1. Context
Wolff-Parkinson-White (WPW) syndrome is a congenital cardiac pre-excitation syndrome, which occurs due to the presence of one or more accessory pathways (1). Multiple studies of children and adults have reported the incidence of WPW to be 1 - 3 per 1,000 (0.1% - 0.3%) (1). WPW is rarely associated with congenital cardiac anomalies, while the Ebstein anomaly and hypertrophic cardiomyopathy may be concomitant with WPW (2). Familial WPW has a higher prevalence (0.55%) among the first-degree relatives of an index patient with WPW (1).
The hallmark of the electrocardiographic (ECG) findings on WPW include the short PR interval of < 0.12 seconds, prolonged QRS with the total duration of > 0.12 seconds with an initial slurring and slow rise (delta wave) in the presence of the sinus rhythm, and abnormal ventricular repolarization (3). WPW is also considered as benign arrhythmia, and the patients may experience symptoms that are associated with arrhythmia, such as palpitations, dizziness, syncope, dyspnea, chest pain, and sudden cardiac death (SCD) (1, 3). The WPW ECG pattern is caused by early ventricular depolarization through an accessory pathway, which bypasses the normal cardiac conduction system (4). The accessory pathway allows impulses to propagate in a retrograde manner, which in turn leads to reentrant supraventricular tachycardia or sudden death (5).
Most of the patients with WPW remain asymptomatic throughout their life, and the risk of sudden death in these patients is approximately 0.25% per year or 3% - 4% over a lifetime (3). The incidence of asymptomatic WPW progressing to arrhythmia has been estimated at 1% - 2% per year (1). Therefore, an immediate treatment or intervention is not required in the patients with an asymptomatic WPW ECG pattern (3).
SCD is the first and only manifestation of WPW in some patients (1). Based on the guidelines of the American College of Cardiology and European Society of Cardiology, prophylactic radiofrequency catheter ablation is only used to manage asymptomatic patients with high-risk occupations (6). Radiofrequency catheter ablation is an invasive procedure, which may lead to complications such as thromboembolism, hemorrhage, infection, cardiac perforations, and new arrhythmias; nevertheless, the complication rate is relatively low (6). In general, the benefits of prophylactic catheter ablation may outweigh the risks.
This review aimed to investigate whether prophylactic ablation could improve the long-term outcomes of asymptomatic patients with WPW.
2. Methods
A systematic literature search was performed in databases such as PubMed, Google Scholar, and Cochrane Library for the relevant articles published during 2000 - 2020. The search terms included catheter ablation AND Wolff-Parkinson-White, radiofrequency ablation AND Wolff-Parkinson-White, and prophylactic ablation AND Wolff-Parkinson-White. Additional studies of interest were retrieved from the reference lists of the selected articles. The tiles and abstracts of the retrieved studies were screened to assess their eligibility for inclusion in the review. In case of indecision based on the titles and abstracts, the full text of the articles was used to assess the eligibility. Only original studies, cohorts, and randomized controlled trials (RCTs) focused on WPW patients undergoing radiofrequency ablation were selected, and review studies, case reports, and RCTs on animals were excluded.
3. Results
3.1. Long-Term Risk of Mortality and Atrial Fibrillation in WPW Syndrome
Some studies have suggested that the radiofrequency ablation of accessory pathways could prevent the recurrence of atrial fibrillation, while recent studies have indicated that the patients had a high incidence of atrial fibrillation even after ablation (7-9). Table 1 shows the all-cause mortality rates in the patients with WPW syndrome undergoing catheter ablation compared to those not receiving ablation and individuals without WPW.
| Study | Study Design | Patient Populations | Duration of Follow-Up | Mortality Rate |
|---|---|---|---|---|
| Borregaard et al., 2014 (7) | Retrospective Cohort | 362 in WPW without ablation; 3,619 in control with no WPW | 8.8 years in WPW without ablation; 8.6 years in control with no WPW | 5.3% in both groups |
| Bunch et al., 2015 (8) | Retrospective Cohort | 872 in WPW with ablation; 1,461 in WPW without ablation; 11,175 in control with no WPW | 7.9 ± 5.4 years in WPW with ablation; 7.9 ± 6.2 years in WPW without ablation; 7.5 ± 5.5 years in control with no WPW | 6.1% in WPW with ablation; 19.6% in WPW without ablation; 14.0% in control with no WPW |
| Wongcharoen et al., 2018 (9) | Prospective Cohort | 381 in WPW with ablation; 1,524 in WPW without ablation; 2,108 in control | 10.3 ± 1.9 years in WPW with ablation; 9.6 ± 2.9 years in WPW without ablation; 10.5 ± 1.8 years in control with no WPW | 17.3% in WPW with ablation; 25.2% in WPW without ablation; 11.8% in control with no WPW |
Abbreviation: WPW, Wolff-Parkinson-White.
The study by Borregaard et al. (7) was conducted on 362 consecutive patients with WPW syndrome who underwent radiofrequency ablation. The WPW patients were matched to the controls (n = 3,619) with the ratio of 1:10 in terms of age and gender, and the obtained results showed no significant difference in terms of long-term mortality between the WPW group and individuals without the condition. However, the risk of atrial fibrillation was higher in the WPW patients (9.3%) compared to the individuals without the syndrome (1.9%) (7).
The study by Bunch et al. (8) was conducted on three groups of patients, including 872 WPW patients with ablation, 1,461 WPW patients without ablation, and 1:5 control population (n = 11,175). The results of the mentioned study indicated that the mortality rate of the WPW patients receiving ablation was lower than those without ablation, while the long-term mortality rates were similar in the WPW and non-WPW patients. In addition, the non-ablated WPW patients had a lower risk of atrial fibrillation compared to the ablated WPW patients (8).
The study by Wongcharoen et al. (9) was performed on 1,524 non-ablated WPW patients, 381 ablated WPW patients, and 2,108 controls. According to the findings, the long-term mortality of the WPW patients undergoing ablation was lower compared to the patients without ablation. However, the ablation group had a higher incidence of coronary events compared to the non-ablation group (9).
3.2. Prophylactic Ablation in Asymptomatic WPW Patients
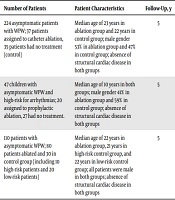
The results of two RCTs suggested that prophylactic ablation may reduce arrhythmic events in high-risk pediatric and adult patients, while one clinical trial indicated no significant risk reduction in arrhythmia in the patients undergoing the prophylactic radiofrequency catheter ablation of the accessory pathways (Table 2).
| Study | Study Design | Number of Patients | Patient Characteristics | Follow-Up, y | Main Findings |
|---|---|---|---|---|---|
| Pappone et al., 2003 (10) | RCT | 224 asymptomatic patients with WPW; 37 patients assigned to catheter ablation, 35 patients had no treatment (control) | Median age of 23 years in ablation group and 22 years in control group; male gender 53% in ablation group and 47% in control group; absence of structural cardiac disease in both groups | 5 | Two patients (5%) in ablation group and 21 patients (60%) in control group had arrhythmic events. |
| Pappone et al., 2003 (11) | RCT | 47 children with asymptomatic WPW and high-risk for arrhythmias; 20 assigned to prophylactic ablation, 27 had no treatment. | Median age of 10 years in both groups; male gender 41% in ablation group and 59% in control group; absence of structural cardiac disease in both groups | 5 | One patient (5%) in ablation group and 12 patients (44%) in control group had arrhythmic events. |
| Ozenc et al., 2014 (12) | Clinical trial | 110 patients with asymptomatic WPW; 80 patients ablated and 30 in control group (including 10 high-risk patients and 20 low-risk patients) | Median age of 22 years in ablation group, 21 years in high-risk control group, and 22 years in low-risk control group; all patients were male in both groups; absence of structural cardiac disease in both groups | 5 | Eight patients (10%) had an arrhythmic event in ablation group, and two patients had supraventricular tachycardia in both high-risk control group (20%) and low-risk control group (10%). |
Abbreviations: RCT, randomized controlled trial; WPW, Wolff-Parkinson-White.
The study by Pappone et al. (10) was conducted on 224 eligible asymptomatic patients with WPW, and the high-risk patients for arrhythmias were randomly assigned to the groups of the radiofrequency catheter ablation of the accessory pathways (n = 37) and no treatment (n = 35). The obtained results indicated the risk reduction of 92% over a five-year follow-up period in the asymptomatic patients who underwent prophylactic radiofrequency ablation (10).
Another study by Pappone et al. (11) was performed on 47 children with WPW who were considered high-risk for arrhythmias, with 20 patients undergoing prophylactic ablation and 27 receiving no treatment. The results of the mentioned study suggested that prophylactic ablation had significant and durable benefits for the children with asymptomatic WPW syndrome who were considered high-risk for arrhythmias.
The clinical trial by Ozenc et al. (12) was conducted by 110 asymptomatic patients with a WPQ electrocardiographic pattern, with 80 patients ablated and 30 receiving no treatment. The findings indicated no significant risk reduction for arrhythmias in the patients undergoing the prophylactic radiofrequency catheter ablation of the accessory pathways (12).
4. Discussion
According to the literature, the catheter ablation of the accessory pathway could improve the left ventricular function, normalized QRS duration, and mechanical resynchronization in patients with WPW (13, 14). Therefore, catheter ablation is an effective first-line treatment for the prevention of SCD and reduction of the associated mortality rate. In this regard, the findings of Wongcharoen et al. (9) indicated that the patients who underwent ablation were at the significantly high risk of developing coronary artery disease in the long run compared to those not receiving an ablation. Coronary artery injury has been reported to be a complication caused by radiofrequency ablation as the coronary artery is in close proximity to the commonly ablated sites of the accessory pathway (15, 16). As such, the closer distance of the ablation site to the coronary artery is associated with the higher risk of coronary artery injury (15).
A few studies have also denoted that the ablation of the accessory pathway cannot prevent the recurrences of atrial fibrillation (17, 18). For instance, Dagres et al. (17) reported that the recurrent rate of atrial fibrillation was 20% after successful radiofrequency ablation, while the incidence rate was higher in the older patients. Furthermore, Derejko et al. (18) stated that the incidence rate of atrial fibrillation was 19%after ablation. The occurrence of atrial fibrillation after catheter ablation might be affected by the incidence of atrial fibrillation before catheter ablation (7). On the other hand, the high incidence of atrial fibrillation in WPW may cause the electrical remodeling of the atrium, which eventually leads to the higher rate of atrial fibrillation after ablation (7). Patients aged 50 or more are at the higher risk of developing atrial fibrillation after successful ablation (19). In addition, the incidence of atrial fibrillation may be due to atrial myopathy (8). Atrial fibrillation in WPW has a shorter effective refractory period of the pulmonary veins and longer maximal veno-atrial conduction delay (18). Moreover, inducible atrial fibrillation in these patients is associated with the higher risk of supraventricular and ventricular arrhythmias after ablation (8). Nevertheless, the risk of post-ablation atrial fibrillation is not affected by the location of the accessory pathway (20).
Previous findings have indicated that ablation could reduce the mortality rate in WPW patients although the recurrence rate of atrial fibrillation is relatively high (8, 9). This may be due to the fact that the patients who undergo ablation have more awareness about other cardiac diseases as they visit cardiologists more frequently (8). Therefore, prophylactic ablation may decrease the mortality risk of asymptomatic WPW given the effectiveness of the therapy in symptomatic patients.
Electrophysiological and population-based studies have suggested the low rate of sudden death among asymptomatic patients with WPW syndrome (10). Furthermore, the risk of SCD has been shown to be low in symptomatic pediatric patients and even lower in asymptomatic patients in the absence of cardiac diseases (21). In pediatric patients, symptomatic and asymptomatic WPW are associated with a similar risk of long-term SCD (21). In this regard, the meta-analysis by Obeyesekere et al. (22) showed that the risk of SCD in asymptomatic patients was 1.93 per 1,000 patients per year in the pediatric population as opposed to 0.86 per 1,000 patients per year in the adult population. On the other hand, a large-scaled, prospective, long-term follow-up study on 162 asymptomatic patients indicated that three patients had ventricular fibrillation (1.85%), and only one patient had SCD (23). Multiple accessory pathways in the right and left sides of the septum are considered to be an important risk factor for ventricular fibrillation in WPW patients (24). Therefore, the ablation of multiple pathways could prevent the occurrence of ventricular fibrillation and SCD (25). In addition, the WPW patients who only have minimally symptomatic atrial fibrillation may proceed to ventricular fibrillation and SCD (23). It is rather difficult for physicians to stratify or identify the risk of SCD in asymptomatic WPW patients; the reason is that although the patients have an unpredictable risk of SCD in the long run, only a small number are actually at risk (25).
In another study in this regard, the effectiveness of radiofrequency ablation in asymptomatic patients with WPW was reported to be low as 112 patients received treatment for one patient to have a reduced risk of death after three years (6). The reliable indication for ablation is a combination of inducible atrioventricular reciprocating tachycardia and short refractory RR interval in the atrial fibrillation (≤ 250 ms) based on electrophysiological testing (25). However, invasive electrophysiological testing has a low predictive value to justify the use of prophylactic ablation in the risk analysis of asymptomatic WPW patients (6). Routine electrophysiological testing and the prophylactic ablation of the accessory pathways are considered essential in asymptomatic patients since SCD could present as a symptom in some patients with WPW (18). Moreover, electrophysiological testing plays a key role in the identification of high-risk patients for subsequent ventricular fibrillation and SCD prevention (25). However, the risk of sudden death is relatively low in asymptomatic patients (1 per 1,000 patients per year), and these patients have been reported to be at 30% risk of becoming symptomatic (6). If all the asymptomatic patients with WPW were treated and tested, many patients would be treated unnecessarily and exposed to the risks and complications of electrophysiological studies and ablation (26). According to several surveys, most electrophysiologists decide to perform radiofrequency ablation on asymptomatic patients since the negative predictive value is not 100%, and they need to avoid the risk of SCD (27, 28).
According to the literature, the incidence of periprocedural complications for catheter ablation is relatively low (2.9%), while the risk of 1.5 per 1,000 of requiring a cardiac stimulator has been reported (6, 29). Furthermore, the success rate and risk of ablation depend on the pathway location as the ablation of pathways in the septal area may lead to heart block, and the ablation of left-sided pathways could increase the risk of transseptal puncture or retrograde aortic approach (25). Therefore, prophylactic ablation should only be recommended to the patients presenting with the prominent risks factors for SCD.
Older patients may present with a more threatening form of WPW, which could lead to SCD (30). Moreover, males are at a higher risk of SCD compared to females as reported by Timmermans et al. (30) and Obeyesekere et al. (22). In addition, some electrophysiological properties of the accessory pathway may be associated with the increased risk of SCD, such as the loss of pre-excitation, short refractory RR interval in the atrial fibrillation of ≤ 250 milliseconds, anterograde effective refractory periods of ≤ 250 milliseconds, inducible atrioventricular reciprocating tachycardia, and multiple accessory pathways (26). Finally, the presence of structural cardiac diseases and septal localization are among the risk factors for SCD (26).
5. Conclusions
According to the results, prophylactic ablation is effective in the prevention of arrhythmic events in asymptomatic patients with WPW. However, the risk of asymptomatic patients becoming symptomatic or presenting with SCD is relatively low. The benefits of prophylactic ablation in asymptomatic patients are limited. If all the asymptomatic patients are to receive treatment, many patients may be exposed to the risks of electrophysiological studies and catheter ablation. Therefore, these patients should consult their physician about whether benefits such as decreased mortality and increased quality of life outweigh the risks associated with the procedures. In addition, the asymptomatic patients who are classified as high-risk based on electrophysiological examinations or other factors with a low risk of complications based on localization may be recommended to undergo prophylactic ablation.