Abstract
Background:
Polyacrylamide gel (PAAG) has been used extensively for soft tissue augmentation. Complications of PAAG injection mandate evacuation of filler.Objectives:
This study aimed to introduce a new method of evacuating PAGG with the help ultrasonography markings on face.Patients and Methods:
We enrolled patients who were unsatisfied with the results of injection or had developed complications such as induration, gel migration, or infection referred to our clinic to evacuate the filler since 2011. Patients were examined by ultrasonography and a radiologist reported the volume, place, and depth of gel as well as fibrosis and marked them on the patients’ face or its photographs. We used Barikbin’s tumescent solution to facilitate the evacuation of concentrated gel and reduce the risk of injury to vital tissues. We inserted a 16G-fat-transfer cannula through a hole on the nasolabial folds and evacuated the gel by vacuum force and milking. We also used a Barikbin’s blunt subcision blade to dissect fibrosis. The evacuated region was irrigated by tumescent solution. Patients’ satisfaction was assessed by visual analogue scale (VAS). The procedure was repeated at four-week interval until achieving favorable results.Results:
We treated 173 patients, including 164 females (94.8%), with the mean (SD) age of 43.75 (10.62) years. According to VAS, 95.4% of patients reported complete satisfaction while 2 (1.2%) were unsatisfied with the results. Patients reported no complication of therapy.Conclusions:
Our method provided good results and performing evacuation under the guide of bedside ultrasonography is recommended.Keywords
Polyacrylamide Gels Ultrasonography Cannula Visual Analogue Scale
1. Background
Polyacrylamide gel (PAAG) is a synthetic and durable filler, which is used in dermatology and plastic surgery to augment skin defects of the face and breasts. This translucent material is composed of 2.5% 5% cross-linked polyacrylamide and sterile water. In contrast to other biocompatible fillers, i.e. collagen, hyaluronic acid, and calcium hydroxyapatite, PAGG provides permanent effects as it cannot be degraded by enzymes and hence, it is not bioresorbable (1, 2).
Although finding a material with permanent effects was a great advance in the preceding decades, these materials have their own downsides. While the manufacturer states that PAAG is not displaced easily or cause allergic reactions, fibrosis, or capsules (3), the literature as well as our experience shows that these complications are quite frequent (2, 4-6).
When complications such as foreign body reaction to PAAG, induration, migration, or infection develop, the filler should be removed; however, it is a difficult procedure and despite multiple attempts to extract, some residues would remain. Milking and aspiration through a needle were previously used to remove PAAG in face (7). In addition, ultrasonography (USG) is an effective tool in determining the type and location of injected fillers (8). The USG was used in determining the locations and more precise aspiration of fillers by large-bore syringes in unsatisfactory or displaced PAGG in facial or breast augmentation (9).
2. Objectives
We aimed to remove PAAG with a new technique using Barikbin’s tumescent solution (BTS), Barikbin’s blunt subcision blade (BBSB), and fat-transfer cannula in patients with complicated or displaced injected materials. In this method, the exact site of PAAG was determined by USG and marking the sites on face or photographs before removal of materials.
3. Patients and Methods
This study was performed in a private clinic under supervision of Tehran University of Medical Sciences, Tehran, Iran. The Ethic Committee of the university approved the protocol of the study.
Since 2011, patients who were referred to our clinic for removal of the injected PAAG in different regions of their face were included. The reasons for PAAG removal were being unsatisfied with the results or developing complications of injection such as induration, migration, or infection. The filler was injected in malar region, lips, nasolabial fold, marionette line, chin, and mandibular angle. Patients with coagulopathies or evidence of injected fillers other than PAGG were excluded. Data concerning basic characteristics, region of injection, and complications were documented. All patients signed a written informed consent before initiating the diagnostic and therapeutic procedures.
3.1. Method of Evacuation
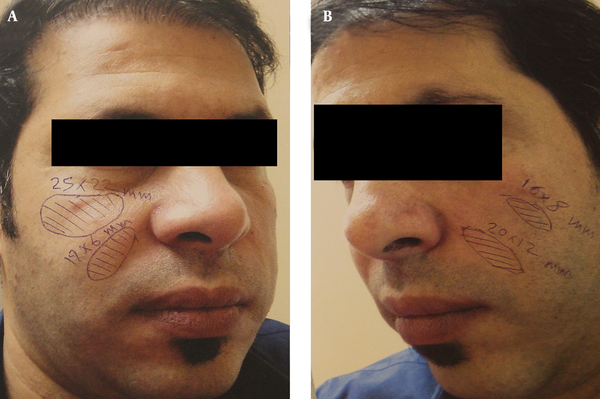
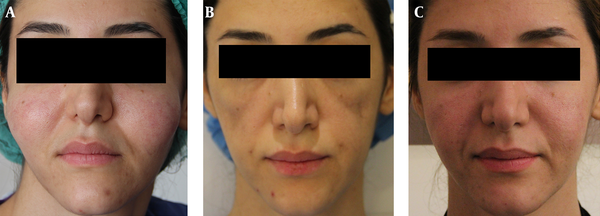
When examining the patients’ face to detect PAAG, some foci of filler accumulation might be missed due to their small size or deep location; hence, we used USG to detect sites of PAGG and mark the sites on face before evacuations. Patients were asked to take medical photographs of face and were referred to a radiologist. The radiologist examined the patients employing 10-MHz ultrasound probe. The radiologist determined the size and depth of PAAG foci and location of fibrosis in his report. Moreover, he drew lines and wrote the size of each focus of PAAG and fibrosis on photographs of the patient’s face by two pens with different colors and sent them back to us (Figure 1). Then we marked the face according to the photographs. This method was used for two-thirds of patients; however, we decided to mark the patients face at the time of performing USG. Therefore, for the rest of patients, we asked the radiologist to determine the foci of fibrosis and PAAG accumulation on the patients’ face and then sent them to take medical color photographs of face from different views (Figure 2). This improves the accuracy of dermatologist surgeon performance during evacuation. Nonetheless, we had to prepare the face for procedure and hence, we had to draw marks again according to photographs when they were erased.
Before the procedure, patient was sedated with one acetaminophen/codeine (300 mg/20 mg) and an alprazolam (1 mg) tablets. After using povidone iodine on the skin to disinfect the area, a special tumescent solution (BTS) was injected subcutaneously into the skin to provide local anesthesia, induce vasoconstriction for decreasing the risk of hemorrhage and hematoma formation, improve access to the filler focus, and facilitate evacuation by diluting the PAAG (Figure 3 A, 3B). The BTS consisted of epinephrine (0.5 mg), 2% lidocaine (30 mL), triamcinolone acetonide (40 mg), and gentamycin (80 mg) in 500 mL of 0.9% saline.
After 15 minutes, on the top of the detected nodule, which was palpated through physical examination, a circle was drawn by a marker to improve localization of the nodule. Thereafter, a 2-mm hole was made by an 18G needle in nasolabial fold or across marionette line and a 16G-fat-transfer cannula was inserted through the hole. By slow and slight pressure, the cannula was guided to the nodule and penetrated through its wall. A 20-mL syringe was used to vacuum the material within the nodule (Figure 3 C). The aspiration was performed until no more materials could be evacuated. This process was repeated for all nodules that had been determined by the radiologist plan. Then the residual materials were extracted by slight pressure on the skin and milking (Figure 3 D). In rare cases, when some of the fillers’ foci were left and could not be accessed through the prepared hole, another hole was made over the site for local evacuation. After finishing extracting the gel with this method, we irrigated the location of evacuated filler and tissue spaces with BTS.
In case of fibrotic lesions, subcision with BBSB (under print work) was performed to dissect fibrotic band and facilitate the evacuation. The holes were dressed with mupirocin ointment and one layer of sterile gauze. Oral antibiotics including oral clindamycin (150 mg, TDS), ciprofloxacin (500 mg, bid), acyclovir (400 mg, TDS), and topical mupirocin were prescribed for seven days and patient was visited one week later. After 30 days, another USG examination would be performed to detect residual materials and the same process was repeated at one-month intervals until achieving satisfactory results.
In order to complete the treatment and achieve favorable cosmetic results, we augmented the evacuated areas with hyaluronic acid fillers or autologous fat injection, based on several items differing from one patient to another.
The primary endpoint measure of the study was introducing a method of PAAG evacuation with the help of USG marking in a large sample of patients. Moreover, patients’ satisfaction was measured subjectively through a visual analogue scale (VAS) with zero and ten indicating the least and the most satisfied status, respectively.
Since a long time had elapsed from the injection of PAAG, we could not trace back the amount of injected filler or the manufacturer of PAAG. Moreover, there was no standard treatment for comparing the results with; therefore, we could not recruit a control group and or randomize the study.
3.2. Statistical Analysis
We aimed to introduce a new method of treatment and without a control group and most of our data were presented as report of distribution. Nonetheless, SPSS 16.0 (SPSS Inc. Chicago, Illinois, the United States) was used to analyze data and report the descriptive findings. Pearson’s correlation coefficient was used to determine any possible correlation between variable. P > 0.05 was considered statistically significant.
Marking the Site of Gel Accumulation on the Photographs of Patient’s Face by Radiologist at the Time of Ultrasonography
Photographs After Marking the Face During Ultrasonography in a Fifty-Three-Year-Old Woman With Induration of Polyacrylamide Gel

Evacuation of Polyacrylamide Gel in a Sixty-One-Year-Old Woman With Induration and Gel Migration

4. Results
Among 179 patients with complicated filler injection, we evacuated PAAG in 173 patients including nine males (5.2%) and 164 females (94.8%). The mean (SD) age of the patients was 43.75 (10.62) years (range, 23-72 years). Seven patients (4%) were referred for abscess formation, 28 (16.2%) for migration, and 138 (79.8%) for induration of filler. Regarding assessment of subjective satisfaction on VAS, 165 patients (95.4%) had reported full satisfaction (VAS score of 10). Only two patients (1.2%) were almost unsatisfied with the results (VAS score of 5). One of them was a 23-year-old man who had received three treatment sessions but no reconstruction treatment and another one was a 51-year-old woman who had received four treatment sessions; however, she experienced infection after autologous fat-transfer in another center. Overall, 98.2% of patients reported favorable satisfaction (VAS score, 8-10) with the treatment. In 87 patients (50.3%), a single session of evacuation led to patients’ satisfaction and less than 5% of patients needed more than four treatment sessions. There was no association between age of patients and satisfaction of results (r = 0.107; P = 0.162). Patients reported no serious complication except edema and ecchymosis of the face, which resolved within ten days, as well as some degrees of pain, which was controlled by over-the-counter analgesics. Overall, 38 patients (22%) received reconstruction therapy (Figure 4) by the date of preparing this report.
A Thirty-Five-Year-Old Woman with Polyacrylamide Gel Induration and Immigration
5. Discussion
We successfully evacuated PAAG in a large number of patients with complications of injecting this filler. According to patients’ report, more than 98% had achieved favorable to complete satisfaction with the results and few negligible adverse effects were seen. In the first session of evacuation, the main bulk of fillers were extracted and the change in appearance would be sensible, which justifies full satisfaction in almost half of patients after the first session. The satisfactory results were independent of the patients’ age.
Injecting cosmetic fillers is increasing worldwide and desiring a cheap permanent filler had led to increased use of PAAG as filler in cosmetic procedures. Although there are some reports on the safety of PAAG in long-term, we frequently see complications including induration, immigration, and infection, years after injection, in our clinics. Most of these safety reports are from treatment of patients with human immunodeficiency virus (HIV)-related facial lipodystrophy. For instance, Rauso et al. (10) and De Santis et al. (11) reported safety and efficacy of PAAG after respectively 18-month follow-up of 32 patients and at least five-year follow-up of 141 patients with HIV-related facial lipodystrophy. Moreover, Pallua and Wolter reported more than 65% satisfaction with the results in 251 healthy patients and low rate of complications in a 60-month follow-up (12). Nonetheless, there are numerous reports on the complications of PAAG during recent years (2, 4-6, 13). For instance, Manafi et al. reported 98 patients with dissatisfactory results and complications of PAAG injection including inflammation, infection, abscess formation, and gel migration, which were treated with incision, milking, and irrigation (13) also, Reda-Lari et al. reported a complication rate of 8.4% among more than 1300 patients after three-month to six-years follow-up (14).
Before removal or evacuation of complicated PAAG, the exact location and size of the materials must be determined. Although T2-weighted magnetic resonance imaging (MRI) without fat suppression seems to be the best radiologic study to detect the nodules (15), it is not practical due to the cost of MRI and needed time to perform the imaging. Therefore, most of the studies have used USG because it is available almost everywhere, is quick, has low cost, and lacks adverse effects of irradiation to the head and neck (16). In USG images, PAAG is detected as an oval anechoic pseudocyst with increased echogenicity of the surrounding subcutaneous tissue (17).
Different methods have been used to remove the complicated filler. Wilson et al. employed USG report to evacuate PAAG through suction by a 14G, 1.5-inch (3.81-cm) needle connected to a 10-mL syringe. They used distance from facial landmarks on the radiologist reports to find the nodules and used local anesthesia at the site of needle entrance, 5 to 7 mm below the nodule (7). Kavoussi and Ebrahimi used USG images and evacuated delayed PAAG indurations in 20 patients through making a hole on the skin by 16G needle and squeezing the nodule (18). Although Wolter and Pallua used stab incision to remove PAAG in lip asymmetry and reported favorable results (19), making incision in the face is not desirable as they might lead to permanent scar formation.
While many studies have recommended USG to guide the surgeon during evacuation of fillers, almost all studies have used the radiologist report to detect the nodules and site of deeper gel accumulations. To our knowledge, our study was the first study that had used the drawing on the face to determine the exact site of PAAG accumulation as well as its size. Moreover, we have become the referral center for removing PAAG during recent years and hence, we were able to report the largest number of patients with successful PAAG evacuation. We worked with a radiologist in our building who had considerable knowledge in performing USG examination and drawing lines on the patients’ face. We also used a special tumescent to make the nodule more accessible, provide more anesthesia, reduce the risk of injury to nerves and vessels, and dilute the concentrated gel. Moreover, we used fat-transfer cannula, which helped us with making a small hole on nasolabial fold instead of multiple insertions on different parts of skin needed when aspiration is made through needle. In addition, the blunt head of cannula minimized injury to vital parts of face and decreased adverse effects such as hematoma formation due to rupturing blood vessels or sensory defects due to nerve injury. By connecting the cannula to a 20-mL syringe, we were able to provide enough vacuum force to extract a large volume of viscous materials. Most patients stated full satisfaction after the first treatment session, which was due to removing the main bulk of filler in the first step. When evacuating PAAG, it is important to remove almost all the materials, as it is a good milieu for bacterial growth and might lead to abscess formation.
For the first time and by determining the fibrosis foci through USG, we dissected the fibrosis by inserting BBSB from the same hole made for evacuating PAAG. It led to better correction of deformities and patients’ satisfaction with results. Moreover, it made further corrections with injecting filler or autologous fat more acceptable.
Our study had some limitation. Although USG marking facilitated the evacuation, the nodules were mobile in most of the cases and as we had used the cannula, they just escaped the tip of instrument, which would mandate multiple attempts to rupture the fibrous wall of cyst; in addition, some of the nodules were small and might be missed by radiologist. Hence, we recommend bedside (real-time) USG and evacuation under the guide of USG. In fact, we have started this method in our center and have reached favorable results (not reported yet). The patients could not remember the brand of PAAG they had used and almost none of them remembered the amount of injected filler as long time had elapsed since treatment.
We could not measure the extracted materials exactly, but it ranged from 5 to 50 mL. In fact, it was impossible to determine the exact volume as some unknown reactions had increased the amount of extracted materials and using tumescent and irrigation at the end of procedure might have added to the extracted volume. Nevertheless, in almost all the patients, the volume of evacuated PAAG was more than expected injected volume and while the PAAG is a colorless material, the evacuated materials were yellow. Determining the exact composition of the extracted materials was hindered by high cost of the technology to analyze them and scarcity of laboratory that would perform it precisely; however, it seems that the yellow color was due to degrading fat tissue by PAAG that might explain the large volume of evacuated materials leading to face deformity.
In conclusion, we obtained favorable results in evacuating PAAG by employing USG report and marking the face of patients. Employing fat-transfer cannula and tumescent helped decrease the adverse events and complication of therapy. It is recommended to perform bedside USG and USG-guided evacuation in future studies.
References
-
1.
Breiting V, Aasted A, Jorgensen A, Opitz P, Rosetzsky A. A study on patients treated with polyacrylamide hydrogel injection for facial corrections. Aesthetic Plast Surg. 2004;28(1):45-53. [PubMed ID: 15116275]. https://doi.org/10.1007/s00266-003-3019-9.
-
2.
Kalantar-Hormozi A, Mozafari N, Rasti M. Adverse effects after use of polyacrylamide gel as a facial soft tissue filler. Aesthet Surg J. 2008;28(2):139-42. [PubMed ID: 19083518]. https://doi.org/10.1016/j.asj.2007.12.005.
-
3.
Christensen LH, Breiting VB, Aasted A, Jorgensen A, Kebuladze I. Long-term effects of polyacrylamide hydrogel on human breast tissue. Plast Reconstr Surg. 2003;111(6):1883-90. [PubMed ID: 12711948]. https://doi.org/10.1097/01.PRS.0000056873.87165.5A.
-
4.
Lee CJ, Kim SG, Kim L, Choi MS, Lee SI. Unfavorable findings following breast augmentation using injected polyacrylamide hydrogel. Plast Reconstr Surg. 2004;114(7):1967-8. [PubMed ID: 15577379].
-
5.
Evstatiev D. Late complications after injections of hydrogel in the breast. Plast Reconstr Surg. 2004;113(6):1878. author reply 1878-9. [PubMed ID: 15114178].
-
6.
Shen H, Lv Y, Xu JH, Hong XY, Zeng BW, Xiao W, et al. Complications after polyacrylamide hydrogel injection for facial soft-tissue augmentation in China: twenty-four cases and their surgical management. Plast Reconstr Surg. 2012;130(2):340-8. [PubMed ID: 22842430]. https://doi.org/10.1097/PRS.0b013e3182589b7d.
-
7.
Wilson YL, Ellis DA. Large needle suction aspiration of permanent fillers. Laryngoscope. 2011;121(10):2146-9. [PubMed ID: 21898418]. https://doi.org/10.1002/lary.21555.
-
8.
Wortsman X, Wortsman J, Orlandi C, Cardenas G, Sazunic I, Jemec GB. Ultrasound detection and identification of cosmetic fillers in the skin. J Eur Acad Dermatol Venereol. 2012;26(3):292-301. [PubMed ID: 21418333]. https://doi.org/10.1111/j.1468-3083.2011.04047.x.
-
9.
Cheng NX, Xu SL, Deng H, Ding XB, Zhang XM, Wu DH, et al. Migration of implants: a problem with injectable polyacrylamide gel in aesthetic plastic surgery. Aesthetic Plast Surg. 2006;30(2):215-25. [PubMed ID: 16547628]. https://doi.org/10.1007/s00266-005-0081-5.
-
10.
Rauso R, Freda N, Parlato V, Gherardini G, Amore R, Tartaro G. Polyacrylamide gel injection for treatment of human immunodeficiency virus-associated facial lipoatrophy: 18 months follow-up. Dermatol Surg. 2011;37(11):1584-9. [PubMed ID: 21806709]. https://doi.org/10.1111/j.1524-4725.2011.02131.x.
-
11.
De Santis G, Pignatti M, Baccarani A, Pedone A, Spaggiari A, Orlando G, et al. Long-term efficacy and safety of polyacrylamide hydrogel injection in the treatment of human immunodeficiency virus-related facial lipoatrophy: a 5-year follow-up. Plast Reconstr Surg. 2012;129(1):101-9. [PubMed ID: 22186503]. https://doi.org/10.1097/PRS.0b013e3182362142.
-
12.
Pallua N, Wolter TP. A 5-year assessment of safety and aesthetic results after facial soft-tissue augmentation with polyacrylamide hydrogel (Aquamid): a prospective multicenter study of 251 patients. Plast Reconstr Surg. 2010;125(6):1797-804. [PubMed ID: 20517105]. https://doi.org/10.1097/PRS.0b013e3181d18158.
-
13.
Manafi A, Emami AH, Pooli AH, Habibi M, Saidian L. Unacceptable results with an accepted soft tissue filler: polyacrylamide hydrogel. Aesthetic Plast Surg. 2010;34(4):413-22. [PubMed ID: 19452201]. https://doi.org/10.1007/s00266-009-9359-3.
-
14.
Reda-Lari A. Augmentation of the malar area with polyacrylamide hydrogel: experience with more than 1300 patients. Aesthet Surg J. 2008;28(2):131-8. [PubMed ID: 19083517]. https://doi.org/10.1016/j.asj.2007.12.004.
-
15.
Ginat DT, Schatz CJ. Imaging features of midface injectable fillers and associated complications. AJNR Am J Neuroradiol. 2013;34(8):1488-95. [PubMed ID: 22837310]. https://doi.org/10.3174/ajnr.A3161.
-
16.
Indrizzi E, Moricca LM, Pellacchia V, Leonardi A, Buonaccorsi S, Fini G. Biomaterial implantation in facial esthetic diseases: ultrasonography monitor follow-up. J Craniofac Surg. 2008;19(4):1098-103. [PubMed ID: 18650740]. https://doi.org/10.1097/SCS.0b013e3181763633.
-
17.
Wortsman X. Common applications of dermatologic sonography. J Ultrasound Med. 2012;31(1):97-111. [PubMed ID: 22215775].
-
18.
Kavoussi H, Ebrahimi A. Delayed gel indurations as an adverse effect of polyacrylamide filler and its easy treatment. Dermatol Res Pract. 2012;2012:539153. [PubMed ID: 23093956]. https://doi.org/10.1155/2012/539153.
-
19.
Wolter TP, Pallua N. Removal of the permanent filler polyacrylamide hydrogel (aquamid) is possible and easy even after several years. Plast Reconstr Surg. 2010;126(3):138-9. [PubMed ID: 20811192]. https://doi.org/10.1097/PRS.0b013e3181e3b506.