Abstract
Introduction:
Mangled extremity injuries in civilian settings are challenging conditions for the accident and emergency units of low-resource settings where salvage therapies may not be feasible or affordable for the patients.Case Report:
We have described a successful case of initial conservative limb salvage management for a mangled distal left lower limb in a four-year-old male who sustained the injury when a vehicle ran over his extremity as he played by the road. The treatment approach was in contrast to the radical completion of amputation with its attendant revisions, which are associated with similar injuries with the mangled extremity severity scores of ≥ 7.Conclusions:
The benefits and challenges of the limb salvage intervention were discussed based on the literature in this regard, and a recommendation was proposed while considering an initial conservative limb salvage approach in well-resuscitated children presenting early with a mangled extremity injury.Keywords
1. Introduction
Mangled extremities and crush injuries in civilian settings are often accidental (1), and children represent a vulnerable population in this regard. Ankle fractures constitute 5% of all pediatric fractures (2). However, the initial evaluation of the crush injury to determine the severity and predict the consequences may not be straightforward.
Scoring systems such as the mangled extremity severity score (MESS) (3) are commonly used in our institution to assess the severity of such injuries, while the decision on the appropriate interventions and their long-term outcomes may require more factors to be considered in addition to the MESS (4). Some of the factors that are often overlooked are the acceptability of the intended amputations to the patients (1) and the accessibility and quality of prosthetic and rehabilitation services after the amputation (5).
Regardless of the severity score, a less radical initial approach to mangled extremity injuries in children involves debridement and external fixation when indicated, which could offer viable alternatives to a completion amputation (6, 7). It is possible that the amputation and disability rates in such injuries reduce if training and basic orthopedic resources are available to general surgeons and medical officers in Ghanaian district hospitals.
In the present study, we have described a successful case of initial limb salvage approach adopted in the management of a four-year-old male with a mangled extremity despite the MESS of eight.
2. Case Presentation
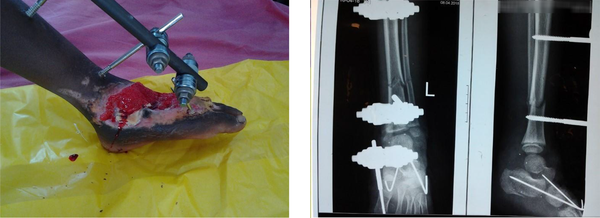
A four-year-old male was rushed to our hospital within an hour after his left leg and foot had been run over by a moving vehicle while he was playing by the road. The patient sustained an open left ankle injury (Figure 1). The left distal leg and foot were painfully deformed and had moderate bleeding and exposed bones.
No loss of consciousness was observed, and the examination of the other organ systems was unremarkable. The patient had a Glasgow coma score of 15/15 upon admission. The primary examination revealed a class I hemorrhagic shock (BP: 80/50 mmHg, pulse rate: 115 bpm), which was managed with crystalloid boluses, followed by maintenance fluids. Broad-spectrum antibiotics, analgesics, and anti-tetanus prophylaxis were also administered. No evidence of head injury and thoracic/abdominopelvic trauma was present, and eFAST was negative.
Status localis showed a mangled distal left leg, ankle, and foot with complete dorsal skin avulsion (Figure 1). In addition, there was an open disrupted left ankle joint with the ligaments in disarray. The articular cartilage was also avulsed with the separation of the tarsal complex. Avulsion fractures of the uppermost tarsals were observed. The dorsalis pedis was involved in the injury, while the posterior tibial artery could not be objectively assessed. The popliteal artery pulsation was intact. The injury corresponded to a Gustilo Grade IIIB injury. Distal sensorimotor assessment could not be performed due to the nature of the injury. The toes distal to the injury were relatively cold to touch with a capillary refill time of more than three seconds, while the dangling foot was not pale or darkened in appearance.
The calculated MESS was eight (tissue injury: 4, limb ischemia: 2, shock group: 2, age: 0). Prompt resuscitation and blood examination were performed. After obtaining informed consent, the patient was transferred to the operating room for wound debridement and an attempt at limb salvage. Intraoperative X-rays revealed additional transverse fractures of the distal tibia, fibula, and the calcaneus (Figure 2). A significant portion of the extensor tendons were completely avulsed.
After adequate wound debridement, an ankle-bridging external fixation was mounted during image-guided surgery (Figure 2). Two Kirschner pins were also inserted into the AP direction to stabilize the tarsal complex (Figure 2). Postoperatively, wound dressing was carried out daily for five days until a significant reduction was observed in drainage with the appearance of healthy granulation tissues. Wound dressing continued afterwards at scheduled 3-4-day intervals until the wound became completely granulated (Figure 2). Split-thickness skin grafting was successfully carried out on postoperative day (POD) 33 by which time the transverse distal tibia/fibula fracture had united.
Ankle Injury upon Admission

Ankle Injury on POD 33
3. Discussion
Crush injuries of the lower limb among children playing along transportation routes are an important cause of extremity amputation in this population (5-7). The subsequent use of prostheses over the period of growth into adulthood is reported to be a source of significant healthcare expenditure (8). Such healthcare costs are a burden on the amputees in Ghana, most of whom are ultimately resigned to using crutches or a wheelchair, which significantly decreases the quality of life and socioeconomic potential.
The case described in our study represents a less common scenario in a low-resource setting where a potential completion amputation was averted in a mangled extremity injury despite the non-reassuring MESS of eight (3). The arguments for completing the amputation included the securing of hemostasis in a shocked patient, conducting a shorter procedure, and eliminating the risk of crush syndrome or a reperfusion injury associated with limb salvage (9). The unavailability of vascular reconstruction (10) for such extremity injuries in most Ghanaian centers casts doubt about the future viability of a replanted mangled extremity, which was a valid consideration in our patient since the blood supply in the ankle area had less elaborate collaterals compared to the other large joints. The damage to the dorsalis pedis and the uncertain preservation of the posterior tibial artery further diminished the chances of extremity viability.
Despite the reduction of distal perfusion, the MESS of eight could be overlooked, and limb salvage could be attempted. In a study, several patients with ischemia on the initial examination had successful limb salvage (11). The MESS has come under scrutiny, having its sensitivity questioned due to the rather subjective nature of its constituent parameters (4).
The case described here could point to the faster healing and tissue regeneration potential of children (12) as a key advantage that should be harnessed to encourage more efforts at limb salvage for major and minor extremity crush injuries in this patient population. This is further supported by the lower incidence of persistent talus osteonecrosis in children aged less than 12 years even after operative management for open ankle injuries (13). Therefore, the MESS should remain a guiding tool but not used as an independent decision-making resource since its sensitivity in the presented case was quite low. Over-reliance on the MESS for decision-making could lead to performing unneeded amputations. Care for extremity crush injuries (particularly in children) should be based on an individualized approach, which considers relevant factors to the patients’ age, hemodynamic status upon referral, setting-specific resource availability, and the acceptance of the intended procedure.
In all cases of extremity crush injuries involving children who are referred early to the hospital, it is tempting to suggest the justification of an initial limb salvage approach when not contraindicated despite non-reassuring clinical limb viability scores. This should be accompanied by adequate supportive therapy and the regular reassessment of the wound and extremity (5), and a decision regarding the need for an amputation may be made thereafter (1). Although such an approach may not be very appropriate, it could be practical in the cases where crush syndrome has already set in or when clear risks are speculated for reperfusion injury following the restoration of circulation. In the long run, the patient is expected to require physical therapy and more surgeries to enhance the limb function (14, 15). Anticipated problems include joint stiffness (2), angulation deformities, limb-length discrepancy (11), and psychosocial disorders (15), all of which are issues depicting the benefit of a multidisciplinary approach to the management of these patients (5). On the other hand, addressing patients’ expectations of treatment outcomes should be expertly handled in severe injuries (14). Since the timeliness and effectiveness of the initial intervention is crucial, healthcare stakeholders in low-resource settings such as Ghana should seriously consider equipping district hospitals with the capacity to salvage mangled limbs, which could have long-term benefits in reducing the overall healthcare expenditure in rehabilitation and lost man-hours.
3.1. Conclusions
We presented the case of an initial conservative limb salvage procedure in a mangled lower extremity injury in a four-year-old child. Improved outcomes are hoped to be achieved by instituting prompt hemodynamic and operative interventions. In well-resuscitated children referred early, brief limb salvage procedures may be the best initial step with any decision on amputation made at the subsequent reassessments. Although the MESS is considered clinically useful in low-resource settings, it may not be an optimal indicator of extremity viability distal to the level of injury. Therefore, resources must be made available in lower-level hospitals to facilitate prompt limb salvage interventions before referral to higher trauma centers.
Acknowledgements
References
-
1.
Clasper J, Ramasamy A. Traumatic amputations. Br J Pain. 2013;7(2):67-73. [PubMed ID: 26516502]. [PubMed Central ID: PMC4590129]. https://doi.org/10.1177/2049463713487324.
-
2.
Olgun ZD, Maestre S. Management of pediatric ankle fractures. Curr Rev Musculoskelet Med. 2018;11(3):475-84. [PubMed ID: 29987644]. [PubMed Central ID: PMC6105478]. https://doi.org/10.1007/s12178-018-9510-3.
-
3.
Krettek C, Lerner A, Giannoudis P, Willy C, Muller CW. [Limb salvage and amputation after trauma: Decision criteria and management algorithm]. Unfallchirurg. 2016;119(5):358-73. German. [PubMed ID: 27178157]. https://doi.org/10.1007/s00113-016-0181-5.
-
4.
Prasarn ML, Kloen P, Helfet DL. Mangled extremity: Management in isolated extremity injuries and in polytrauma. The poly-traumatized patient with fractures. Berlin, Heidelberg: Springer; 2016. p. 169-86.
-
5.
Tintle SM, Keeling JJ, Shawen SB, Forsberg JA, Potter BK. Traumatic and trauma-related amputations: part I: general principles and lower-extremity amputations. J Bone Joint Surg Am. 2010;92(17):2852-68. [PubMed ID: 21123616]. https://doi.org/10.2106/JBJS.J.00257.
-
6.
Blair JA, Eisenstein ED, Pierrie SN, Gordon W, Owens JG, Hsu JR. Lower extremity limb salvage: Lessons learned from 14 years at war. J Orthop Trauma. 2016;30 Suppl 3:S11-5. [PubMed ID: 27661420]. https://doi.org/10.1097/BOT.0000000000000669.
-
7.
Leland HA, Rounds AD, Burtt KE, Gould DJ, Marecek GS, Alluri RK, et al. Soft tissue reconstruction and salvage of infected fixation hardware in lower extremity trauma. Microsurgery. 2018;38(3):259-63. [PubMed ID: 28509409]. https://doi.org/10.1002/micr.30176.
-
8.
Garay M, Hennrikus WL, Hess J, Lehman EB, Armstrong DG. Lawnmowers versus children: The devastation continues. Clin Orthop Relat Res. 2017;475(4):950-6. [PubMed ID: 27785676]. [PubMed Central ID: PMC5339136]. https://doi.org/10.1007/s11999-016-5132-5.
-
9.
Sutera D, Barbuscia L, Bonarrigo A, D'Angelo G, Gitto E. Intensive management of a crush syndrome case. Atti della Accademia Peloritana dei Pericolanti-Classe di Scienze Medico-Biologiche. 2020;108(1):1-5.
-
10.
Wen APY, Jusoh MH, Saad AZM, Halim AS, Faisham N, Azman WSW. Successful ankle replantation in two cases with different presentations. Arch Plast Surg. 2020;47(2):182-6. [PubMed ID: 31462030]. [PubMed Central ID: PMC7093274]. https://doi.org/10.5999/aps.2018.00514.
-
11.
Doucet JJ, Galarneau MR, Potenza BM, Bansal V, Lee JG, Schwartz AK, et al. Combat versus civilian open tibia fractures: The effect of blast mechanism on limb salvage. J Trauma. 2011;70(5):1241-7. [PubMed ID: 21610438]. https://doi.org/10.1097/TA.0b013e3182095b52.
-
12.
Gladden PB, Wilson CH, Suk M. Pediatric orthopedic trauma: Principles of management. Semin Pediatr Surg. 2004;13(2):119-25. [PubMed ID: 15362282]. https://doi.org/10.1053/j.sempedsurg.2004.01.008.
-
13.
Buza JA, Leucht P. Fractures of the talus: Current concepts and new developments. Foot Ankle Surg. 2018;24(4):282-90. [PubMed ID: 29409210]. https://doi.org/10.1016/j.fas.2017.04.008.
-
14.
Khan MA, Javed AA, Rao DJ, Corner JA, Rosenfield P. Pediatric traumatic limb amputation: The principles of management and optimal residual limb lengths. World J Plast Surg. 2016;5(1):7-14. [PubMed ID: 27308235]. [PubMed Central ID: PMC4904133].
-
15.
Solove M, Turcotte Benedict F. Ankle injuries in the pediatric emergency department. Pediatr Emerg Care. 2020;36(5):248-54. [PubMed ID: 32355069]. https://doi.org/10.1097/PEC.0000000000002097.