1. Introduction
Brucellosis is a zoonotic bacterial disease caused by Brucella spp., which can involve multiple organs and tissues. Brucellae are small, facultative intracellular coccobacilli that infect humans either by direct contact with infected animals or by ingesting unpasteurized dairy products or milk from infected animals. The most common symptoms of human brucellosis are fatigue, fever, back, and low-back pain, decreased appetite, myalgias, arthralgias, sweat, and weight loss. The most common complications of brucellosis are osteoarticular involvement comprising osteomyelitis, peripheral arthritis, tenosynovitis, sacroiliitis, bursitis, and spondylodiscitis.
Spondylodiscitis is a severe complication of brucellosis described as an infection of vertebral bodies, intervertebral disc space, or paraspinal soft tissues. It can cause mortality and morbidity and warrants diagnostic delay and inadequate treatment (1). The use of adequate antibiotics is primarily successful for treating brucellar spondylodiscitis in the early stages of disease; however, the diagnosis and management of the disease are complex and challenging. A delay in diagnosis could occur because of abscess formation in adjacent tissues, disabling neurological deficits, and the insidious onset of symptoms. We report herein the isolation of Brucella melitensis from lumbar vertebrae in a case of brucellar spondylodiscitis in which the only symptom was chronic low-back pain without any positive responses in serological tests to detect Brucella agglutinating antibodies.
2. Case Presentation
A 65-year-old male was presented to Alborz hospital (western Iran) due to a longstanding history of low-back pain, restricted lumbar movements, headache, poor appetite, and fatigue for the past nine months. He was a security officer with a history of the regular consumption of raw cow milk and milk products for a long time in his family. There was no contact history with cows, sheep, goats, or pets. The patient had no fever, and his vital signs were stable on physical examination during the case report. The patient complained of tenderness points on his low back and had pain when walking or sitting for a long time despite conventional treatment by his primary care physician for the past nine months. He also suffered from spinal osteoarthritis as an underlying condition. Before admission, the patient's medication history showed a white cell count of 6.7 × 103/µL with an erythrocyte sedimentation rate of 27 mm/h, 52.7% neutrophils, and negative C reactive protein. Other laboratory results for complete blood count, erythrocyte sedimentation rate, rheumatoid factor, urea, aspartate aminotransferase, creatine, and alanine transaminase were normal, except for red cell distribution width (RDW, 15%), red blood cell (RBC, 4.34 × 106/µL), and hemoglobin (HGB, 13.3 g/dL).
The Rose Bengal test (RBT), Serum Agglutination test (SAT), 2-Mercaptoethanol (2-ME), iELISA (IgG), and real-time PCR for the detection of specific Brucella DNA (B. melitensis, B. suis, B. abortus, B. ovis, and B. canis) in the blood were negative. Moreover, the culture of blood for possible Brucella spp. isolation was negative. The first lumbosacral magnetic resonance imaging (MRI) without intravenous contrast showed minimal disc bulge at L3 - L4 and L4 - L5 without caudal or foraminal narrowing. In addition, mass impression upon the thecal sac at L4 - L5 was notable with a relevant herniated disc. Right lateral recess and canal stenosis occurred at L4 - L5. Visualized cord and conus medullaris showed the normal shape, and signal intensity and the lumbar canal showed adequate dimension. However, no evidence of intramedullary lesion abnormality was seen, other discs appeared normal, and herniation was not seen. Based on the MRI results, the patient was treated with nonsteroidal anti-inflammatory drugs and myorelaxants for lumbar disc herniation, but his symptoms did not resolve.
Three months after the first MRI report and throughout the case report, the results of the second MRI showed right lateral recess and canal stenosis at L4 - L5 with narrowing the thecal sac at the disc space. Endplate abnormalities at L4 - L5 with associated epidural soft tissue and epidural abscess at L4 also were reported. Moreover, extensive high signal abnormalities in paraspinal tissues at L3, L4, L5, S1, S2, and S3 levels were notable. Furthermore, fluid collection at the subcutaneous fat-fascia interface along the posterior paraspinal lumbosacral region may have resulted from a shearing injury known as Morel-Lavallee lesion. Visualized cord and conus medullaris showed the normal shape and signal intensity. Destruction or fracture was not seen in vertebral bodies. Other discs appeared normal, and herniation was not seen. Brain MRI also showed lesion clusters more pronounced in the corona radiate and periventricular white matter. Moreover, numerous patchy punctate, radial/linear areas of hyperintensity around small medullary veins revealed gliosis limited to old lacunes.
The signal intensity of gray matter was normal, and no evidence of extra-axial or intra-axial mass lesion was seen. Sellar, suprasellar, and parasellar areas showed normal shape, and no specific pathology was seen in the skull base. The pons, medulla oblongata, and visualized region of the cervical cord and petromastoid structure showed normal patterns. The laboratory values were normal for white blood cell count and blood biochemistry profile. However, hemoglobin and RBC were lower than the reference value, and RDW exhibited higher values. No Brucella species were isolated from repeat blood cultures. Therefore, the disc tissue and body vertebrate were sampled according to the standard operating practice through the lumbar microdiscectomy for possible isolation of bacteria. The patient was diagnosed with brucellar spondylodiscitis through the positive culture for B. melitensis. For this purpose, the tissue of disc and body vertebrate fragment were homogenized in 3 mL of Brucella broth medium (Himedia, India) and inoculated on Brucella selective supplement medium containing 5% inactivated horse serum and vancomycin (10 mg), cycloheximide (50 mg), nalidixic acid (2.5 mg), polymyxin B (2,500 IU), bacitracin (12,500 IU), and nystatin (50,000 IU) (Oxoid, UK).
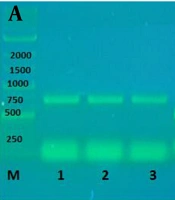
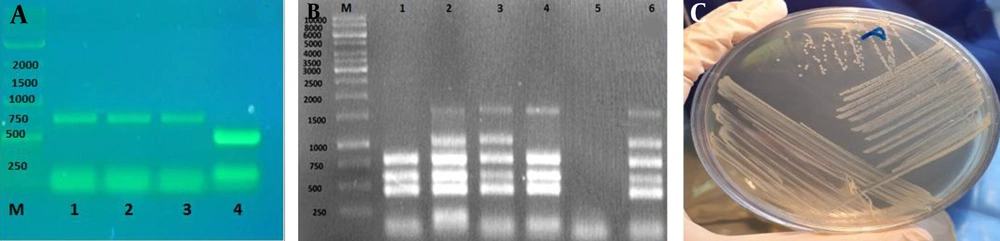
The inoculated plates were kept at 37°C under 10% CO2 for 10 days. Molecular and conventional biotyping analyses identified typical isolated Brucella from the disc tissue and vertebrate body fragment. Common specific phenotypic features of Brucella spp. such as Gram-negative bacteria with smooth and translucent honey color surfaces were observed in the isolated bacteria. The Brucella isolate was identified as B. melitensis biovar 1 using conventional biotyping methods, i.e., H2S production, CO2 requirement, growth in the presence of basic fuchsin and thionin dyes, sensitivity to lysis using the Tbilisi and Izatnagar phage, and agglutination test with A and M monospecific antisera. Then, the isolate was identified as wild type B. melitensis using AMOS and Bruce-ladder PCR. The AMOS PCR results produced DNA products of 731 bp sizes for B. melitensis biovar 1. This result was further confirmed by the Bruce-ladder PCR, resulting in PCR products of 1682, 794, 587, 450, 152, and 1,071 bp sizes (Figure 1A - C). The patient was subjected to surgical debridement with epidural abscess drainage and antibiotic therapy with oral doxycycline 100 mg/12 h plus oral rifampin 300 mg/12 h for three months and intramuscular streptomycin 1 g daily for the first two weeks. A six-month follow-up showed that the patient’s general condition significantly improved and low-back pain, night sweats, and weakness reduced following the treatment.
A, PCR amplified AMOS-PCR products on agarose gel electrophoresis (1%). Lane M indicated a 1000 bp DNA marker. Lane 1 represents Brucella melitensis isolated from lumbar vertebra culture; Lane 2 shows B. melitensis wild type; Lane 3 shows B. melitensis 16 M (reference bacteria); Lane 4 shows B. abortus 544 (reference bacteria); B, Bruce-ladder PCR products on agarose gel electrophoresis (1%). Lane M shows a 1000 bp DNA marker. Lane 1 shows B. abortus strain RB51; Lane 2 shows B. melitensis strain Rev1; Lane 3 shows B. melitensis 16M; Lane 4 shows B. abortus 544; Lane 5 is negative control; Lane 6 represents isolated Brucella from disc culture; C, Colony of B. melitensis on Brucella agar.
3. Discussion
Brucellosis is a zoonotic infection and a common public health concern, especially in the Middle East region, including Iran. In endemic regions, musculoskeletal complications of brucellosis like peripheral arthritis, sacroiliitis, and peripheral arthritis are frequently reported, but other complications are rare. Our finding showed the isolation and molecular identification of B. melitensis from inherited disc and body vertebrate infection in a male patient with brucellar spondylodiscitis, suggesting the critical role of Brucella species in the induction of this infection. However, previous investigations showed the isolation and classical identification of B. melitensis from an epidural abscess in a female patient with brucellar spondylodiscitis (2). Our finding was significant since this case revealed negative serological, molecular, and blood culture tests despite the isolation of B. melitensis from lumbar vertebrae, suggesting that focal complications may show no specific Brucella antibody titers in infected cases.
Similar to our case, two other publications of brucellar spondylodiscitis also reported positive Brucella spp. culture and typical radiological modifications despite negative serological tests (2, 3). A study showed an uncommon case of brucellar spondylodiscitis involving several paravertebral and vertebrae abscesses localized in the spinal muscle (4) and another one isolated Brucella spp. in the disco-vertebral biopsy with the positive Brucella serology (5). Therefore, negative serology tests could not exclude the focal form of brucellosis. It has been revealed that 6 - 12% of human brucellosis cases have spinal involvement, inducing disabling and debilitating complications. Moreover, epidural, paravertebral, psoas, and prevertebral abscesses are infrequent manifestations of spinal brucellosis that represent non-specific signs such as lower limb weakness, spinal tenderness, fever, sensory loss or sphincter loss due to subsequent spinal stenosis, and spinal cord compression in case of delayed diagnosis. Our case was complicated with the epidural abscess behind L4, revealing a rarely encountered clinical case of B. melitensis infection. A spinal epidural abscess can lead to permanent complications and even death if untreated.
The incidence of spinal epidural abscess is rare and associated with spondylitis, documented in less than 1.5% of neurological complications of brucellosis. Several antibiotic combinations such as rifampicin, doxycycline, aminoglycoside, ciprofloxacin, and sulphamethoxazole plus trimethoprim are suggested for brucellar spondylodiscitis treatment. In our case, a combination of three antibiotics for three months and surgical debridement with epidural abscess drainage significantly improved the symptoms. It has been reported that the aminoglycoside-containing regimens show better outcomes in brucellar vertebral osteomyelitis than rifampin-containing regimens. Our case had a history of ingesting raw dairy products, which is the most common way to acquire brucellosis.
Finally, a multi-disciplinary approach involving different diagnostic methods like MRI, culture, serological, and PCR tests and accurate history-taking is demanded in the early diagnosis and management of complicated spinal brucellosis. A history of animal contact and consumption of dairy products is a diagnostic guide for human brucellosis in endemic regions such as Iran. Therefore, physicians should remember brucellar spondylodiscitis among differential diagnoses in patients with chronic back pain and perform an MRI for patients with such a condition. Furthermore, a culture or biopsy from infected tissue is recommended as an accurate diagnostic test to confirm the diagnosis. Any delay in treatment could lead to lifelong neurological deficits or death. Surgery should be recommended if there is a poor response to antibiotic treatment. Also, it should be highlighted that the early diagnosis of brucellar spondylodiscitis requires expertise and laboratory services and remains very difficult. A limitation of this case report was the lack of an MRI test for the patient's clinical progress after antibiotic therapy. This could be attributed to the COVID-19 pandemic restrictions and the improvement of his low-back pain.