Abstract
Introduction:
Eccrine poroma is a benign neoplasm thought to derived from Eccrine sweat glands. Recently, studies have shown wide distribution of Eccrine poroma, including acral, face, and abdomen forms.Case Presentation:
We reported a 65-years-old woman with rapidly growing 5-cm ulcerative Eccrine poroma with active bleeding since one year prior to presentation.Conclusions:
Although rapid growth and bleeding can be related to malignancy and biopsy is necessary to be performed, benign lesions can present with mentioned symptoms. Physicians should be aware that benign poroma can present as an ulcerative and large neoplasm.Keywords
1. Introduction
The eccrine poroma is an adnexal neoplasm composed of growing cuboidal monomorphic cells, which shows ductal differentiation. These cells arise from the intra-epidermal portion of the eccrine duct and extend into the dermis. The disease was first described in 1956 (1) presented as a soft, reddish papule protruding from a depression. It is thought to occur most on acral skin, especially the soles or feet sides, but it can be presented on face, chest, and abdomen. Typically, it is seen in adulthood with no sex predilection. The size of eccrine poroma has been reported from a few millimeters to 6 cm (2, 3). Rarely, numerous poromas can develop in a generalized distribution, which make a clinical pattern namely poromatosis (4). Eccrine poroma pathogenesis is still unknown.
Multiple lesions of eccrine poroma have been reported in patients with history of chronic radiation and patients with mycosis fungoides treated with electron beam therapy (5-7) and rare cases reported with correlation to pregnancy.
We reported an ulcerative poroma in a 65-years old woman. We reported this case because there are few reports of ulcerative eccrine poroma with fast development and a benign pathology. Moreover, this was a rare case, because its appearance was like a squamous cell carcinoma.
2. Case Presentation
A 65-years-old fair skin woman (skin type 1) presented with a rapidly growing, reddish tumor since one year ago on lateral part of her right leg, which was approximately 5 cm in diameter (Figures 1 and 2). She denied any pain, but complained about sudden growth and bleeding. When the lesion first appeared, it was a small papule. She did not have any other medical problems and was otherwise healthy.
A Moist Ulcerative Reddish Tumor

Close View of Tumor With Bleeding Spot in it

On physical examination, a moist 5-cm ulcerative reddish tumor was seen on her right leg. Its differential diagnosis included pyogenic granuloma, squamous, and basal cell carcinoma and amelanotic melanoma. A 2-mm deep ellipse biopsy was obtained from the superior portion of the lesion.
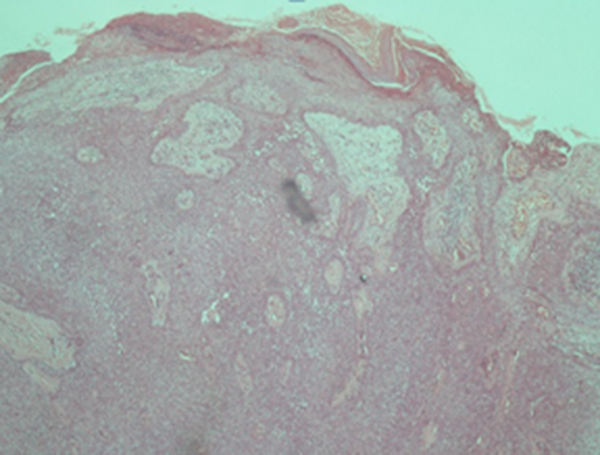
Histopathology demonstrated a dermal proliferation of cuboidal cells extensively connected to the epidermis. There were multiple duct structures and a supporting fibro-vascular stromal (Figure 3). No malignant changes reported. We decided to excise the lesion completely.
Histopathology of the Tumor
3. Discussion
Goldman et al. was the first who unified two terms of eccrine and apocrine poroma (1). Many studies have shown evidence that poromas may arise from both eccrine and apocrine sweat glands (4, 8). Its differential diagnosis includes pyogenic granuloma, hemangioma, seborrheic keratosis, verruca, fibroma, melanoma, nevus, cysts and basal and squamous cell carcinoma (9). There are four different variants of poroma including eccrine poroma, intraepidermal poroma, intradermal tumor and poroid hidradenoma (2). The above four variants are histopathologically differentiated from each other by where the neoplastic cells are located.
An eccrine poroma invades the basal layer of the epidermis and the upper part of the dermis by neoplastic poroid cells; however, poroid cells, intracytoplasmic or intercellular vacuolization to form ducts, necrosis and monomorphism of nuclei may be consistent features of all histopathologic variants. Sweat gland tumors are 1% of all primary skin lesions and eccrine poroma represents 10% of these tumors. Moreover, benign neoplasms can precede the development of malignant neoplasm and the benign poroma can change to the porocarcinoma (10-12).
Spontaneous bleeding, pain and sudden growth have been presented as signs and symptoms, which could alarm development of porocarcinoma (13). Although, some skepticism has been mentioned about the reliability of above symptoms, some patients seek medical attention due to rapid growth of tumor. In a study, 11 of 69 cases with eccrine porocarcinomas, appeared to arise with a benign preexistent poroma (10).
However, in another report less than 1% of porocarcinoma were mixed with benign eccrine poroma. As a result, further studies are required before any reclassification (14). Surgical treatment is optimal. Electrosurgical destruction, carbon dioxide laser-assisted removal or surgical excision may be performed. Topical treatments such as 1% atropine solution have been reported beneficial in the treatment of superficial lesions (9). We decided to excise the lesion fully, because there was still uncertain amount of risk for malignant transformation.
We presented an ulcerative poroma in a 65-years-old woman. There are few reports of ulcerative eccrine poroma with fast development and a benign pathology in the literature. In addition, this was a rare case, because its appearance was like a squamous cell carcinoma. Literature reported eccrine poroma in unusual sites like face (12), and reported ulcerative eccrine poroma with slow growth, which was porocarcinoma in pathology (12). Our case is special due to rapid growth in a female with skin type 1 who worked in farm and had been exposed with sun for many years. Another surprising point of our case was the lesion appearance and pain, which were both like a malignant neoplasm.
Even though an eccrine poroma has typical histopathological features, it has a propensity toward varied clinical presentations. Hence, such atypical nodules require a biopsy for confirmation of diagnosis and further management. Physicians should be aware that benign lesions can present with mentioned symptoms, which can be confusing with malignant lesions, but biopsy and pathologic assessment can help for further managements.
References
-
1.
Goldman P, Pinkus H, Rogin JR. Eccrine poroma; tumors exhibiting features of the epidermal sweat duct unit. AMA Arch Derm. 1956;74(5):511-21. [PubMed ID: 13361538].
-
2.
Abenoza P, Ackerman AB. Neoplasms with eccrine differentiation. In: Ackerman AB, editor. Ackerman's Histologic Diagnosis of Neoplastic skin diseases, a method by pattern Analysis. 1. Philadelphia, PA: Lea and Febiger; 1990. p. 113-85.
-
3.
Brenn T, Mckee PH. Tumors of the sweat glands. In: Mckee PH, Calonje E, Brenn T, Lazar A, editors. Pathology of the skin. 4 ed. Philadelphia; 2005.
-
4.
McCalmont TH. Adnexal neoplasms. In: Bolognia JL,, Jorizzo JL, Rapini RP, editors. Dermatology. 2 ed. Mosby: Elsevier; 2008. 1704–5 p.
-
5.
Goldner R. Eccrine poromatosis. Arch Dermatol. 1970;101(5):606-8. [PubMed ID: 5444082].
-
6.
Ullah K, Pichler E, Fritsch P. Multiple eccrine poromas arising in chronic radiation dermatitis. Acta Derm Venereol. 1989;69(1):70-3. [PubMed ID: 2563613].
-
7.
Kurokawa M, Amano M, Miyaguni H, Tateyama S, Ogata K, Idemori M, et al. Eccrine poromas in a patient with mycosis fungoides treated with electron beam therapy. Br J Dermatol. 2001;145(5):830-3. [PubMed ID: 11736912].
-
8.
Kamiya H, Oyama Z, Kitajima Y. "Apocrine" poroma: review of the literature and case report. J Cutan Pathol. 2001;28(2):101-4. [PubMed ID: 11168759].
-
9.
Agarwal S, Kumar B, Sharma N. Nodule on the chest. Eccrine poroma. Indian J Dermatol Venereol Leprol. 2009;75(6):639. [PubMed ID: 19915263].
-
10.
Robson A, Greene J, Ansari N, Kim B, Seed PT, McKee PH, et al. Eccrine porocarcinoma (malignant eccrine poroma): a clinicopathologic study of 69 cases. Am J Surg Pathol. 2001;25(6):710-20. [PubMed ID: 11395548].
-
11.
Ahmed TSS, Priore JD, Seykora JT. Tumours of the Epidermal Appendages. In: Elder DE,, Rosalie E, Johnson BL, editors. Lever's Histopathology of the Skin. 10 ed. Wolters Kluwer: Lippincott Williams and Wilkins; 2005. 885–8 p.
-
12.
Mahajan RS, Parikh AA, Chhajlani NP, Bilimoria FE. Eccrine poroma on the face: an atypical presentation. Indian J Dermatol. 2014;59(1):88-90. [PubMed ID: 24470670].
-
13.
Pylyser K, De Wolf-Peeters C, Marien K. The histology of eccrine poromas: a study of 14 cases. Dermatologica. 1983;167(5):243-9. [PubMed ID: 6317476].
-
14.
Choi CM, Cho HR, Lew BL, Sim WY. Eccrine porocarcinoma presenting with unusual clinical manifestations: a case report and review of the literature. Ann Dermatol. 2011;23 Suppl 1:S79-83. [PubMed ID: 22028580].