Abstract
Introduction:
Babesiosis is caused by apicomplexa parasites of the genus Babesia. Humans are commonly infected by Babesia through tick bites. There is limited information available about Babesia infection of humans in China. The aim of this study was to isolate the pathogen from a patient with severe parasitemia.Case Presentation:
Blood samples were observed by transmission electron microscopy (TEM) and indirect fluorescent antibody (IFA), and red blood cells of bone marrow and blood smears were examined by a microscope. The patient was infected by Babesia and cured after a combined treatment.Conclusions:
Babesia infection was detected in an individual from China.Keywords
Babesiosis Infection indirect fluorescent antibody TEM transmission electron microscopy
1. Introduction
Babesiosis is a worldwide tick borne protozoan disease that infects humans and animals. Babesia is the intra-erythrocyte infectious agent of babesiosis. Humans are commonly infected by Babesia through tick bites (1). Babesia infected tick introduce sporozoites to the host and multiply in the blood as a clinical manifestation (2). Human to human transmission occurs through blood transfusions (3). Babesia is highly prevalent in malaria endemic countries, such as Africa, Asia, and South America (4), but rarely reported in Southeast China. In April 2010, a 46-year-old woman residing in Yunnan was hospitalized due to diarrhea, fever (37.3°C), chills, myalgia, fatigue, high leucocytes (18.40 × 109/L) and polymorphonuclear neutrophils (88.2%). The patient was reportedly bitten by ticks while traveling in Xishuangbanna where malaria was endemic.
2. Case Presentation
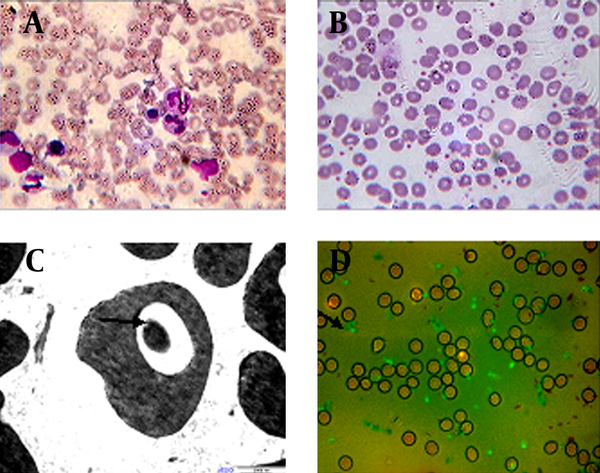
The study was approved by the patient and the Ethics Committee of Kunming General Hospital of Chengdu Military Region. Severe parasitemia was observed by microscopic examination of the erythrocytes in the bone marrow fluid with Wright stain (Figure 1 A, Nikon, E200). The morphology of Babesia was subsequently assessed by thin blood smears stained with Giemsa (Figure 1 B). For further identification of Babesia infection, blood samples were fixed, dehydrated, thin sectioned, and stained for transmission electron microscopy (TEM, Hitachi, H-9500, Japan) according to a previous study (5). Vacuolization of the host cytoplasm was observed by TEM (Figure 1 C, black arrow). To distinguish between Plasmodium falciparum and Babesia infection, indirect fluorescent antibody test (IFA) was performed using the Babesia microti IgG IFA kit (BMG-120, Gentaur, Belgium, at 1:256 dilutions) as the antigen to detect antibodies in the blood smears (Figure 1 D, black arrow). The detection of Babesia specific antibody by IFA is the most prominent tool for diagnosis, with specificity of 100% in patients with other tick borne diseases or those not exposed to the parasite (6).
Babesia sp Examined by the Microscope
3. Discussion
The patient in the present study was cured by a combined treatment of artemether, azithromycin, and clindamucin through intramuscular injection and oral intake of atovaquone. Babesia is commonly reported to infect human beings with splenectomy (1, 7) or anemia (8). No lesions in the spleen or liver of the patient were observed by the CT scan. No indication of anemia was found. These results imply that immunodeficient patients, as well as those with low resistance, can be vulnerable to Babesia infection.
Acknowledgements
References
-
1.
Garnham PC, Donnelly J, Hoogstraal H, Kennedy CC, Walton GA. Human babesiosis in Ireland: further observations and the medical significance of this infection. Br Med J. 1969;4(5686):768-70. [PubMed ID: 4902496].
-
2.
Ueti MW, Palmer GH, Kappmeyer LS, Scoles GA, Knowles DP. Expression of equi merozoite antigen 2 during development of Babesia equi in the midgut and salivary gland of the vector tick Boophilus microplus. J Clin Microbiol. 2003;41(12):5803-9. [PubMed ID: 14662988].
-
3.
Herwaldt BL, Neitzel DF, Gorlin JB, Jensen KA, Perry EH, Peglow WR, et al. Transmission of Babesia microti in Minnesota through four blood donations from the same donor over a 6-month period. Transfusion. 2002;42(9):1154-8. [PubMed ID: 12430672].
-
4.
Vannier E, Gewurz BE, Krause PJ. Human babesiosis. Infect Dis Clin North Am. 2008;22(3):469-88. viii-ix. [PubMed ID: 18755385]. https://doi.org/10.1016/j.idc.2008.03.010.
-
5.
Braga W, Venasco J, Willard L, Moro MH. Ultrastructure of Babesia WA1 (Apicomplexa: Piroplasma) during infection of erythrocytes in a hamster model. J Parasitol. 2006;92(5):1104-7. [PubMed ID: 17152960]. https://doi.org/10.1645/GE-712R.1.
-
6.
Sambri V, Marangoni A, Storni E, Cavrini F, Moroni A, Sparacino M, et al. [Tick borne zoonosis: selected clinical and diagnostic aspects]. Parassitologia. 2004;46(1-2):109-13. [PubMed ID: 15305697].
-
7.
Wormser GP, Lombardo G, Silverblatt F, El Khoury MY, Prasad A, Yelon JA, et al. Babesiosis as a cause of fever in patients undergoing a splenectomy. Am Surg. 2011;77(3):345-7. [PubMed ID: 21375849].
-
8.
Qi C, Zhou D, Liu J, Cheng Z, Zhang L, Wang L, et al. Detection of Babesia divergens using molecular methods in anemic patients in Shandong Province, China. Parasitol Res. 2011;109(1):241-5. [PubMed ID: 21503639]. https://doi.org/10.1007/s00436-011-2382-8.