Abstract
Background:
Previous Algerian epidemiologic studies have revealed that obesity has become an epidemic in many parts of the community, due to the cumulative body mass index (BMI) allied to upper total cholesterol and low-density lipoprotein (LDL) cholesterol asserting by medical scholarships in these topics.Objectives:
This study aimed at evaluating the association between anthropometric risk index with lipid profiles among some Algerian females.Methods:
This case-control study was performed female workers and spinster at the OPAPS laboratory during academic years 2015 and 2016. All participants in this study accepted venous blood withdrawal under fasting conditions and anthropometric measurement (weight, height, waist size (WC) and BMI). The SPSS 22 software using Levene’s statistic, independent t-test and the stepwise multiple linear regression was performed on the data.Results:
The samples included 36 females; 18 spinsters and 18 married, their average age was 22.75 ± 2.56 years, weight ≈ 65.52 ± 4.58, BMI ≈ 25.15 ± 2.10, ABSI ≈ 0.07 ± 0.01, ABSIz ≈ -0.38 ± 0.09, TC (g/L) 1.28 ± 0.12, and TG ≈ 1.11 ± 0.17. The homogeneity of the 2 groups was based on administrative workers with the same education, the social status, age, and weight categories. On the basis of the laboratory results, records with applied anthropometric measurements as a protocol, were used in this experiment. The practical statistics with a significant set at 0.05, confirmed that total cholesterol (LDL and HDL) level as part of lipid profile increased with increasing BMI in married females in contrast to spinsters. To predict the health risk, it is important to take into account the amount of fat and calculate the cumulative risk index based on all relevant measurements and indicators, such as ABSI and ABSI z-score to capture the risk profile associated with body size and shape.Conclusions:
On the basis of anthropometric characters related to blood test practice, lower lipid profile was in the benefit of spinsters. The results indicate that upper lipid profile control by BMI and ABSI was inversely associated with HDL and TG. Established by the association between upper quartile of ABSI related to BMI and both HDL and TG interpret in the case of this study to the side effects of oral contraceptives causing a decrease in Apoprotein, cholesterol, HDL, triglycerides reported the case of married females. In contrast, the conclusions are in agreement with similar studies, which advised a positive relationship between upper quartile of ABSI related to BMI and triglycerides related to lower HDL cholesterol and its relationship to lipoprotein lipase activity as part of lipid profile associated with obesity as a health risk in the benefit of married versus spinster females.Keywords
1. Background
Several studies from Eastern Mediterranean show that fat has reached alarming levels in adult males and females, accounting for more than 50% of the causes of death. It has been confirmed by the world health organization that obesity could put the Arab population at risk of developing non-communicable diseases (NCD) including the Algerian community.
Considering the above points, the intervention of the present study was based on the effect of weight on serum lipids, which is often overlooked in clinical practice (1). However, this practice requires the assistance of laboratory analyses, which makes it a very expensive method. In contrast anthropometric parameters, such as BMI, waist size (WC) and waist size-to-hip ratio (WHR), are clinical measurements with good interpretations, which could be used as a cheap method, especially in a developing countries like Algeria where obesity is becoming a public health problem and it is expected to worsen as its prevalence is increasing (2). Several data have reported that obesity is related to Upper BMI associated at all ages with an upper plasma triglyceride level, lower HDL cholesterol level, and greater total and non-HDL cholesterol levels, which contributes to the development of metabolic syndrome (3). While comparing the excess mortality hazard from high ABSI posed by high BMI and WC (4), it has been claimed that ABSI is a better measure of total cholesterol, LDL-cholesterol, and non-HDL-cholesterol (5).
2. Objectives
Anthropometric preventative measures are simple tools with good reproducibility, recommended for developing country (6). However, studies in this regard have been limited by the underrepresentation of obese subjects according to Shamai L, et al. (2011) (7). On this basis, the intervention of this study was limited in the interpretation of the analysis of medical assessments; it is hypothesized to expect:
-Variance in lipid profiles amongst the married and spinster females (anthropometric and biochemical).
To assess the objectives, this controlled study was based on linking female workers, married versus spinster, considering homogeneity. The sample consisted of administrative workers with the same education and social status (no children). The only difference between them was being married and its associated circumstances, such as the use of birth control (8) for family planning (9-11). The first word of warning about possible side effects from oral contraceptive use emerged from the United Kingdom, where an increased risk of heart disease (12), weight gain, fluid retention, and nausea was reported (13).
Moreover, The Algerian community is a Mediterranean region, where this subject is an irreproachable subject according to which knowledge of females on new contraceptive methods is still limited (14) such as the Italian population. Our involvement centred on the fact “Every medication seems to have its problems” (15). While to esteem this aim, the current study was conducted aimed to describe the correlation between lipid profiles and body mass index between married females and spinster, in order to provide baseline information for future analytical studies.
3. Methods
This study was based on the interpretation of blood tests obtained from the laboratory and their association with anthropometric characters.
3.1. Participants
This research studied a sample of 36 females; 18 spinsters and married with an average age of 22.75 ± 2.56 years. They were selected by intentional sampling since they were admitted to venous blood withdrawal under fasting conditions. All participants were healthy with good habits, and their recommended daily caloric intake ranges were from about 1600 to 2200 calories, with no engagement in intentional physical activity; the only difference between them was marriage and its commitments, the example of the use of birth control. They were all informed about processes and all delivered their written agreement.
3.2. Anthropometric Measurements
Body weight was measured to the nearest 0.1 kg and height to the nearest 0.5 cm using standard medical equipment without shoes. Body mass index was formulated from body mass (kg) divided by height (m) squared (16). A body shape index (ABSI) was collected according to the formula developed by Nir Y. Krakauer, Jesse C. Krakauer (2012) controlled by calculi ABSI z score to identify premature mortality risk level (17).
3.3. Blood Tests
Participants were asked to withdraw from physical activity with great intensity for 48 hours prior to blood sampling. Venous blood was collected after an overnight fast, in the morning at 8:00 to 8:30 a.m, in plastic tubes having anticoagulant and centrifuged at 4°C. Plasma was stored at -70°C until analysis (9).
Triacylglycerol’s (TG), total cholesterol (TC), and cholesterol were assayed calorimetrically. All variables were determined using commercial kits (laboratory of Dr. Bajaj Committee Zhana). All analyses were run in duplicates for the two groups. All results used in this research were derived from a medical assessment of the cases.
3.4. Statistical Analyses
The study was a comparative study of married females versus spinsters in the OPAPS laboratory during the academic years of 2015 to 2016; all participants agreed to venous blood withdrawal under fasting conditions and anthropometric measurements (body weight, body height, a body shape index, body mass index, and ABSI z-score to identify risk level). The data were analyzed using the SPSS 22 software Levene’s statistics, independent t-test and Pearson’s correlation coefficient
4. Results
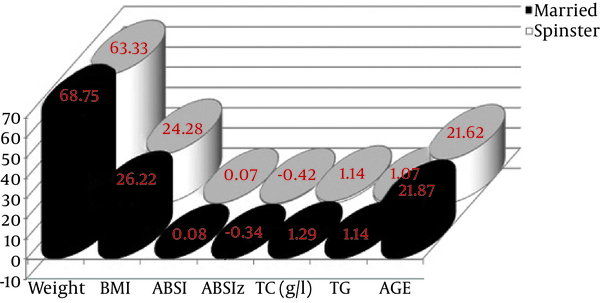
According to Figure 1, based on the norms of BMI standards, the total sample was overweight confirmed by the standards elaborated by the world health organization (WHO) (18) with low ABSI z-score, according to ABSI risk levels (17). However, triacylglycerol (TG) and total cholesterol (TC) had a good profile according to Linda Brannon and Jess Feist (19). Based on the Levene’s statistics, the total sample was homogeneous in age and weight in contrast to the other variables.
The Anthropometric Characteristics and Biochemical Variables of Married Versus Spinster Females
The Variances Between the Married and Spinster Females
| Variables | Sample | N = 36 | Means ± SD | T | Sig. | Levene Statistic | Sig. |
|---|---|---|---|---|---|---|---|
| Weight | Married | 18 | 68.75 ± 3.22 | 2.89 | 0.01 | 0.21 | 0.84 |
| Spinster | 18 | 63.33 ± 2.62 | |||||
| BMI | Married | 18 | 26.22 ± 3.11 | 4.25 | 0.00 | 5.58 | 0.00 |
| Spinster | 18 | 24.28 ± 1.17 | |||||
| ABSI | Married | 18 | 0.08 ± 0.02 | 2.185 | 0.04 | 13.62 | 0.00 |
| Spinster | 18 | 0.07 ± 0.006 | |||||
| ABSIz | Married | 18 | -0.34 ± 0.08 | 2.676 | 0.01 | 0.53 | 0.47 |
| Spinster | 18 | -0.42 ± 0.08 | |||||
| TC (g/L) | Married | 18 | 1.29 ± 0.11 | 3.12 | 0.00 | 2.36 | 0.14 |
| Spinster | 18 | 1.14 ± 0.07 | |||||
| TG | Married | 18 | 1.14 ± 0.14 | 3.19 | 0.00 | 2.62 | 0.00 |
| Spinster | 18 | 1.07 ± 0.15 | |||||
| AGE | Married | 18 | 21.87 ± 1.02 | 0.69 | 0.79 | 0.72 | 0.73 |
| Spinster | 18 | 21.62 ± 0.92 |
Regarding the independent t test, the married females had higher weight, body fat, triacylglycerol (TG) and total cholesterol (TC) when compared with spinsters, which correlated with changes in BMI and ABSI levels that agrees with the WHO recommendation of anthropometric risk index inclusion in health risk evaluation (20).
Through Table 2, all the relationships analyzed between independen t variables and predictors were significant at P ≤ 0.05. From the regression analyses model 1, 2, and 3, the program showed that weight, BMI, and ABSI were able to explain changes in total cholesterol (TC).
The Multiple Stepwise Linear Regression Using Total Cholesterol as the Dependent Variable to Estimate the Most Important Factors That Influence Lipid Profile Between Married Versus Spinster Femalesa,b,c,d,e
| Model Stepwise | R | R 2 | Adjusted R 2 | Coefficients | T | P | F | P |
|---|---|---|---|---|---|---|---|---|
| 1 | 0.62 | 0.38 | 0.36 | (Constant) | 0.75 | 0.46 | 20.82 | 0.000 |
| Weight | 4.56 | 0.00 | ||||||
| 2 | 0.67 | 0.45 | 0.42 | (Constant) | 1.02 | 0.32 | 13.62 | 0.000 |
| Weight | 2.38 | 0.02 | ||||||
| BMI | 2.08 | 0.04 | ||||||
| 3 | 0.74 | 0.65 | 0.64 | (Constant) | 1.82 | 0.04 | 11.85 | 0.000 |
| Weight | 1.56 | 0.01 | ||||||
| BMI | 1.22 | 0.00 | ||||||
| ABSI | 1.04 | 0.00 |
5. Discussion
Through total cholesterol is part of lipid profile, similar studies have reported an adverse lipid profile is related to total and LDL cholesterol, triglycerides, and apolipoprotein B. Regarding Figure 1 and Table 2, the current results are in conformity with the studies, which advised that changes in lipid levels are predictors of blood pressure, total cholesterol, and body mass index (21); not limited to obese but also to overweight females. Thus, it could be suggested that lipid profiles are adversely affected, with increased triglycerides and total cholesterol, because of contraceptive pills (22), according to similar studies conducted in this field. While the contextual framework approves the current results, the lifestyle of married females, due to the cumulative body fat associated with upper total cholesterol and lower density of lipoprotein cholesterol (LDL) reported in medical schoolwork as metabolism syndrome relative to the treatment with estrogen and progestogen, the case of females taking the oral contraceptives which influence the lipids and high-density lipoprotein cholesterol concentrations (23, 24). Regarding the study of Marlene et al. it was shown that progestin component causes decreases in HDL, total cholesterol, and triglyceride levels and increases in LDL-cholesterol (25), which was suggested as a risk factor when the levels of serum cholesterol is higher than 200 mg/dL and serum triglycerides are greater than 150 mg/dL (26). In the current study, based on differences in total cholesterol relative to lipid profiles reported for married females at risk of obesity relative to the levels of BMI and ABSI as Anthropometric Risk Index measuring metabolic syndrome, the authors suggest that the use of birth control pill increased the effect of obesity (27). Regarding the design of this study and its limitations, it is suggested to use BMI and ABSI as an index of health risk defining the risk of metabolic syndrome associated with body composition and all-cause health risk (28) related to obesity/overweightness. The authors agree that the use of contraceptive pills requires practice of sports to reduce the effects of body gain (29) and the coronary heart disease risk (30). Regarding higher BMI compared to ABSIz-score, the authors approve the association of excess of body fat at all ages with a higher plasma triglyceride level, lower HDL cholesterol level, and greater total and non-HDL cholesterol levels (1, 16).
5. 1. Conclusions
The results suggest that higher BMI and ABSI are linked with a high level of lipid profile observed for married females, and their total cholesterol is associated with their higher BMI and ABSI compared to spinsters. The HDL and TG levels among married females was associated with their adverse lipid profile such that females on birth control pills are recommended to enhance their lifestyle by a healthy diet and physical programs to decrease lipid levels.
Acknowledgements
References
-
1.
Denke MA, Sempos CT, Grundy SM. Excess body weight. An underrecognized contributor to high blood cholesterol levels in white American men. Arch Intern Med. 1993;153(9):1093-103. [PubMed ID: 8481076].
-
2.
Atek M, Traissac P, El Ati J, Laid Y, Aounallah-Skhiri H, Eymard-Duvernay S, et al. Obesity and association with area of residence, gender and socio-economic factors in Algerian and Tunisian adults. PLoS One. 2013;8(10):75640. [PubMed ID: 24116063]. https://doi.org/10.1371/journal.pone.0075640.
-
3.
Hamma SA, Fergani I, Lakehal A. Oxidative Stress in Algerian Adults Obesity. J Metabolic Syndrome. 2015;4(4). https://doi.org/10.4172/2167-0943.1000188.
-
4.
Rexford S. A. Obesity epidemiology, pathogenesis, and treatment: A multidisciplinary approach apple academic press. 1 ed. CRC Press; 2014. https://doi.org/10.1201/b16443.
-
5.
Malara M, Keska A, Tkaczyk J, Lutoslawska G. Body shape index versus body mass index as correlates of health risk in young healthy sedentary men. J Transl Med. 2015;13:75. [PubMed ID: 25890016]. https://doi.org/10.1186/s12967-015-0426-z.
-
6.
Manjareeka M, Nanda S, Mishra J, Mishra S. Correlation between anthropometry and lipid profile in healthy subjects of Eastern India. J Midlife Health. 2015;6(4):164-8. [PubMed ID: 26903756]. https://doi.org/10.4103/0976-7800.172302.
-
7.
Shamai L, Lurix E, Shen M, Novaro GM, Szomstein S, Rosenthal R, et al. Association of body mass index and lipid profiles: evaluation of a broad spectrum of body mass index patients including the morbidly obese. Obes Surg. 2011;21(1):42-7. [PubMed ID: 20563664]. https://doi.org/10.1007/s11695-010-0170-7.
-
8.
Robinson M, Shipton D, Walsh D, Whyte B, McCartney G. Regional alcohol consumption and alcohol-related mortality in Great Britain: novel insights using retail sales data. BMC Public Health. 2015;15:1. [PubMed ID: 25563658]. https://doi.org/10.1186/1471-2458-15-1.
-
9.
Pier Giorgio C, Carmine N, Salvatore R, Vincenzina B, Silvia M. Davide Sonnino and The Italian EVRA Contrast Study Group. atisfaction and compliance in hormonal contraception: the result of a multicentre clinical study on women's experience with the ethinylestradiol/norelgestromin contraceptive patch in Italy. BMC Women's Health. 2009;9(18):1-11.
-
10.
Zerf M. Which causal relationship established the effect of the control technique contraceptives on weight gain case housewives newlyweds. Int J Humanities Social Sci. 2016;7(1):47-58.
-
11.
MacArthur J. Right thinking in a world gone wrong: A biblical response to today's most controversial issues US. Harvest House Publishers; 2009.
-
12.
Cole E, Esther DR, Ann MV. Menopause, me and you: The sound of women pausing UK. Routledge; 2013.
-
13.
Riewald S, Rodeo S. Science of Swimming Faster US. Human Kinetics; 2015.
-
14.
Gambera A, Corda F, Papa R, Bastianelli C, Bucciantini S, Dessole S, et al. Observational, prospective, multicentre study to evaluate the effects of counselling on the choice of combined hormonal contraceptives in Italy--the ECOS (Educational COunselling effectS) study. BMC Womens Health. 2015;15:69. [PubMed ID: 26329464]. https://doi.org/10.1186/s12905-015-0226-x.
-
15.
Chebet JJ, McMahon SA, Greenspan JA, Mosha IH, Callaghan-Koru JA, Killewo J, et al. "Every method seems to have its problems"- Perspectives on side effects of hormonal contraceptives in Morogoro Region, Tanzania. BMC Womens Health. 2015;15:97. [PubMed ID: 26530029]. https://doi.org/10.1186/s12905-015-0255-5.
-
16.
Malara M, Keska, A. Joanna Tkaczyk and Grazyna Lutosławska. Body shape index versus body mass index as correlates of health risk in young healthy sedentary men. J Translational Med. 2015;13(75):1-6.
-
17.
Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS One. 2012;7(7):39504. [PubMed ID: 22815707]. https://doi.org/10.1371/journal.pone.0039504.
-
18.
World Health Organization. World Health Statistics FR. World Health Organization; 2010.
-
19.
Brannon L, Feist J. Health psychology: An introduction to behavior and health US. Cengage Brain;
-
20.
World Health Organization. Waist circumference and waist-to-hip ratio: report of a WHO expert consultation. Geneva: WHO; 2008.
-
21.
Halter J, Ouslander J, Tinetti M. Hazzard's geriatric medicine and gerontology. Sixth ed. McGraw Hill Professional; 2008.
-
22.
Sabaratnam A, Sivanesaratnam V, Alokendu C. Essentials of gynecology US. Anshan; 2005.
-
23.
Ficalora RD, Mueller PS, Beliveau M. M.D. Mayo clinic internal medicine board review UK. Oxford University Press; 2013.
-
24.
Woo TM, Robinson MV, Davis FA. Pharmacotherapeutics for advanced practice nurse prescribers US. 2015.
-
25.
Goldman MB, Troisi R, Rexrod KM. Women and Health US. Elsevier; 2012.
-
26.
Pothuri Radha Krishna Murthy. Heart in fours: Cardiology for residents and practitioners New Delhi. Japee Brothers Medical publishers; 2013.
-
27.
Melina RK, William HP, James STY. Venous Disorders US. USA: PMPH; 2010.
-
28.
Chang Y, Guo X, Chen Y, Guo L, Li Z, Yu S, et al. A body shape index and body roundness index: two new body indices to identify diabetes mellitus among rural populations in northeast China. BMC Public Health. 2015;15:794. [PubMed ID: 26286520]. https://doi.org/10.1186/s12889-015-2150-2.
-
29.
Zerf M. Impact of preventing pregnancy methods and their relationships with the level of growth fitness body health housewife case women newlyweds. American J Sport Sci Med. 2015;3(5):90-5.
-
30.
Mokkedes MI, Zerf M. Relationship betwin hearthbeats and body composition among some fatness algerians housewives. American J Innovative Res Appl Sci. 2016;2(4):128-34.