Abstract
Background:
Being overweight is a characteristic that may influence a person’s heat exchange.Objectives:
The purpose of this study was to assess the effect of body weight on heat strain indices in hot and dry climatic conditions.Materials and Methods:
This study was completed with a sample of 30 participants with normal weights, as well as 25 participants who were overweight. The participants were physically inactive for a period of 120 minutes in a climatic chamber with hot and dry conditions (22 - 32°C and with 40% relative humidity (RH)).The physiological strain index (PSI) and heat strain score index (HSSI) questionnaires were used. Simultaneous measurements were completed during heat exposure for periods of five minutes. The resting periods acted as the initial measurements for 15 minutes.Results:
In both groups, oral temperature, heart rate, and thermal perceptual responses increased during heat exposure. The means and standard deviations of heart rate and oral temperature were gathered when participants were in hot and dry climatic conditions and were not physically active. The heart rates and oral temperatures were 79.21 ± 5.93 bpm and 36.70 ± 0.45°C, respectively, for those with normal weights. For overweight individuals, the measurements for heart rate and oral temperature reached 82.21 ± 8.9 bpm and 37.84 ± 0.37°C, respectively.Conclusions:
The results showed that, compared to participants with normal weights, physiological and thermal perceptual responses were higher in overweight participants. Therefore, overweight individuals should avoid hot/dry weather conditions to decrease the amount of heat strain.Keywords
Body Mass Index (BMI) Heat Strain Indices Climatic Conditions Overweight
1. Background
One of the consequences of heat exposure in the workplace is heat strain. There are several factors affecting heat strain, such as dry temperatures, wet bulb temperature, radiant temperature, metabolic rate, age, gender, BMI, and clothing type (1-4). The onset of heat stress in a human can reduce productivity and lead to heat exhaustion. Therefore, it is essential to evaluate the amount of heat-induced physiological strain that a person can tolerate during different activities (5, 6). Physiological research has identified personal factors associated with the degree to which an individual is susceptible to heat stress, including age, gender, race, physical fitness, obesity, hydration, medication, personal acclimatization capacity, clothing type, as well as whether or not an individual smokes (7, 8). Those who are obese commonly experience heat-related illnesses (HRIs). BMI is a useful factor for determining obesity (9). The PSI was developed to evaluate heat and physiological strain by measuring heart rate (HR) and core body temperature (10). The HSSI, established and evaluated by Dehghan et al. is an index that evaluates emotional and perceptual variables using questionnaire. This index has been used to assess heat strain in Iranian women and men in hot work environments (11). The HSSI index includes variable, observational, and subjective questions related to heat stress, including thermal and humidity sensations (12), intensity of sweating (3, 13), the degree of impact from heat (14), physical dimensions of the workspace (15), exposure of the face to heat, surrounding surface temperature, air movement, and other factors that influence heat strain.
2. Objectives
The purpose of this study was to assess the effect of body weight on heat strain indices in hot/dry climatic conditions.
3. Materials and Methods
3.1. Subjects
The participants were classified into two groups based on BMI: 30 participants with normal weights (BMI of 20-25 kg/m-2) and 25 overweight participants (BMI of 25.1-30 kg/m-2) (16, 17). No-participants experienced medical issues six months prior to the study. The subjects were informed of the nature of the study and the potential risks of exercising in a hot climate. The participants were asked to signa volunteer consent form. Based on the recommendations of an attending physician, the study was stopped at any time.
3.2. Protocol
The study was conducted in a climatic chamber (4.5 meter in length, 3.5 meter wide and 3 meter high) at the Department of Occupational Health Engineering at Isfahan University of Medical Sciences in Isfahan, Iran. All of the subjects wore the same clothing (shirts, pants, and socks). The details of the materials used in clothing for Iranian men, including the weights of individual garments, fabric composition, and body surface area coverage, are presented in Table 1.
| Clothing Ensembles | Body Surface Area Coverage | Weight, gr/m2 | The Density of Warp Yarns, cm-1 | The Density of Weft Yarns, cm-1 | Insulation Values | |
|---|---|---|---|---|---|---|
| Clothing Insulation | M2° CW-1 | |||||
| Islamic summer clothing | 223.15 | 31 | 24 | 0.80 | 0.123 | |
| Pants | 45 | |||||
| Shirts | 61 | |||||
| Socks | 7 | |||||
3.3. Environmental Conditions
The subjects exercised in a hot, dry climate (between 22 and 32°C and 40% RH) for 120 minutes. After 15 minutes of rest on a bed outside the climate chamber, the subjects returned to the chamber and were physically inactive (seated).
3.4. Measurements
During periods of rests and heat exposure, heart rate and oral temperature were monitored and recorded at 5 minutes intervals (these measurements were made every five minutes). Heart rate was measured using a Polar heart rate monitor (Polar Electro RS100, Finland) (3). Oral temperature was measure dusinga medical digital thermometer (Digital Thermometer, Omron). The wet bulb globe temperature (WBGT) index was also measured (18) during periods of rest and exposure using ahead stress monitor (Micro herm WBGT, Casella, United Kingdom). The heights (meters) and weights (kilograms) of the participants were recorded and converted into BMI values (kg/m-2).
The ratings from the HSSI were gathered using questionnaire-validated scales that the participants completed at 5 minutes intervals during periods of rest and heat exposure (the periods of exposure last for five minutes). This process was used to measure several physiological parameters simultaneously. As a measure of physiological strain, coincident oral temperature and heart rate measurements were used to create the PSI (9). In this study, oral temperature was calculated to represent core body temperature (Trek), as rectal temperature measurement was not possible (11).
3.5. Statistical Analysis
With the use of SPSS16, the data were analyzed using descriptive statistics and a one-way analysis of variance (ANOVA). Heat radiation was not present in the climatic chamber. Prior to beginning this study, approval was obtained from the Medical Ethics Committee of Isfahan University of Medical Sciences. All procedures were in agreement with the Helsinki declaration.
4. Results
The subjects of this study were 55 healthy adult males. The demographic and physiological characteristics of the subjects, including Mean ± SD, are presented in Table 2.
| Demographic and Physiological Characteristics | Normal Weight (n = 30) | Overweight (n = 25) |
|---|---|---|
| Age, y | 23.34 ± 1.6 | 25.66 ± 1.39 |
| Height, m | 1.74 ± 5.61 | 1.75 ± 5.61 |
| Weight, kg | 63.34 ± 8.34 | 82.01 ± 6.09 |
| Waist size, cm | 78.50 ± 5.99 | 94.86 ± 6.43 |
| BMI, kg/m-2 | 20.70 ± 2.52 | 26.570 ± 0.95 |
| Heart rate, bpm | ||
| Resting | 73.38 ± 9.74 | 75.98 ± 11.38 |
| Seated | 79.21 ± 5.93 | 82.21 ± 8.9 |
| Oral temperature, °C | ||
| Resting | 36.92 ± 0.35 | 36.71 ± 0.41 |
| Seated | 36.70 ± 0.45 | 37.84 ± 0.37 |
The oral temperature ranged from 0.3 to 0.7°C lower than core body temperature, averaging at around 0.5°C. national institute of occupational safety and health (NIOSH ) and the world health organization (WHO) recommend that core body temperature remain below 38°C (9).
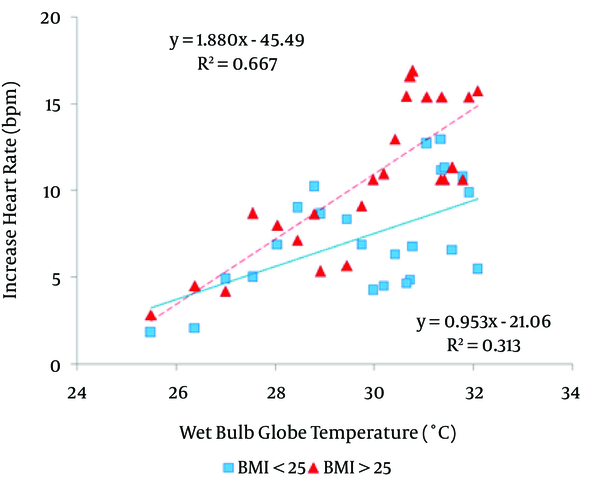
The relationship between the WBGT index and HR was evaluated during periods of limited physical activity lasting 120 minutes in the normal weight and overweight groups. During periods of limited physical activity in hot conditions, the heart rates in the overweight group were similar to those of the normal weight group in low temperatures prior to heat exposure. The heart rates increased gradually over the last 120 minutes in both groups. However, compared to those with normal weights, the heart rates of the overweight participants were higher (Figure 1).
A scatter Plot Showing The Relationship Between the WBGT Index and Heart Rates in The Normal Weight and Overweight Groups
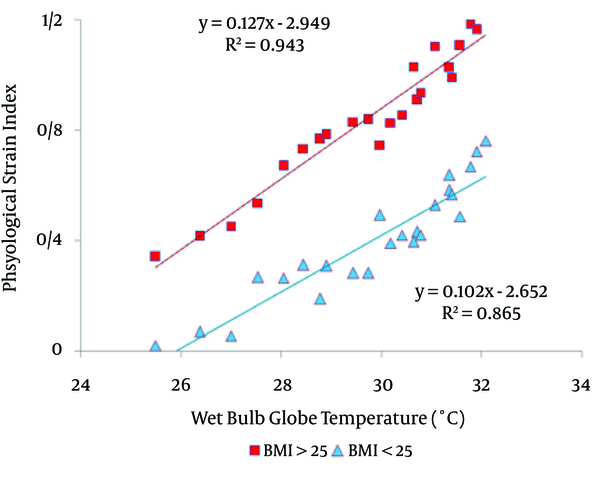
In terms of the relationship between the WBGT index and the PSI during periods of low physical exertion for 120 minutes, increases in the PSI were greater in participants who were overweight compared to those with normal weights (Figure 2).
A scatter Plot Showing The Relationship Between The WBGT Index and The PSI in Normal Weight and Overweight Groups
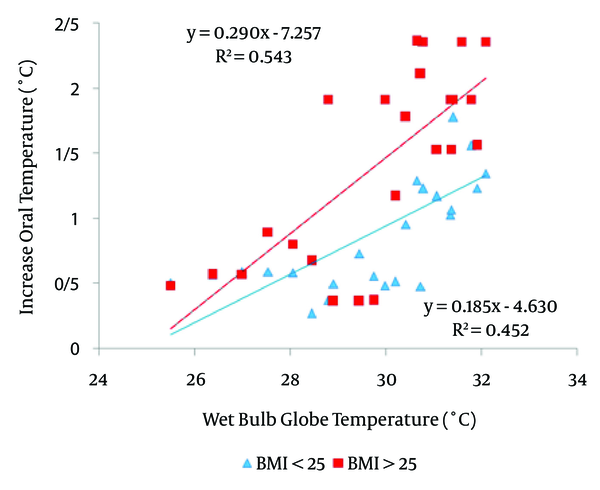
According to the relationship between the WBGT index and oral temperature, increases in oral temperature were higher in overweight participants compared to those with normal weights. This portion of the experiment included periods of low physical exertion for 120 minutes (Figure 3).
The Relationship Between The WBGT Index and Oral Temperature in The Normal Weight and Overweight Groups
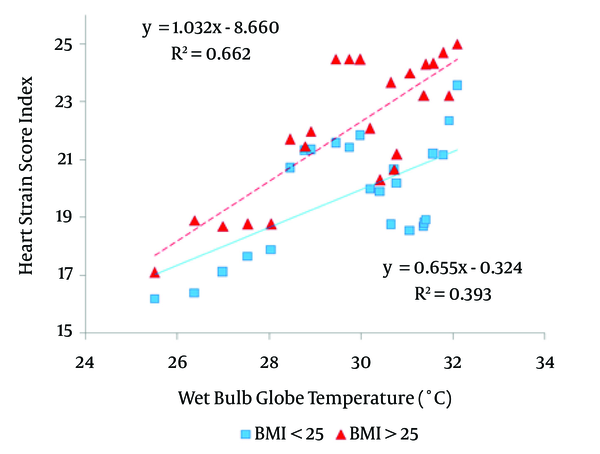
When evaluating the relationship between the WBGT index and the HSSI, the results show that the increase in the HSSI was greater in the overweight group in comparison to the normal weight group (Figure 4).This evaluation was completed during a period of low physical activity for 120 minutes.
The Relationship Between WBGT Index and HSSI in The Normal Weight and Overweight Groups
5. Discussion
Obesity is often associated with poor heat tolerance. Therefore, the main aim of this study was to measure the effect of being overweight on heat strain indices in hot and dry climates. The study used analytical indices (the PSI), empirical indices (WBGT index), and thermal perceptual indices (HSSI) (11, 19, 20). When the environmental temperature was above physiological responses, the subjects absorbed heat from the environment and relied entirely on perspiration for heat loss (21). In many studies, age and BMI are considered heat stress risk factors (22, 23). Dehghan et al. (15) conducted a cross-sectional study comparing cardiac strain among workers in the Persian Gulf with normal weights and those who were overweight. The study, the authors reported that the average resting heart rates and working heart rates of overweight individuals were significantly higher than the heart rates of individuals with normal weights (15). The results showed that, no significant difference in mean heart rate, oral temperature, and HSSI levels between the normal weight group and the overweight group. These rates were measured during periods of low physical exertion in climatic conditions (The study was conducted in a climatic chamber (4.5 meters in length, 3.5 meters wide, and 3 meters high) at the department of occupational health engineering at Isfahan University of Medical Sciences in Isfahan, Iran), both of which may influence the results.
In a study conducted by Donoghue et al. (24) on the risks of heat exhaustion, heat exhaustion experienced by individuals with high BMIs (32-36.99 kg/m-2) was 3.63 compared to heat exhaustion in individuals with BMIs lower than 27 kg/m-2. These finding indicates that individuals with a higher BMI are at greater risk for heat stroke. Figure 1 shows that, as BMI increases, heart rate also increases.
Yazdanirad et al. (25) completed a study on the heart rates of overweight individuals in hot weather when engaging in light to moderate exercise under controlled conditions. In this study, the authors reported that the mean heart rate was higher in participants who were overweight. The results of our study revealed that, during a period of low physical exertion, the mean heart rate was higher in participants who were overweight than those with normal weight.
Tuomaala et al. (26) studied the effects of individual characteristics and BMI on ratings of thermal sensation (RTS) using predicted mean vote (PMV). The authors did not identify a correlation between thermal sensation and BMI < 25. These results are consistent with the findings of the present study.
Michael Gallagher et al. (27) used the perceptual hyperthermia index to study heat strain when participants exercised using treadmill. In this study, the authors reported that core body temperature, heart rate, rate of perceived exertion (RPE), and increases in thermal sensation were greater in participants with mean BMIs of 30.1 ± 5.4 compared to participants with mean BMIs of 25.1 ± 4.0 (the results of our study showed that the emotional and perceptual variables of the HSSI index, which included the main parameters (such as thermal sensation and rate of physical exertion) of heat strain, core body temperature, and HR during exposure to heat stress, were higher in overweight participants when they were seated. At lower temperatures, the heart rates had minimal influences on other physiological variables. However, at higher temperatures, overweight subjects experienced higher heart rates because of heat transfer and greater blood flow restriction. Therefore, compared to subjects with normal weights, the risk of heat strain is greater in overweight subjects.
The results indicated that physiological and thermal perceptual responses to heat strain were higher in overweight participants. To decrease heat strain, overweight individuals should avoid hot and dry weather conditions.
Acknowledgements
References
-
1.
Basu R, Samet JM. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol Rev. 2002;24(2):190-202. [PubMed ID: 12762092].
-
2.
Glazer JL. Management of heatstroke and heat exhaustion. Am Fam Physician. 2005;71(11):2133-40. [PubMed ID: 15952443].
-
3.
Moran DS, Shapiro Y, Laor A, Izraeli S, Pandolf KB. Can gender differences during exercise-heat stress be assessed by the physiological strain index? Am J Physiol. 1999;276(6 Pt 2):R1798-804. [PubMed ID: 10362762].
-
4.
Tikuisis P, McLellan TM, Selkirk G. Perceptual versus physiological heat strain during exercise-heat stress. Med Sci Sports Exerc. 2002;34(9):1454-61. [PubMed ID: 12218738]. https://doi.org/10.1249/01.mss.0000027764.43430.fe.
-
5.
Pandolf KB, Stroschein LA, Drolet LL, Gonzalez RR, Sawka MN. Prediction modeling of physiological responses and human performance in the heat. Comput Biol Med. 1986;16(5):319-29. [PubMed ID: 3769464].
-
6.
Lindgren E, Albihn A, Andersson Y, Forsberg B, Olsson G, Rocklov J. [Consequences of climate changes for the health status in Sweden. Heat waves and disease transmission most alarming]. Lakartidningen. 2008;105(28-29):2018-23. [PubMed ID: 18710157].
-
7.
Islam MZ. Influence of gender on heart rate and core temperature at critical wbgt for five clothing ensembles at three levels of metabolic rate. uni south florida: Scholar Commons; 2005. Available from: http://scholarcommons.usf.edu/etd/2933.
-
8.
Rowlinson S, Yunyanjia A, Li B, Chuanjingju C. Management of climatic heat stress risk in construction: a review of practices, methodologies, and future research. Accid Anal Prev. 2014;66:187-98. [PubMed ID: 24079394]. https://doi.org/10.1016/j.aap.2013.08.011.
-
9.
Dehghan H, Ghanbary Sartang A. Validation of Perceptual Strain Index to Evaluate the Thermal Strain in Experimental Hot Conditions. Int J Prev Med. 2015;6:78. [PubMed ID: 26425333]. https://doi.org/10.4103/2008-7802.163185.
-
10.
Moran DS, Kenney WL, Pierzga JM, Pandolf KB. Aging and assessment of physiological strain during exercise-heat stress. Am J Physiol Regul Integr Comp Physiol. 2002;282(4):R1063-9. [PubMed ID: 11893610]. https://doi.org/10.1152/ajpregu.00364.2001.
-
11.
Dehghan H, Habibi E, Habibi P, Maracy MR. Validation of a questionnaire for heat strain evaluation in women workers. Int J Prev Med. 2013;4(6):631-40. [PubMed ID: 23930180].
-
12.
Dehghan H, Mortazavi SB, Jafari MJ, Meraci M, Khavanin A, Jahangiri M. Construct validation of a heat strain score index with structural equation modeling. Health Syst Res. 2011;6(4):601-12.
-
13.
Dehghan H, Habibi E, Khodarahmi B, HA HY, Hasanzadeh A. The relationship between observational–perceptual heat strain evaluation method and environmental/physiological indices in warm workplace. Pakistan J Med Sci. 2013;29(1):358-62.
-
14.
Habibi P, Dehghan H, Rezaei S, Maghsoudi K. Thermal, physiological strain index and perceptual responses in Iranian Muslim women under Thermal Condition in order to Guide in Prevention of Heat Stress. Iran J Health Environmt. 2014;1(4):172-6.
-
15.
Dehghan H, Mortazavi SB, Jafari MJ, Maracy MR. Cardiac strain comparison between workers with normal weight and overweight in the hot humid weather of the Persian Gulf region. J Edu Health. 2013;2.
-
16.
Hartman ML, Veldhuis JD, Johnson ML, Lee MM, Alberti KG, Samojlik E, et al. Augmented growth hormone (GH) secretory burst frequency and amplitude mediate enhanced GH secretion during a two-day fast in normal men. J Clin Endocrinol Metab. 1992;74(4):757-65. [PubMed ID: 1548337]. https://doi.org/10.1210/jcem.74.4.1548337.
-
17.
Tunc O, Bakos HW, Tremellen K. Impact of body mass index on seminal oxidative stress. Andrologia. 2011;43(2):121-8. [PubMed ID: 21382066]. https://doi.org/10.1111/j.1439-0272.2009.01032.x.
-
18.
Epstein Y, Moran DS. Thermal comfort and the heat stress indices. Ind Health. 2006;44(3):388-98. [PubMed ID: 16922182].
-
19.
Parsons K. Heat stress standard ISO 7243 and its global application. Ind Health. 2006;44(3):368-79. [PubMed ID: 16922180].
-
20.
Dehghan H, Mortazavi SB, Jafari MJ, Maracy MR. construct validation of a heat strain score index with structural equation modeling. Health System Res. 2011;6(4):601-12.
-
21.
Binkley HM, Beckett J, Casa DJ, Kleiner DM, Plummer PE. National Athletic Trainers' Association Position Statement: Exertional Heat Illnesses. J Athl Train. 2002;37(3):329-43. [PubMed ID: 12937591].
-
22.
Havenith G. Individualized model of human thermoregulation for the simulation of heat stress response. J Appl Physiol (1985). 2001;90(5):1943-54. [PubMed ID: 11299289].
-
23.
Donoghue AM, Bates GP. The risk of heat exhaustion at a deep underground metalliferous mine in relation to surface temperatures. Occup Med (Lond). 2000;50(5):334-6. [PubMed ID: 10975131].
-
24.
Donoghue AM, Bates GP. The risk of heat exhaustion at a deep underground metalliferous mine in relation to body-mass index and predicted VO2max. Occup Med (Lond). 2000;50(4):259-63. [PubMed ID: 10912377].
-
25.
Yazdanirad S, Dehghan H, Rahimi Y, Zeinodini M, Shakeriyan M. The Relationship Between Overweight and Heart Rate in Hot and Very Hot Weather Under Controlled Conditions. Health Scop j. 2015;4(4). ee30604.
-
26.
Tuomaala P, Holopainen R, Piira K, Airaksinen M. Impact of individual characteristics such as age, gender, BMI and fitness on human thermal sensation. Build Simul J. 2013:26-8.
-
27.
Gallagher MJ, Robertson RJ, Goss FL, Nagle-Stilley EF, Schafer MA, Suyama Jr M, et al. Development of a perceptual hyperthermia index to evaluate heat strain during treadmill exercise. Eur J Appl Physiol. 2012;112(6):2025-34. [PubMed ID: 21947408]. https://doi.org/10.1007/s00421-011-2173-z.