Abstract
Background:
Brucellosis is an inflammatory disease that may affect any organ or system.Objectives:
The aim of this retrospective cross-sectional study was to investigate the predictive value of novel and traditional inflammatory markers for the diagnosis of brucellosis.Methods:
The demographic characteristics and laboratory results of 55 patients with confirmed brucellosis and 60 healthy controls were analyzed and compared. Blood culture was performed using the BacT/ALERT 3D automated system. The presence of Brucella antibodies was detected by both the Brucellacapt test and Brucella Coombs gel test. Complete blood count, erythrocyte sedimentation rate (ESR), and biochemical analyzes were also performed.Results:
Compared to healthy controls, the patients with brucellosis had significantly higher high-sensitivity C-reactive protein (hsCRP), hsCRP to albumin ratio (CAR), ESR, monocyte, monocyte to high-density lipoprotein ratio (MHR), aspartate aminotransferase, creatinine levels, while had significantly lower mean platelet volume, lymphocyte to monocyte ratio, albumin, total cholesterol, and high-density lipoprotein levels. There was no significant difference between the two groups in terms of leukocyte count, neutrophil, lymphocyte, hemoglobin, red blood cell distribution width, platelet, neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, glucose, alanine aminotransferase, blood urea nitrogen, triglyceride, low-density lipoprotein levels. Positive correlations were observed between CAR, hsCRP, ESR, and MHR levels.Conclusions:
This is the first study evaluating the predictive value of CAR and MHR in the diagnosis of brucellosis. The data revealed that CAR and MHR could be used as the markers of systemic inflammation in patients with brucellosis.Keywords
1. Background
Brucellosis is a zoonotic bacterial infection caused by Brucella species and continues to be a major public health issue, especially in developing countries (1, 2). Approximately half of a million new human brucellosis infections are reported annually, and it is still endemic, mainly in the Mediterranean basin, Middle East, Latin America, Central Asia, and the Indian subcontinent (1, 3). The disease is usually transmitted by close contact with infected animals (most commonly sheep, goats, cattle, and pigs) or by consuming unpasteurized milk and milk products (2-4). Human brucellosis is a systemic inflammatory disease that can affect any organ or system of the body. Patients with brucellosis may present diverse non-specific clinical manifestations, such as fever, fatigue, sweating, arthralgia, myalgia, headache, hepatomegaly, splenomegaly, and lymphadenopathy. The definitive diagnosis frequently depends on the results of laboratory testing because there are no disease-specific pathognomonic symptoms or signs (1, 5-7).
Several bacteriological, serological, and molecular methods have been improved for the laboratory diagnosis of brucellosis. Each of these methods has advantages and limitations and needs careful interpretation. Although bacterial culture is accepted as the superior diagnostic method, the isolation rate of Brucella spp. varies based on the disease stage, previous antibiotic use, clinical sample, and the culture technique, and culture is generally unsuccessful owing to the inability to provide optimum culture conditions (1, 6, 8). Therefore, serological tests are more widely used as diagnostic and screening tools in routine laboratory practice. However, serological tests sometimes yield false positive or negative results due to cross-reactions with other Gram-negative bacteria, the presence of blocking antibodies, or high antibody titers interfering with the antigen-antibody complex formation known as the prozone phenomenon (4, 8-10). Polymerase chain reaction (PCR) has been demonstrated to be more sensitive and specific than culture and serological methods in the laboratory diagnosis of brucellosis (1, 6). Nevertheless, due to the high costs, and long and labor-intensive process, PCR assays are not appropriate for widespread use in many medical laboratories, particularly in developing countries.
Because of the difficulties in the clinical and laboratory diagnosis of brucellosis, identifying novel, specific, and cost-effective biomarkers is important for resolving the diagnostic obstacles, especially in endemic regions. The systemic inflammatory burden could be evaluated using various biomarkers. Increased values of C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), two well-known acute phase reactants, have been usually reported in patients as a result of inflammatory response in brucellosis (7, 8, 11-14). The CRP to albumin ratio (CAR), obtained by dividing CRP by albumin, is a new biomarker extensively studied as a diagnostic and prognostic tool in various diseases (15-18). In recent years, hematological and biochemical parameters, such as neutrophil to lymphocyte ratio (NLR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR), and monocyte to high-density lipoprotein ratio (MHR), have been investigated as potential indicators of systemic inflammation in several infectious and non-infectious diseases (7, 11, 19-23). These inflammatory markers are broadly available and affordable parameters that can be easily calculated based on routine complete blood count (CBC) and biochemical analysis.
2. Objectives
The present study aimed to evaluate the predictive performance of novel and traditional inflammation markers to diagnose brucellosis and guide clinicians in the diagnostic process.
3. Methods
This retrospective cross-sectional study was conducted at Suleyman Demirel University Research and Practice Hospital, Isparta, Turkey. The medical records of patients with brucellosis and healthy controls who were admitted to the inpatient/outpatient clinics of the hospital during July 2018 - January 2020 were analyzed.
3.1. Patients and Controls
Fifty-five patients with newly diagnosed brucellosis and 60 healthy controls with similar age and gender distribution were enrolled in the study. Participants with any autoimmune disease, malignancy, severe chronic disease, and recent infectious disease were excluded from the study. In the patient group, the diagnosis of brucellosis was based on bacteriological, serological, and clinical data according to the Centers for Disease Control and Prevention (CDC) reference guidelines and previous reports (6-8, 11-14, 20, 21, 24). Confirmed brucellosis was defined as the positivity of blood culture for Brucella spp. and/or serological test positivity (a four-fold or greater rise in antibody titer between two serum specimens obtained at least two weeks apart) by both serological methods in the presence of compatible clinical symptoms, signs, and anamnesis. Presumptive brucellosis was defined as serological test positivity (a single antibody titer ≥ 1/320) in the presence of clinical symptoms, signs, and anamnesis. All participants in the patient group met the criteria for confirmed brucellosis and received specific antimicrobial therapy (a combination of doxycycline and rifampin or streptomycin for 6 weeks). The control group consisted of healthy volunteers attending outpatient clinics for a routine health check-ups. None of the control subjects met the criteria for confirmed or presumptive brucellosis.
3.2. Laboratory Analysis
Venous blood samples (5 - 8 mL) were obtained from each participant and were centrifuged before analysis. The specific antibodies against Brucella infection were detected by the Brucellacapt test (Vircell, Granada, Spain) and Brucella Coombs gel test (Across Gel, Dia Pro, Turkey). The serum samples were analyzed at the dilutions of 1/20 - 1/5120. The assays were performed according to the manufacturer’s instructions. Antibody titers at 1/320 and higher for both serological methods were interpreted as a positive reaction for brucellosis, while those lower than 1/320 were interpreted as negative.
Blood cultures were processed using the BacT/ALERT 3D (bioMérieux, France) automated blood culture system. The isolated bacterial strains were identified by conventional methods (colony morphology, Gram staining, biochemical tests, oxidase, and urease tests). Serum biochemical parameters were analyzed using Beckman Coulter AU5800 clinical chemistry analyzer (Beckman Coulter, Brea, USA). The CBC and ESR measurements were performed using Beckman Coulter UniCel DxH 800 hematology analyzer (Beckman Coulter, Brea, USA) and Test-1 analyzer (Alifax, Padova, Italy), respectively. For CBC and ESR analyzes, blood specimens withdrawn from each participant were collected in blood tubes containing citrate or ethylenediaminetetraacetic acid. All assays were performed according to the manufacturers’ recommendations. The values of CAR, NLR, LMR, PLR, and MHR were calculated based on CBC and biochemical analysis.
3.3. Statistical Analysis
The SPSS software version 22 was used for statistical analysis (SPSS Inc., Chicago, IL, USA). The continuous variables were compared between the groups utilizing the Mann-Whitney U test or Student's t-test. Categorical variables were compared using the chi-square test. Results of descriptive statistics were presented as frequency and percentage, or mean ± standard deviation. Moreover, receiver operating characteristic (ROC) curves were plotted for significant variables, and the areas under the ROC curve (AUC-ROC) values with 95% CI were calculated. The optimal cut-off values were identified for predicting brucellosis. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated. The correlations between variables were assessed by Spearman’s correlation analysis. P-value < 0.05 was considered statistically significant.
4. Results
The comparison of demographic features, including age and gender, and the results of biochemical tests, CBC, and ESR between the patient and control groups is demonstrated in Table 1. The patients with brucellosis had significantly higher hsCRP, CAR, ESR, monocyte, MHR, aspartate aminotransferase (AST), and creatinine levels compared to the controls. On the other hand, patients had significantly lower mean platelet volume (MPV), LMR, albumin, total cholesterol, and high-density lipoprotein (HDL) levels than the control group (P < 0.05). No significant difference was found in leukocyte count, neutrophil, lymphocyte, hemoglobin, red blood cell distribution width (RDW), platelet, NLR, PLR, fasting blood glucose, alanine aminotransaminase (ALT), blood urea nitrogen (BUN), triglyceride, and low-density lipoprotein (LDL) levels between the two groups (P > 0.05).
Comparison of Demographic Features and Laboratory Findings Between the Patient and Control Groups
| Patient Group (N = 55) | Control Group (N = 60) | P-Value | |
|---|---|---|---|
| Age (y) | 45.73 ± 14.85 | 49.78 ± 12.8 | 0.119 |
| Gender | 0.626 | ||
| Male | 30 (54.5) | 30 (50) | |
| Female | 25 (45.5) | 30 (50) | |
| hsCRP (mg/L) | 21.92 ± 20.25 | 2.38 ± 1.71 | < 0.001 |
| CAR | 6.06 ± 6.16 | 0.57 ± 0.41 | < 0.001 |
| ESR (mm/h) | 28.4 ± 21.51 | 9.51 ± 6.92 | < 0.001 |
| Leukocyte (×103/µL) | 7.44 ± 2.55 | 6.83 ± 2.04 | 0.159 |
| Neutrophil (×103/µL) | 4.68 ± 2.31 | 4.15 ± 1.57 | 0.146 |
| Lymphocyte (×103/µL) | 1.96 ± 0.58 | 1.97 ± 0.57 | 0.89 |
| Monocyte (×103/µL) | 0.62 ± 0.24 | 0.52 ± 0.2 | 0.015 |
| Hemoglobin (g/dL) | 13.66 ± 1.43 | 14.05 ± 1.78 | 0.201 |
| RDW (%) | 14.65 ± 1.58 | 14.56 ± 1.86 | 0.779 |
| Platelet (×103/µL) | 258.94 ± 93.34 | 255.43 ± 58.99 | 0.808 |
| MPV (fL) | 8.12 ± 0.92 | 8.53 ± 0.75 | 0.015 |
| NLR | 2.61 ± 1.52 | 2.21 ± 0.98 | 0.094 |
| LMR | 3.61 ± 1.89 | 4.17 ± 1.44 | 0.01 |
| PLR | 142.23 ± 66.04 | 137.64 ± 45.04 | 0.662 |
| MHR | 17.79 ± 7.55 | 11.82 ± 5.08 | < 0.001 |
| Glucose (mg/dL) | 101.68 ± 14.64 | 102.71 ± 32.3 | 0.829 |
| ALT (IU/L) | 26.7 ± 19.23 | 22.04 ± 10.02 | 0.103 |
| AST (IU/L) | 27.69 ± 13.37 | 22.42 ± 6.87 | 0.008 |
| BUN (mg/dL) | 14.14 ± 4.16 | 14.21 ± 3.44 | 0.92 |
| Creatinine (mg/dL) | 0.79 ± 0.17 | 0.73 ± 0.15 | 0.045 |
| Albumin (mg/dL) | 3.85 ± 0.5 | 4.16 ± 0.3 | < 0.001 |
| Triglyceride (mg/dL) | 133.97 ± 61.34 | 131.6 ± 55.3 | 0.828 |
| Total cholesterol (mg/dL) | 170.2 ± 43.26 | 182.89 ± 37.16 | 0.031 |
| LDL-C (mg/dL) | 106.53 ± 34.17 | 110.58 ± 31.01 | 0.507 |
| HDL-C (mg/dL) | 36.9 ± 9.31 | 45.97 ± 9.75 | < 0.001 |
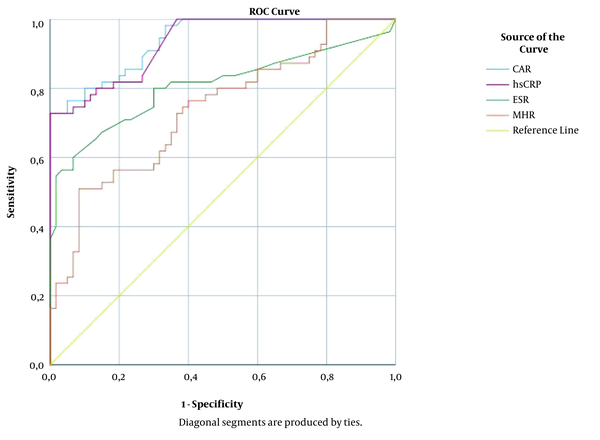
The correlations between inflammation-associated laboratory parameters in patients with brucellosis are shown in Table 2. The CAR levels were positively correlated with hsCRP, ESR, and MHR, while negatively correlated with LMR, MPV, and albumin. The MHR levels had a positive correlation with CAR, hsCRP, ESR, and NLR and negative correlations with LMR, MPV, and albumin. The ROC curve analysis for the significant variables was performed to evaluate their predictive performance for diagnosing brucellosis. The AUC values for CAR, hsCRP, ESR, and MHR were calculated as 0.939 (95% CI: 0.901 - 0.978), 0.932 (95% CI: 0.891 - 0.974), 0.807 (95% CI: 0.721 - 0.892), and 0.737 (95% CI: 0.647 - 0.828), respectively (Figure 1). The sensitivity, specificity, PPV, and NPV values are presented in Table 3 at the optimal cut-off values of 0.8 and 1.5 for CAR and the optimal cut-off values of 11 and 18.1 for MHR.
Correlation Between Inflammation-Associated Laboratory Parameters [r Value (P-Value)]
| Parameter | CAR | hsCRP | ESR | MHR | LMR |
|---|---|---|---|---|---|
| CAR | - | 0.996 (< 0.001) | 0.596 (< 0.001) | 0.476 (< 0.001) | -0.267 (0.004) |
| hsCRP | 0.996 (< 0.001) | - | 0.589 (< 0.001) | 0.472 (< 0.001) | -0.260 (0.005) |
| ESR | 0.596 (< 0.001) | 0.589 (< 0.001) | - | 0.187 (0.045) | -0.180 (0.054) |
| MHR | 0.476 (< 0.001) | 0.472 (< 0.001) | 0.187 (0.045) | - | -0.653 (< 0.001) |
| LMR | -0.267 (0.004) | -0.260 (0.005) | -0.180 (0.054) | -0.653 (< 0.001) | - |
| MPV | -0.342 (< 0.001) | -0.342 (< 0.001) | -0.231 (0.013) | -0.340 (< 0.001) | -0.211 (0.024) |
| Albumin | -0.410 (< 0.001) | -0.350 (< 0.001) | -0.284 (0.002) | -0.255 (0.006) | 0.193 (0.038) |
| NLR | 0.043 (0.648) | 0.048 (0.608) | 0.126 (0.178) | 0.246 (0.008) | -0.665 (< 0.001) |
| PLR | -0.015 (0.871) | -0.029 (0.757) | 0.197 (0.035) | -0.065 (0.491) | -0.414 (< 0.001) |
| RDW | 0.103 (0.273) | 0.089 (0.345) | 0.206 (0.027) | 0.060 (0.526) | -0.024 (0.801) |
Diagnostic Performance of CAR and MHR Cut-off Values in Predicting Brucellosis According to ROC Curve Analysis
| Cut-off Value | Sensitivity % | Specificity % | PPV % | NPV % |
|---|---|---|---|---|
| CAR ≥ 0.8 | 90.9 (80.4 - 96.1) | 71.7 (59.2 - 81.5) | 74.6 (63.1 - 83.5) | 89.6 (77.8 - 95.5) |
| CAR ≥ 1.5 | 72.7 (59.8 - 82.7) | 98.3 (91.1 - 99.7) | 97.6 (87.4 - 99.6) | 79.7 (69.2 - 87.3) |
| MHR ≥ 11 | 80 (67.6 - 88.4) | 51.7 (39.3 - 63.8) | 60.3 (48.8 - 70.7) | 73.8 (58.9 - 84.7) |
| MHR ≥ 18.1 | 50.9 (38.1 - 63.6) | 91.7 (81.9 - 96.4) | 84.8 (69.1 - 93.3) | 67.1 (56.3 - 76.3) |
ROC curve analysis of CAR, hsCRP, ESR, and MHR. AUC values for CAR, hsCRP, ESR, and MHR were calculated as 0.939, 0.932, 0.807, and 0.737, respectively.
5. Discussion
The clinical and laboratory diagnosis of brucellosis continues to be a challenge for clinicians because of its non-specific clinical manifestations, low isolation rates in blood cultures, and the possibility of false-positive or false-negative results in the serological methods. Nevertheless, an early and accurate diagnosis is essential to prevent the mismanagements and serious complications associated with brucellosis. Although numerous investigations have attempted to identify the predictive biomarkers for the diagnosis of brucellosis, there are yet no clinically valuable biomarkers that could be specific for brucellosis (7, 8, 11-14, 19-21). In the current study, besides well-recognized inflammatory markers, such as hsCRP and ESR, we investigated novel inflammatory markers which can reflect systemic inflammatory burden in patients with brucellosis.
It is known that positive acute phase reactants, CRP and ESR, are increased in brucellosis as a consequence of the inflammatory process. CRP is a sensitive but non-specific biomarker of systemic inflammation and is synthesized by the liver in response to proinflammatory cytokine signaling primarily mediated by neutrophils and monocytes (12, 13, 25). Serum CRP levels elevate within hours of inflammation and infection and can be easily determined by the high-sensitivity assays in routine laboratory practice. The hsCRP measurements detect even low serum concentrations of CRP, which are significantly associated with certain inflammatory and cardiovascular diseases. Many studies have reported the clinical utility of CRP and ESR in brucellosis (7, 8, 11-14, 26).
In a prospective case-control study in Iran, Akya et al. reported significantly higher CRP levels in patients with brucellosis compared to healthy individuals. The authors observed higher ESR values in patients with brucellosis than in healthy subjects. However, the difference between the groups was not statistically significant (8). In another study, Celik et al. revealed statistically significant increases in CRP and ESR in patients with brucellosis compared to the control group (12). A multicentric study carried out in Turkey demonstrated mild to moderate elevations in CRP and ESR in patients with genitourinary brucellosis (26). Similarly, in the present study, hsCRP and ESR values were significantly higher in patients than in control subjects (Table 1), and a positive correlation (r = 0.589, P ≤ 0.001) was found between hsCRP and ESR (Table 2). The findings of the current study and previous reports suggest that serum CRP level and ESR could be used as suitable markers of systemic inflammation in brucellosis.
Albumin is a negative acute-phase reactant produced in the liver, and its level in the serum decreases during inflammation. The combination of CRP and albumin into a single index (ie, CAR) has been proposed previously as a strong biomarker of systemic inflammation. CAR has been widely investigated in recent years as a diagnostic and prognostic marker in many clinical conditions, such as sepsis, inflammatory bowel disease, pancreatitis, and some malignancies (15-18). Yılmaz suggested that CAR can be used as a promising potential inflammatory marker for determining the prognosis in acute pancreatitis cases (16).
In another study, Kim et al. reported that CAR was superior to CRP in predicting long-term mortality in patients with severe sepsis or septic shock (18). However, to our knowledge, CAR has not yet been evaluated in patients with brucellosis. In the present study, it was found that patients with brucellosis had significantly higher CAR values compared to the control group (Table 1). Furthermore, positive correlations were noted between CAR, hsCRP, ESR, and MHR (Table 2), and it was observed that CAR had higher AUC values than hsCRP, ESR, and MHR (Figure 1). The cut-off values of ≥ 0.8 and ≥ 1.5 for CAR were shown to have diagnostic sensitivities of 90.9% and 72.7% and diagnostic specificities of 71.7% and 98.3%, respectively, in predicting brucellosis (Table 3).
The systemic inflammatory reaction leads to alterations in the blood levels and functions of neutrophils, lymphocytes, monocytes, and platelets. Neutrophils are among the first cells to react in the acute inflammatory response, and especially in bacterial infections, neutrophilia and relative lymphocytopenia are observed (7, 21, 27, 28). Platelets, in addition to their hemostatic functions, stimulate the release of proinflammatory cytokines and empower the migration of inflammatory cells, particularly monocytes and neutrophils, to the inflammatory sites (8, 20). Therefore, NLR, LMR, and PLR, which include neutrophil, lymphocyte, monocyte, and platelet counts, have been regarded as the indicators that effectively reflect systemic inflammatory status. This study found higher NLR and PLR and lower LMR values in patients with brucellosis than in healthy controls. However, only the difference in LMR values between the two groups was statistically significant (Table 1).
limited number of studies have investigated NLR, LMR, and PLR values in brucellosis, and discrepant results have been reported about the significance of these values (7, 8, 11, 14, 19-21). Although no statistically significant difference was determined in terms of NLR and PLR values in our study, Aktar et al. observed significantly increased NLR and PLR in children with Brucella arthritis (20). Bozdemir et al. reported significantly increased NLR and decreased MPV in childhood brucellosis. However, the authors found no significant difference in PLR values (7). In another study, reduced LMR and MPV values and increased NLR and PLR values were found to be significantly related to specific organ involvement in adult patients with brucellosis (21). Interestingly, in contrast to the literature, Olt et al. observed significantly lower NLR values in adult patients with brucellosis compared to the controls (19). As a result, the findings related to the hematological inflammatory parameters in patients with brucellosis were relatively different in various studies and raise questions regarding the role of these markers in the diagnosis of brucellosis. These inconsistent results may be due to the differences in sample size, age groups, or study population. In the light of these data, the results for the hematological inflammatory parameters show a diverse distribution in cases with brucellosis, and more detailed and comprehensive studies are required to elucidate the role of hematological inflammatory markers in brucellosis.
It has been recently demonstrated that increased MHR levels were related to the systemic inflammatory burden, and MHR might be used as a predictive factor of future cardiovascular disease (22, 23, 29-32). Circulating monocytes and macrophages in tissues play an essential role in initiating inflammation and activating the immune response and phagocytosis. However, the recruitment of monocytes aggravates oxidative stress and inflammation, particularly in the progression of atherosclerosis. The HDL, which has anti-inflammatory and antioxidant properties, suppresses monocyte activities and decreases the risk of cardiovascular disease by inhibiting new atherosclerotic plaque formations. As a result, combining the measurements of monocyte and HDL levels as MHR may reliably reflect the inflammatory process (22, 23, 29-32).
In an observational prospective cohort study conducted by Kanbay et al., it was noted that MHR could predict adverse clinical cardiovascular events in patients with chronic kidney disease (29). In another study, MHR was demonstrated to be an independent predictor of the severity of coronary artery disease and future cardiovascular events in patients with the acute coronary syndrome (30). There is no published report on the association between brucellosis and MHR. The present study indicated that MHR levels in patients with brucellosis were higher than those of the control subjects (Table 1). MHR values were positively correlated with CAR, hsCRP, ESR, and NLR and negatively correlated with LMR, MPV, and albumin (Table 2). The cut-off values of ≥ 11 and ≥ 18.1 for MHR were shown to have diagnostic sensitivities of 80% and 50.9% and diagnostic specificities of 51.7% and 91.7%, respectively, in predicting brucellosis (Table 3). As a practical and cost-effective marker, MHR could be used in clinical practice to assess the inflammatory status of brucellosis. Furthermore, MHR, together with hsCRP, which predicts cardiovascular risk, may provide a perspective for determining the patients with brucellosis at an elevated risk of cardiovascular disease.
The present research had some limitations that should be taken into account. First, it was a retrospective, single-center study with a relatively limited number of patients and controls. Second, we measured the levels of inflammatory markers only on admission, and we could not assess the changes in the levels of markers after the treatment. In spite of these limitations, we believe that our preliminary data can provide valuable insights for future research.
5.1. Conclusions
In conclusion, our findings demonstrated that increased CAR and MHR might reflect the systemic inflammatory burden in patients with brucellosis. These markers are significantly correlated with hsCRP and ESR and can be used as the markers of inflammation in diagnosing brucellosis. However, further studies with a larger sample size are required to support our findings and suggestions.
References
-
1.
Franco MP, Mulder M, Gilman RH, Smits HL. Human brucellosis. Lancet Infect Dis. 2007;7(12):775-86. https://doi.org/10.1016/s1473-3099(07)70286-4.
-
2.
Rubach MP, Halliday JE, Cleaveland S, Crump JA. Brucellosis in low-income and middle-income countries. Curr Opin Infect Dis. 2013;26(5):404-12. [PubMed ID: 23963260]. [PubMed Central ID: PMC3888775]. https://doi.org/10.1097/QCO.0b013e3283638104.
-
3.
Franc KA, Krecek RC, Hasler BN, Arenas-Gamboa AM. Brucellosis remains a neglected disease in the developing world: a call for interdisciplinary action. BMC Public Health. 2018;18(1):125. [PubMed ID: 29325516]. [PubMed Central ID: PMC5765637]. https://doi.org/10.1186/s12889-017-5016-y.
-
4.
Pappas G, Akritidis N, Bosilkovski M, Tsianos E. Brucellosis. N Engl J Med. 2005;352(22):2325-36. [PubMed ID: 15930423]. https://doi.org/10.1056/NEJMra050570.
-
5.
Doganay M, Aygen B. Human brucellosis: an overview. Int J Infect Dis. 2003;7(3):173-82. https://doi.org/10.1016/s1201-9712(03)90049-x.
-
6.
Al Dahouk S, Nockler K. Implications of laboratory diagnosis on brucellosis therapy. Expert Rev Anti Infect Ther. 2011;9(7):833-45. [PubMed ID: 21810055]. https://doi.org/10.1586/eri.11.55.
-
7.
Bozdemir SE, Altintop YA, Uytun S, Aslaner H, Torun YA. Diagnostic role of mean platelet volume and neutrophil to lymphocyte ratio in childhood brucellosis. Korean J Intern Med. 2017;32(6):1075-81. [PubMed ID: 27951626]. [PubMed Central ID: PMC5668393]. https://doi.org/10.3904/kjim.2016.092.
-
8.
Akya A, Bozorgomid A, Ghadiri K, Ahmadi M, Elahi A, Mozafari H, et al. Usefulness of blood parameters for preliminary diagnosis of brucellosis. J Blood Med. 2020;11:107-13. [PubMed ID: 32280292]. [PubMed Central ID: PMC7125307]. https://doi.org/10.2147/JBM.S245513.
-
9.
Yagupsky P, Morata P, Colmenero JD. Laboratory diagnosis of human brucellosis. Clin Microbiol Rev. 2019;33(1). [PubMed ID: 31722888]. [PubMed Central ID: PMC6860005]. https://doi.org/10.1128/CMR.00073-19.
-
10.
Koroglu M, Aydemir OA, Demiray T, Erkorkmaz U, Ozbek A, Altindis M. Comparative evaluation of the Brucella Coombs gel test in laboratory diagnosis of human brucellosis. Biotechnol Biotechnol Equip. 2016;30(5):970-5. https://doi.org/10.1080/13102818.2016.1190945.
-
11.
Balin SO, Tartar AS, Akbulut A. The predictive role of haematological parameters in the diagnosis of osteoarticular brucellosis. Afr Health Sci. 2018;18(4):988-94. [PubMed ID: 30766564]. [PubMed Central ID: PMC6354860]. https://doi.org/10.4314/ahs.v18i4.19.
-
12.
Celik VK, Sari I, Bakir S, Engin A, Bakir D, Sari M, et al. Erythrocyte sedimentation rate, serum amyloid A and C-reactive protein levels in patients with acute brucellosis. Pak J Med Sci. 2011;27(4):823-6.
-
13.
Liu J, Zhao X. Clinical features and serum profile of inflammatory biomarkers in patients with brucellosis. J Infect Dev Ctries. 2017;11(11):840-6. https://doi.org/10.3855/jidc.8872.
-
14.
Togan T, Narci H, Turan H, Ciftci O, Kursun E, Arslan H. The impact of acute brucellosis on mean platelet volume and red blood cell distribution. Jundishapur J Microbiol. 2015;8(2). e20039. [PubMed ID: 25825650]. [PubMed Central ID: PMC4376969]. https://doi.org/10.5812/jjm.20039.
-
15.
Oh TK, Choi YR, Cho JY, Yoon YS, Han HS, Park IS, et al. The high-sensitivity c-reactive protein/albumin ratio predicts long-term oncologic outcomes after curative resection for hepatocellular carcinoma. J Clin Med. 2018;7(6). [PubMed ID: 29880755]. [PubMed Central ID: PMC6024983]. https://doi.org/10.3390/jcm7060139.
-
16.
Yılmaz EM. Significance of red blood cell distribution width and CRP/albumin levels in predicting prognosis of acute pancreatitis. Turkish J Trauma Emerg Surg. 2018;24(6):528-31. https://doi.org/10.5505/tjtes.2018.98583.
-
17.
Park JE, Chung KS, Song JH, Kim SY, Kim EY, Jung JY, et al. The C-reactive protein/albumin ratio as a predictor of mortality in critically ill patients. J Clin Med. 2018;7(10). [PubMed ID: 30297655]. [PubMed Central ID: PMC6210319]. https://doi.org/10.3390/jcm7100333.
-
18.
Kim MH, Ahn JY, Song JE, Choi H, Ann HW, Kim JK, et al. The C-reactive protein/albumin ratio as an independent predictor of mortality in patients with severe sepsis or septic shock treated with early goal-directed therapy. PLoS One. 2015;10(7). e0132109. [PubMed ID: 26158725]. [PubMed Central ID: PMC4497596]. https://doi.org/10.1371/journal.pone.0132109.
-
19.
Olt S, Ergenc H, Acikgoz SB. Predictive contribution of neutrophil/lymphocyte ratio in diagnosis of brucellosis. Biomed Res Int. 2015;2015:210502. [PubMed ID: 25722970]. [PubMed Central ID: PMC4333181]. https://doi.org/10.1155/2015/210502.
-
20.
Aktar F, Tekin R, Bektas MS, Gunes A, Kosker M, Ertugrul S, et al. Diagnostic role of inflammatory markers in pediatric Brucella arthritis. Ital J Pediatr. 2016;42:3. [PubMed ID: 26753565]. [PubMed Central ID: PMC4709903]. https://doi.org/10.1186/s13052-016-0211-5.
-
21.
Sen P, Demirdal T, Nemli SA. Predictive inflammation markers in brucellosis. Arch Iran Med. 2019;22(11):640-5.
-
22.
Ganjali S, Gotto AJ, Ruscica M, Atkin SL, Butler AE, Banach M, et al. Monocyte-to-HDL-cholesterol ratio as a prognostic marker in cardiovascular diseases. J Cell Physiol. 2018;233(12):9237-46. [PubMed ID: 30076716]. https://doi.org/10.1002/jcp.27028.
-
23.
Sirin MC, Korkmaz S, Erturan I, Filiz B, Aridogan BC, Cetin ES, et al. Evaluation of monocyte to HDL cholesterol ratio and other inflammatory markers in patients with psoriasis. An Bras Dermatol. 2020;95(5):575-82. [PubMed ID: 32711928]. [PubMed Central ID: PMC7562997]. https://doi.org/10.1016/j.abd.2020.02.008.
-
24.
CDC. Brucellosis reference guide: Exposures, testing and prevention. US Department of Health and Human Services, CDC Atlanta (GA); 2017.
-
25.
Sproston NR, Ashworth JJ. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front Immunol. 2018;9:754. [PubMed ID: 29706967]. [PubMed Central ID: PMC5908901]. https://doi.org/10.3389/fimmu.2018.00754.
-
26.
Erdem H, Elaldi N, Ak O, Gulsun S, Tekin R, Ulug M, et al. Genitourinary brucellosis: results of a multicentric study. Clin Microbiol Infect. 2014;20(11):O847-53. [PubMed ID: 24831227]. https://doi.org/10.1111/1469-0691.12680.
-
27.
Skendros P, Boura P. Immunity to brucellosis. Rev Sci Tech. 2013;32(1):137-47. [PubMed ID: 23837372]. https://doi.org/10.20506/rst.32.1.2190.
-
28.
Zahorec R. Ratio of neutrophil to lymphocyte counts--rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy. 2001;102(1):5-14. [PubMed ID: 11723675].
-
29.
Kanbay M, Solak Y, Unal HU, Kurt YG, Gok M, Cetinkaya H, et al. Monocyte count/HDL cholesterol ratio and cardiovascular events in patients with chronic kidney disease. Int Urol Nephrol. 2014;46(8):1619-25. [PubMed ID: 24853998]. https://doi.org/10.1007/s11255-014-0730-1.
-
30.
Cetin MS, Ozcan Cetin EH, Kalender E, Aydin S, Topaloglu S, Kisacik HL, et al. Monocyte to HDL cholesterol ratio predicts coronary artery disease severity and future major cardiovascular adverse events in acute coronary syndrome. Heart Lung Circ. 2016;25(11):1077-86. [PubMed ID: 27118231]. https://doi.org/10.1016/j.hlc.2016.02.023.
-
31.
Enhos A, Cosansu K, Huyut MA, Turna F, Karacop E, Bakshaliyev N, et al. Assessment of the Relationship between Monocyte to High-Density Lipoprotein Ratio and Myocardial Bridge. Arq Bras Cardiol. 2019;112(1):12-7. [PubMed ID: 30570069]. [PubMed Central ID: PMC6317631]. https://doi.org/10.5935/abc.20180253.
-
32.
Ekizler FA, Cay S. A novel marker of persistent left ventricular systolic dysfunction in patients with peripartum cardiomyopathy: monocyte count- to- HDL cholesterol ratio. BMC Cardiovasc Disord. 2019;19(1):114. [PubMed ID: 31092205]. [PubMed Central ID: PMC6521346]. https://doi.org/10.1186/s12872-019-1100-9.