general hospitals in Ghaemshahr established in 1934. The different wards of this hospital included hospitalization, paraclinical, clinical, and COVID-19 hospitalization, with 234 active beds during the outbreak. In this regard, we classified the risk level in each critical point as follows: Direct contact, inhalation of particles, and environmental pollution.
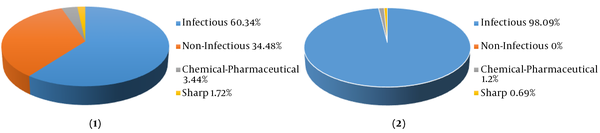
Figure 2 shows the amount of waste generated in kilograms per day. The per capita amount increased from 1.49 to 3.84 kg/day-active bed during the COVID-19 pandemic.
Amount of healthcare waste generated in kilograms per day in the studied hospital before (1) and after (2) the COVID-19 outbreak in Iran.
4.2. Hazard Analysis
In the present study, we evaluated the healthcare waste management of Razi Hospital in Ghaemshahr during the COVID-19 pandemic at different steps related to production, collection, transportation, storage, disinfection, and final disposal (Table 1). Given the prevalence of various emerging diseases in the past, poor management of COVID-19 healthcare waste may cause high transmission in communities. Among the methods mentioned, we mentioned the stage where people were in direct contact with the waste as a high-risk step. There is an exception in the final disposal where disinfection operations are performed (Table 1). The other steps listed in Table 1 have a lower risk of transmitting the COVID-19 virus.
Recommendations of HACCP Method to Describe Critical Control Points in Healthcare Waste
| Waste Management Step | Types of Healthcare Waste | Risk Levels at Critical Points for Staff (High, Medium, and Low Risk) | Recommendations and Corrective Actions | ||
|---|---|---|---|---|---|
| Direct Contact | Inhalation | Environmental Pollution | |||
| Production | Infectious | Medium | Medium | Medium | Train employees continuously and periodically in compliance with health protocols (45). Use appropriate ventilation systems in different wards (46). Dispose of non-infectious waste such as food and containers and disposable food packaging, etc. with household-like waste in landfills (47). During surgery, use full personal protective equipment and immediately place the amputated organs and fetuses in a bag carrying infectious waste (48). Do not separate syringe heads from its body and collect them together (47). Identify high susceptible surfaces and use disinfection frequently to decontaminate them (49). Dispose infectious wastes such as masks, gauze, and gloves in yellow plastic leak-proof litter bin with a special label and a safety box that can be autoclaved (50). Use red bins and garbage bags of healthcare waste for collection and temporary storage (50). Do not close plastic bags after filling (2/3) with a stapler or other methods that cause perforation, and immediately after collection, put in a new plastic bag (51). Tie the lid of the garbage bag properly to reduce the risk of spreading viruses when collecting waste (51). |
| Chemical-pharmaceutical | Low | Low | Low | ||
| Sharp | Medium | Low | Low | ||
| Collection | Infectious | High | High | High | After finishing work, remove your gloves gently to avoid spilling contaminated liquids (47). Store sharp wastes in washable yellow tanks and safety boxes and do not use plastic bags (51). Store medical waste separately from other types of waste (52). Provide proper ventilation with outlet control systems (53). Refrain staff from delivering unlabeled waste (47). Dispose produced waste several times a day based on the volume of generated waste or of the necessary conditions (50). Prohibite using defective and broken containers (50). Protect Medical waste in a place away from adverse conditions such as rain, snow, heat, and sunlight (52). Equip the storage room with hot and cold water systems for cleaning contaminants (47). Strictly avoid any relocation of healthcare waste containers and safety boxes, even from one room to another (47). |
| Chemical-pharmaceutical | Low | Low | Low | ||
| Sharp | Low | Low | Low | ||
| Transportation | Infectious | High | High | High | Use 20 g per litter chlorine (for 2 hours) for decontamination of vehicles which transport infectious waste (47). Use carts which do not have sharp edges for easy loading (47). Do not use shooting systems for transferring healthcare waste to the storage room (51). Cover the roof of the waste transportation vehicle completely (47). Insert the international symbol for transporting waste and license number on the vehicle (47). Do not use vehicles to transport other materials or general waste. Use transportation vehicles with proportional volume (internal height about 2.2 meters and the driver's room should be separated). Lock the loading compartment during transportation. Prohibit the transfer of healthcare waste by the post office (47). |
| Chemical-pharmaceutical | High | High | High | ||
| Sharp | High | High | High | ||
| Storage room | Infectious | High | High | High | Design the temporary storage rooms with adequate lighting, proper ventilation, and appropriate containers near the hospital, and lock the entrance of the storage room to prevent unauthorized access (52). Protect the storage room from sunlight, animals, insects, and birds (52). Keep away the storage room from the fresh food storage or kitchen area (49). Use special warning signs for dividing the storage room (50). Use 60 to 120-liter red tanks, equipped with a durable red garbage bag, pedal, and lid with a special label of COVID-19 for temporary storage of waste (50). |
| Chemical-pharmaceutical | High | High | High | ||
| Sharp | Medium | High | Medium | ||
| Decontamination | Infectious | High | High | High | Train employees involved in the process of collecting and transporting waste (45). Use personal protective equipment such as gloves, masks, gowns, long boots, and shields when working (47). Autoclave infectious waste as soon as possible (maximum 30 minutes) (47). Use 5000 mg per litter chlorine solution to decontaminate containers and other equipment after each step of collection and disposal of healthcare waste (47). Use alcohol (62 to 75%) and chlorine (5000 mg/liter) to decontaminate elevators after each step of transfer (47). Remove your gloves gently to avoid spilling contaminated liquids around (47). Use sodium hypochlorite (1500 ppm) for hospitals, health centers, and office environments disinfection (one-part sodium hypochlorite and 99 parts water) (47). Calibrate the autoclave at least once a year (49). |
| Chemical-pharmaceutical | High | High | High | ||
| Sharp | Medium | High | Medium | ||
| Final disposal | Infectious | Low | Low | Low | Use separate arms for landfilling healthcare waste, and perform multi-step lime spraying after landfilling (47). Dispose non-infectious and household waste daily by the relevant organization to the disposal site (50). Forbid burying chemical-pharmaceutical waste in healthcare landfills even in small quantities (52). Dispose sharp waste collected in safety boxes like infectious and chemical wastes after decontamination (47). |
| Chemical-pharmaceutical | Low | Low | Low | ||
| Sharp | Low | Low | Low | ||
4.3. Analysis of Critical Control Points
In the present study, six important steps were identified to reduce the risks of virus transmission from healthcare waste. The types of healthcare waste generated at each step were determined as high, medium, and low-risk levels similar to past studies (10). Experts through emails and extensive searches of available articles, identified risk levels for each critical point. Recommendations and corrective actions were provided separately for each step (Table 1). For all waste management steps, we must prohibit direct contact with infectious materials and use (1) medical masks and N95 masks; (2) gloves; (3) shields (eye protection) and glasses; (4) long sleeve and apron; and (5) shoe cover. According to previous studies, changes in some behaviors reduce the risk of emerging diseases.
5. Discussion
The HACCP framework enables the rapid identification of hazards associated with the type of healthcare waste at each step (10). Using risk assessment to improve the healthcare waste management system increases the awareness of the performance of health systems and environmental protection (54). Since 1960, the need for proper management has become more obvious and urgent with the increase in the production of healthcare waste in Asia (55). A study conducted during the COVID-19 pandemic in Wuhan, China, in 2020 showed that the reverse logistics network design model was used for short-term decisions to reduce the risks of transportation and disposal and the total cost of healthcare waste (18). A study in the United Kingdom showed that risk analysis at critical control points could be used to respond to infectious diseases to quickly identify hazards (56). We used the HACCP risk analysis method to describe the critical points in the healthcare waste management of Razi Hospital, Ghaemshahr, to protect the staff of different wards. The clinical profile of the virus is changing daily (57). Overcrowding is the most effective factor in the transmission of COVID-19 (58, 59). Using adequate ventilation in public places could reduce the risk of aerosols transmition (53, 60). Currently, the only way to control COVID-19 is to maintain good personal hygiene, increase immunity, and avoid to present in crowded places (61, 62).
Due to changes in the pathogenicity of COVID-19, it is possible that our recommendations and corrective actions to be change. A study in China showed the transmission of the virus from an infected person in the early steps of the disease and before the onset of symptoms (63, 64). In this regard, it is recommended to separate confirmed cases in the shortest possible time. During the pandemic, the amount of per-capita waste for each patient was higher than the average waste generated in normal conditions (65). Due to the high percentage of infection transmission from healthcare waste, it is better to dispose of it safely as soon as possible (66). According to the United Nations Environment Program, incineration at 1000°C has been recommended for residual waste to eliminate the COVID-19 virus (67). If incineration is not available, a disinfectant containing sufficient chlorine can be used for disinfection (68, 69), and a low volume of pharmaceutical waste could be incinerated with infectious waste (70). A study conducted in China recommended using more automated facilities to reduce direct contact with infectious waste and healthcare waste (71). Also, transferring the healthcare waste from a virus-infected home or care center can spread the virus to other wider environments (10). To reduce the risks of healthcare waste in the UK and other countries exposed to the virus, they developed and installed sanitation systems in hospitals and health centers (72). In the event of a pandemic, it is possible to reduce the risk of transmitting the virus by switching from traditional to automated waste treatment systems (73). Waste collection in less than two days after production and burning infectious waste with a flawless incinerator and complete combustion should be a priority in emergencies (74). Waste management is necessary because of a lack of trained personnel, transportation equipment, inadequate waste segregation, and air conditioning (75). Hazard analysis of critical control points framework was used to simplify quick responses of waste management for facing the novel infectious disease and provides recommendations and corrective actions to avoid the existing hazards. However, by the rapid change of the way of infection transmission, it will be possible that our current recommendations are modified in future research.
5.1. Conclusion
By training staff in different parts of hospitals and encouraging them to use personal protective equipment (PPE), hand washing, disinfectants, and proper ventilation, the risk of COVID-19 transmission through healthcare waste can be reduced. Appropriate training programs and awareness should be provided for developing countries with a lack of technical management systems. We can use the HACCP method to provide recommendations and corrective measures to reduce the risk of transmitting the virus during emerging epidemics.
Acknowledgements
References
-
1.
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727-33. [PubMed ID: 31978945]. [PubMed Central ID: PMC7092803]. https://doi.org/10.1056/NEJMoa2001017.
-
2.
Kahn N. New virus discovered by Chinese scientists investigating pneumonia outbreak. New York, USA: Wall Street Journal; 2020. Available from: https://www.wsj.com/articles/new-virus-discovered-by-chinese-scientists-investigating-pneumonia-outbreak-11578485668#:~:text=Chinese%20state%20media%20reported%20Thursday,needed%20to%20understand%20the%20virus..
-
3.
Lai C, Shih TP, Ko W, Tang HJ, Hsueh PR. Severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) and Coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents. 2020;55(3):105924.
-
4.
Sohrabi C, Alsafi Z, O'Neill N, Khan M, Kerwan A, Al-Jabir A, et al. World Health Organization declares global emergency: A review of the 2019 novel Coronavirus (COVID-19). Int J Surg. 2020;76:71-6. [PubMed ID: 32112977]. [PubMed Central ID: PMC7105032]. https://doi.org/10.1016/j.ijsu.2020.02.034.
-
5.
Munster VJ, Koopmans M, van Doremalen N, van Riel D, de Wit E. A Novel Coronavirus emerging in China - key questions for impact assessment. N Engl J Med. 2020;382(8):692-4. [PubMed ID: 31978293]. https://doi.org/10.1056/NEJMp2000929.
-
6.
Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet. 2020;395(10223):514-23. [PubMed ID: 31986261]. [PubMed Central ID: PMC7159286]. https://doi.org/10.1016/S0140-6736(20)30154-9.
-
7.
Askari A, Arasteh P, Jabalameli M, Bagherifard A, Razi M. COVID-19 and orthopaedic surgery: Experiences from Iran. J Bone Joint Surg Am. 2020;102(13):1126-8. [PubMed ID: 32618911]. [PubMed Central ID: PMC7224601]. https://doi.org/10.2106/JBJS.20.00631.
-
8.
Worldometer. COVID-19 Coronavirus pandemic. USA: Worldometer; 2021. Available from: https://www.worldometers.info/coronavirus/.
-
9.
Kieny MP, Evans DB, Schmets G, Kadandale S. Health-system resilience: reflections on the Ebola crisis in western Africa. Bull World Health Organ. 2014;92(12):850. [PubMed ID: 25552765]. [PubMed Central ID: PMC4264399]. https://doi.org/10.2471/BLT.14.149278.
-
10.
Edmunds KL, Elrahman SA, Bell DJ, Brainard J, Dervisevic S, Fedha TP, et al. Recommendations for dealing with waste contaminated with Ebola virus: A hazard analysis of critical control points approach. Bull World Health Organ. 2016;94(6):424-32. [PubMed ID: 27274594]. [PubMed Central ID: PMC4890207]. https://doi.org/10.2471/BLT.15.163931.
-
11.
Zand AD, Heir AV. Emanating challenges in urban and healthcare waste management in Isfahan, Iran after the outbreak of COVID-19. Environ Technol. 2021;42(2):329-36. [PubMed ID: 33331802]. https://doi.org/10.1080/09593330.2020.1866082.
-
12.
Kojima S, Kato M, Wang DH, Sakano N, Fujii M, Ogino K. Implementation of HACCP in the risk management of medical waste generated from endoscopy. J Risk Res. 2008;11(7):925-36. https://doi.org/10.1080/13669870802180613.
-
13.
Kato M, Kojima S, Masaru T. Application of HACCP to the control of medical waste generated from endoscopy. Journal of Kibi International University School of Policy Management. 2007;(3):69-77.
-
14.
Yang Z, Cao X, Liu J, Zhang L. HACCP systen in disinfection interfering process for control of infuenza A (H1N1) outbreak [J]. Chinese Journal of Disinfection. 2010;1.
-
15.
Song YJ, Bae HJ. Influence of characteristics of hospital foodservice operation and dietitian on performance of HACCP prerequisite program. Korean J Food Sci Technol. 2016;32(1):107-13. https://doi.org/10.9724/kfcs.2016.32.1.107.
-
16.
Mmanga M, Singini W, Di Bella V, Flaherty MG, Holm RH. Unpacking healthcare waste management at rural village health clinics in the Ntcheu District (Malawi). Environ Monit Assess. 2019;191(3):175. [PubMed ID: 30788632]. https://doi.org/10.1007/s10661-019-7306-6.
-
17.
Minoglou M, Komilis D. Describing health care waste generation rates using regression modeling and principal component analysis. Waste Manag. 2018;78:811-8. [PubMed ID: 32559976]. https://doi.org/10.1016/j.wasman.2018.06.053.
-
18.
Yu H, Sun X, Solvang WD, Zhao X. Reverse logistics network design for effective management of medical waste in epidemic outbreaks: Insights from the Coronavirus Disease 2019 (COVID-19) outbreak in Wuhan (China). Int J Environ Res Public Health. 2020;17(5). [PubMed ID: 32182811]. [PubMed Central ID: PMC7084373]. https://doi.org/10.3390/ijerph17051770.
-
19.
Manupati VK, Ramkumar M, Baba V, Agarwal A. Selection of the best healthcare waste disposal techniques during and post COVID-19 pandemic era. J Clean Prod. 2021;281:125175. [PubMed ID: 33223625]. [PubMed Central ID: PMC7671925]. https://doi.org/10.1016/j.jclepro.2020.125175.
-
20.
Vahidi-Kolur R, Ebrahimi MT, Jafarpour A, Kamgoo S, Aghamiri S, Kazemi AB, et al. Quantitative and qualitative assessment of waste produced in sari hospitals. J Environ Health Sci Eng. 2021;10(1):1. https://doi.org/10.4103/ijehe.ijehe_2_20.
-
21.
Zand AD, Heir AV. Environmental impacts of new Coronavirus outbreak in Iran with an emphasis on waste management sector. J Mater Cycles Waste Manag. 2020;23(1):240-7. https://doi.org/10.1007/s10163-020-01123-1.
-
22.
Ahmed I. The basel convention on the control of transboundary movements of hazardous wastes and their disposal: A legal misfit in global ship receiving jurisprudence. Wash Int'l LJ. 2019;29:411.
-
23.
Taghipour H, Mohammadyarei T, Asghari Jafarabadi M, Asl Hashemi A. On-site or off-site treatment of medical waste: A challenge. J Environ Health Sci Eng. 2014;12:68. [PubMed ID: 24739145]. [PubMed Central ID: PMC3997194]. https://doi.org/10.1186/2052-336X-12-68.
-
24.
Hong J, Zhan S, Yu Z, Hong J, Qi C. Life-cycle environmental and economic assessment of medical waste treatment. J Clean Prod. 2018;174:65-73. https://doi.org/10.1016/j.jclepro.2017.10.206.
-
25.
Kalantary RR, Jamshidi A, Mofrad MMG, Jafari AJ, Heidari N, Fallahizadeh S, et al. Effect of COVID-19 pandemic on medical waste management: A case study. J Environ Health Sci Eng. 2021:1-6. [PubMed ID: 33758671]. [PubMed Central ID: PMC7970745]. https://doi.org/10.1007/s40201-021-00650-9.
-
26.
Chauhan A. Framework for sustainable healthcare waste management in India. Transforming organizations through flexible systems management. New York, USA: Springer; 2020. p. 189-204.
-
27.
Ali M, Wang W, Chaudhry N. Management of wastes from hospitals: A case study in Pakistan. Waste Manag Res. 2016;34(1):87-90. [PubMed ID: 26628050]. https://doi.org/10.1177/0734242X15616474.
-
28.
Bourouiba L. Turbulent gas clouds and respiratory pathogen emissions: Potential implications for reducing transmission of COVID-19. JAMA. 2020;323(18):1837-8. [PubMed ID: 32215590]. https://doi.org/10.1001/jama.2020.4756.
-
29.
Conrardy J, Hillanbrand M, Myers S, Nussbaum GF. Reducing medical waste. AORN J. 2010;91(6):711-21. [PubMed ID: 20510944]. https://doi.org/10.1016/j.aorn.2009.12.029.
-
30.
Ferronato N, Ragazzi M, Torrez Elias MS, Gorritty Portillo MA, Guisbert Lizarazu EG, Torretta V. Application of healthcare waste indicators for assessing infectious waste management in Bolivia. Waste Manag Res. 2020;38(1):4-18. [PubMed ID: 31665977]. https://doi.org/10.1177/0734242X19883690.
-
31.
Verlicchi P, Galletti A, Petrovic M, Barceló D. Hospital effluents as a source of emerging pollutants: An overview of micropollutants and sustainable treatment options. Hydrology. 2010;389(3-4):416-28.
-
32.
Rolewicz-Kalińska A. Logistic constraints as a part of a sustainable medical waste management system. Transp Res Proc. 2016;16:473-82. https://doi.org/10.1016/j.trpro.2016.11.044.
-
33.
Makajic-Nikolic D, Petrovic N, Belic A, Rokvic M, Radakovic JA, Tubic V. The fault tree analysis of infectious medical waste management. J Clean Prod. 2016;113:365-73. https://doi.org/10.1016/j.jclepro.2015.11.022.
-
34.
Sarsour A, Ayoub A, Lubbad I, Omran A, Shahrour I. Assessment of medical waste management within selected hospitals in Gaza strip palestine: A pilot study. Int J Environ Sci. 2014;2(5):164-73. https://doi.org/10.12983/ijsres-2014-p0164-0173.
-
35.
Çalıs S, Arkan B. The views of the nursing students about the medical wastes and their effects on the environmental and human health. Procedia Soc Behav Sci. 2014;116:1472-6.
-
36.
Chowdhary P, Raj A, Bharagava RN. Environmental pollution and health hazards from distillery wastewater and treatment approaches to combat the environmental threats: A review. Chemosphere. 2018;194:229-46. [PubMed ID: 29207355]. https://doi.org/10.1016/j.chemosphere.2017.11.163.
-
37.
Al-Khatib IA, Khalaf AS, Al-Sari MI, Anayah F. Medical waste management at three hospitals in Jenin district, Palestine. Environ Monit Assess. 2019;192(1):10. [PubMed ID: 31807921]. https://doi.org/10.1007/s10661-019-7992-0.
-
38.
Windfeld ES, Brooks MS. Medical waste management - A review. J Environ Manage. 2015;163:98-108. [PubMed ID: 26301686]. https://doi.org/10.1016/j.jenvman.2015.08.013.
-
39.
World Health Organization. Modes of transmission of virus causing COVID-19: Implications for IPC precaution recommendations: scientific brief. Geneva, Switzerland: World Health Organization; 2020.
-
40.
Bokhoree C, Beeharry Y, Makoondlall-Chadee T, Doobah T, Soomary N. Assessment of environmental and health risks associated with the management of medical waste in Mauritius. Apcbee Procedia. 2014;9:36-41.
-
41.
Hasan MJ, Uddin R, Islam GR. A structural modeling to understand the relationship among food safety knowledge, attitude, and self-reported HACCP practices in restaurant employees in Bangladesh. Research Square. 2021;Preprint.
-
42.
Djekic I, Nikolic A, Uzunovic M, Marijke A, Liu A, Han J, et al. Covid-19 pandemic effects on food safety - Multi-country survey study. Food Control. 2021;122:107800. [PubMed ID: 33281304]. [PubMed Central ID: PMC7707641]. https://doi.org/10.1016/j.foodcont.2020.107800.
-
43.
Soman R, Raman M. HACCP system – hazard analysis and assessment, based on ISO 22000:2005 methodology. Food Control. 2016;69:191-5. https://doi.org/10.1016/j.foodcont.2016.05.001.
-
44.
Hulebak KL, Schlosser W. Hazard analysis and critical control point (HACCP) history and conceptual overview. Risk Anal. 2002;22(3):547-52. [PubMed ID: 12088233]. https://doi.org/10.1111/0272-4332.00038.
-
45.
Bodie MT, McMahon M. Employee testing, tracing, and disclosure as a response to the coronavirus pandemic. Washington University Journal of Law and Policy. 2020;64.
-
46.
de Man P, Paltansing S, Ong DSY, Vaessen N, van Nielen G, Koeleman JGM. Outbreak of Coronavirus disease 2019 (COVID-19) in a nursing home associated with aerosol transmission as a result of inadequate ventilation. Clin Infect Dis. 2021;73(1):170-1. [PubMed ID: 32857130]. [PubMed Central ID: PMC7499506]. https://doi.org/10.1093/cid/ciaa1270.
-
47.
Vice-Chancellor in Treatment Affairs. [Waste management guidelines in post-treatment care centers for corona patients]. Tehran, Iran: Shahid Beheshti University of Medical Sciences; 2021. Persian. Available from: http://treatment.sbmu.ac.ir/index.jsp?pageid=63989&p=1.
-
48.
Haque MS, Uddin S, Sayem SM, Mohib KM. Coronavirus disease 2019 (COVID-19) induced waste scenario: A short overview. J Environ Chem Eng. 2021;9(1):104660. [PubMed ID: 33194544]. [PubMed Central ID: PMC7648514]. https://doi.org/10.1016/j.jece.2020.104660.
-
49.
Ministry of Health and Medical Education. [Country guidelines (nCoV-2019) new coronavirus]. Tehran, Iran: Ministry of Health and Medical Education; 2019. Persian.
-
50.
World Health Organization. Water, sanitation, hygiene and waste management for COVID-19: Technical brief. Geneva, Switzerland: World Health Organization; 2020.
-
51.
Stericycle. Coronavirus disease (COVID-19) – regulated medical waste and sharps packaging guidance. Illinois, USA: Stericycle; 2020. Available from: http://www.tnpatientsafety.com/pubfiles/covid-19/medicalwasteguidance.pdf.
-
52.
Ministry of Health and Medical Education. [Guide to chemical and pharmaceutical waste management in health centers]. Tehran, Iran: Ministry of Health and Medical Education; 2016. Persian. Available from: https://darman.umsu.ac.ir/uploads/%D9%85%D8%AF%DB%8C%D8%B1%DB%8C%D8%AA_%D9%BE%D8%B3%D9%85%D8%A7%D9%86%D8%AF.pdf.
-
53.
Morawska L, Tang JW, Bahnfleth W, Bluyssen PM, Boerstra A, Buonanno G, et al. How can airborne transmission of COVID-19 indoors be minimised? Environ Int. 2020;142:105832. [PubMed ID: 32521345]. [PubMed Central ID: PMC7250761]. https://doi.org/10.1016/j.envint.2020.105832.
-
54.
Morovati P, Gholami Borujeni F. Risk assessment of healthcare waste by preliminary hazard analysis method. J Community Health Res. 2017;3(2):26-34.
-
55.
Ananth AP, Prashanthini V, Visvanathan C. Healthcare waste management in Asia. Waste Manag. 2010;30(1):154-61. [PubMed ID: 19726174]. https://doi.org/10.1016/j.wasman.2009.07.018.
-
56.
Edmunds KL, Hunter PR, Few R, Bell DJ. Hazard analysis of critical control points assessment as a tool to respond to emerging infectious disease outbreaks. PLoS One. 2013;8(8). e72279. [PubMed ID: 23967294]. [PubMed Central ID: PMC3743774]. https://doi.org/10.1371/journal.pone.0072279.
-
57.
Shahyad S, Mohammadi MT. Psychological impacts of COVID-19 outbreak on mental health status of society individuals: A narrative review. Mil Med. 2020;22(2):184-92.
-
58.
Hu M, Roberts JD, Azevedo GP, Milner D. The role of built and social environmental factors in COVID-19 transmission: A look at America’s capital city. Sustain Cities Soc. 2021;65:102580. https://doi.org/10.1016/j.scs.2020.102580.
-
59.
Luo L, Liu D, Liao X, Wu X, Jing Q, Zheng J, et al. Contact settings and risk for transmission in 3410 close contacts of patients with COVID-19 in Guangzhou, China : A Prospective Cohort study. Ann Intern Med. 2020;173(11):879-87. [PubMed ID: 32790510]. [PubMed Central ID: PMC7506769]. https://doi.org/10.7326/M20-2671.
-
60.
Del Rio C, Malani PN. COVID-19-new insights on a rapidly changing epidemic. JAMA. 2020;323(14):1339-40. [PubMed ID: 32108857]. https://doi.org/10.1001/jama.2020.3072.
-
61.
Taheri S. A review on Coronavirus disease (COVID-19) and what is known about it. Depiction of Health. 2020;11(1):87-93. https://doi.org/10.34172/doh.2020.09.
-
62.
Bi Q, Wu Y, Mei S, Ye C, Zou X, Zhang Z, et al. Epidemiology and transmission of COVID-19 in Shenzhen China: Analysis of 391 cases and 1,286 of their close contacts. MedRxiv. 2020;Preprint.
-
63.
Ren X, Li Y, Yang X, Li Z, Cui J, Zhu A, et al. Evidence for pre-symptomatic transmission of coronavirus disease 2019 (COVID-19) in China. Influenza Other Respir Viruses. 2021;15(1):19-26. [PubMed ID: 32767657]. [PubMed Central ID: PMC7436222]. https://doi.org/10.1111/irv.12787.
-
64.
Singanayagam A, Patel M, Charlett A, Lopez Bernal J, Saliba V, Ellis J, et al. Duration of infectiousness and correlation with RT-PCR cycle threshold values in cases of COVID-19, England, January to May 2020. Euro Surveill. 2020;25(32). [PubMed ID: 32794447]. [PubMed Central ID: PMC7427302]. https://doi.org/10.2807/1560-7917.ES.2020.25.32.2001483.
-
65.
Abu Qdais H, Rabi A, Abdulla F. Characteristics of the medical waste generated at the Jordanian hospitals. Clean Technol Environ Policy. 2006;9(2):147-52. https://doi.org/10.1007/s10098-006-0077-0.
-
66.
Rutala WA, Sarubbi FA. Management of infectious waste from hospitals. Infect Control. 1983. [PubMed ID: 6309692]. https://doi.org/10.1017/s0195941700058227.
-
67.
Sarkodie SA, Owusu PA. Impact of COVID-19 pandemic on waste management. Environ Dev Sustain. 2020. [PubMed ID: 32863738]. [PubMed Central ID: PMC7447614]. https://doi.org/10.1007/s10668-020-00956-y.
-
68.
Wang J, Shen J, Ye D, Yan X, Zhang Y, Yang W, et al. Disinfection technology of hospital wastes and wastewater: Suggestions for disinfection strategy during Coronavirus disease 2019 (COVID-19) pandemic in China. Environ Pollut. 2020;262:114665. [PubMed ID: 32443202]. [PubMed Central ID: PMC7194566]. https://doi.org/10.1016/j.envpol.2020.114665.
-
69.
Liu S, Ren N, Li CH, Shan SJ, Miao FY, Yang L, et al. Status of management of medical waste in 125 medical institutions. Chin J Nosocomiol. 2017;27:4265-9.
-
70.
Zhang YN, Song H, Zhang FE, Guo XY. Comparison of influence of oraganic substances specified in two editions of" technical standard for disinfection" on evaluation of germicidal efficacy of disinfectants. Chinese Journal of Disinfection. 2005;3.
-
71.
Singh N, Tang Y, Zhang Z, Zheng C. COVID-19 waste management: Effective and successful measures in Wuhan, China. Resour Conserv Recycl. 2020;163:105071. [PubMed ID: 32834489]. [PubMed Central ID: PMC7383137]. https://doi.org/10.1016/j.resconrec.2020.105071.
-
72.
You S, Sonne C, Ok YS. COVID-19's unsustainable waste management. Science. 2020;368(6498):1438. [PubMed ID: 32587012]. https://doi.org/10.1126/science.abc7778.
-
73.
Sharma HB, Vanapalli KR, Cheela VS, Ranjan VP, Jaglan AK, Dubey B, et al. Challenges, opportunities, and innovations for effective solid waste management during and post COVID-19 pandemic. Resour Conserv Recycl. 2020;162:105052. [PubMed ID: 32834486]. [PubMed Central ID: PMC7362850]. https://doi.org/10.1016/j.resconrec.2020.105052.
-
74.
Nugraha C. Tinjauan kebijakan pengelolaan limbah medis infeksius penanganan Corona Virus Disease 2019 (COVID-19). Jurnal Untuk Masyarakat Sehat (JUKMAS). 2020;4(2):216-29.
-
75.
Morovati P, GholamiBorujeni F. Risk assessment of healthcare waste by preliminary hazard analysis method. J Community Health Res. 2017;3(2):26-34.