Abstract
Background:
Delivery is a physiological process that may cause neurophysiological changes in the lumbosacral region.Objectives:
The current study aimed to compare motor control of the lumbosacral region and pelvic floor muscle strength and performance in women with C-section and vaginal birth.Methods:
In this cross-sectional study, 120 prim parous women referring to healthcare centers in Karaj (Iran) during 2019 are studied. The participants were selected using convenience sampling. The motor control of the lumbosacral region was examined by four clinical tests (standing bent, active straight leg raising, bent knee fall out, and knee lift abdominal test) using a pressure biofeedback unit. Muscle strength and performance were measured using the Oxford scoring system and the PFPI-20 questionnaire, respectively. Data were analyzed using independent t-test, Mann-Whitney, and Chi-square tests. Statistical significance was considered when P value < 0.05.Results:
Based on the standing bent test, a significant difference was found between those in vaginal delivery and C-section groups (P = 0.011). Also, the mean scores of muscular strengths (P = 0.009) and pelvic floor muscular function (P = 0.01) in the vaginal delivery group were significantly higher than the C-section group.Conclusions:
the mean scores of pelvic floor motor control, pelvic floor muscular strength, and function in the C-section group were higher than those in the vaginal delivery group. This study demonstrated the necessity of postpartum pelvic floor muscle rehabilitation, especially in vaginal delivery.Keywords
Natural Childbirth Cesarean Section Pelvic Floor Fecal Incontinence Urinary Incontinence
1. Background
The human musculoskeletal system gives us the ability to move, which is mainly controlled by the central nervous system (CNS). The interconnected network of the CNS controls the stability and movements of the body (1). Motor control is defined as the ability to control the posture and movement for performing the daily activities, controlled by the CNS. Several studies have investigated motor control and its association with pain and musculoskeletal disorders (2-4). Based on the literature, musculoskeletal disorders like low back pain are associated with poor motor control of the pelvic floor muscles (5). It also seems that the acute and chronic pelvic floor pain is associated with changes in the morphology and behavior of a number of muscles such as multifidus, transverse abdominis, and deep trunk muscles (6).
Pelvic floor muscle health is important for women's overall health. Besides, disorders of pelvic floor muscle negatively influence women's quality of life (7). Pelvic floor muscles and their associated tissues support the pelvic organs and contribute to female sexual function, urinary and fecal control processes, and posture control (8). Pelvic floor muscles also contribute to proper lumbar muscle stability (9), which its proper function is necessary for pelvic girdle support. However, injuries may cause losing contractile ability (10). Several factors or mechanical stresses (e.g. pregnancy, childbirth, and endocrine events) may change the pelvic floor during the women's life cycle, which may, in turn, affect the urinary tract during pregnancy and childbirth. Pregnancy and childbirth appear to be major risk factors for developing pelvic floor disorders (11).
The pelvic floor muscle dysfunctions include problems in muscles such as fecal and urinary incontinence, pelvic organ prolapse, sexual disorders, and chronic pain syndromes. It seems that delivery is associated with decreased pelvic floor muscle strength (12). Nowadays, special attention is paying to the effects of different delivery modes on musculoskeletal (11, 13-15). One of the main consequences of C-section is postoperative complications caused by damage to abdominal muscles (16).
Based on the epidemiological data, compared to C-section, vaginal delivery is associated with an increased risk of urinary incontinence three to six months after delivery (14). However, the results on this issue are controversial. Some studies have considered urinary incontinence as a complaint that is associated with natural childbirth (17), while others did not find it (18). Also, there may be a significant difference between the two modes of delivery concerning the pelvic floor muscular strength. de Abreu's et al. (19) reported that weakness of pelvic floor muscles can cause low back pain among women. However, low back pain after C-section may affect the stability and quality of life in women, as some of them cannot even carry out their daily activities (20).
The pelvic floor muscles form the base of the abdominal cavity, and these muscles contract to maintain continuity and contribute to the increased intra-abdominal pressure during the different tasks. In healthy subjects, strong voluntary contraction of the abdominal muscles is accompanied by the contraction of pelvic floor muscle activity (8, 9). Therefore, pelvic floor muscles have a crucial role in the stabilization of the spine. Studies have shown that designing an exercise program for women before and during the second half of the pregnancy can reduce the risk of low back pain and other postpartum disorders (21).
It's well documented that both types of delivery are associated with changes in the lumbosacral region, due to the different interventions performed on the abdominal and pelvic floor muscles, which may negatively affect the function of these muscles and cause long-term consequences regarding motor control. To the best of the author's knowledge, no study is conducted on this issue so far.
2. Objectives
Therefore, the present study aimed to investigate whether pelvic floor motor control, muscular strength, and function in women with a history of C-section and vaginal delivery were different from each other or not?
3. Methods
In this cross-sectional study, 120 women referred to the stations affiliated to the selected healthcare centers in the western Alborz, Iran, during 2019 were recruited via convenience sampling. Based on a previous study (22), by using G*Power version 3.1, and considering α = 0.05 and β = 0.20 for independent t-test of pelvic floor muscle strength (C-section = 2.05 ± 0.58, vaginal delivery = 1.46 ± 0.53), the sample size was estimated as 24 subjects. To increase the validity of the study, the sample size was increased to 120.
Before performing the assessments, all subjects participated in a familiarization session. Informed written consent was obtained from all participants. Participants were ensured about the confidentiality of information. Also, they were informed that they can withdraw from the study at any time. After filling out the personal information form and the questionnaire related to the inclusion and exclusion criteria, the eligible subjects were identified. The inclusion criteria were being prim parous, being aged 18 to 35 years, at least one year between giving birth and getting pregnant again and being pregnant. The exclusion criteria were having a history of pelvic floor pain lasting more than 3 months, pelvic infection at the time of the study, lumbar and pelvic surgery except for C-section, diseases such as MS, diabetes, rheumatoid arthritis, heart disease, epilepsy, and curettage.
The height and weight of all subjects were measured using a standing scale and a Seca 700 caliper. The Persian version of Pelvic Floor Distress Inventory-20 (PFDI-20) was used to evaluate the pelvic floor muscle dysfunction. The PFDI-20, including pelvic organ prolapse, urinary incontinence, and fecal incontinence, was used. PFDI-20 consists of 20 items categorized in three subscales to detect the symptoms of the disease during the past three months: a) Pelvic Organ Prolapse Distress Inventory-6 (POPDI-6), b) Colorectal-Anal Distress Inventory 8 (CRADI-8), and c) Urinary Distress Inventory 6 (UDI-6). The subscales are considering independent scales (23). The Persian version of PFDI-20 was used in the present study, and its test-retest reliability fell between 68 and 71% (24).
Pressure biofeedback Unit(PBU) (Chattanooga stabilizer biofeedback (Australia)) device was used to evaluate the motor control of the lumbopelvic area (25). To assess motor control of the lumbopelvic area, the following four clinical tests were used: Active straight leg Raising (ASLR), Bent knee fall out (BKFO), Knee lift Abdominal test (KLAT), and Standing bent (SB). The intra-rater reliability of using PBU in the examination of motor control of the lumbosacral region was reported from good to excellent (Intra Class Correlation, 0-.60-0.95) (25). All of the abovementioned clinical tests were performed following a previous study (26).
Based on previous studies, the Oxford Grading Scale system was used to evaluate the pelvic floor muscular strength (19). The study protocol was approved by the Ethics Committee for biomedical research of the University of Social Welfare and Rehabilitation Sciences (ID: IR.USWR.REC.1398.005). The statistical analyses were performed using SPSS Version 20. The Kolmogorov-Smirnov test was used to evaluate the normal distribution of data. Independent t-test, Chi-square, and Mann-Whitney tests were used to analyze the data. Statistical significance was considered when P value < 0.05.
4. Results
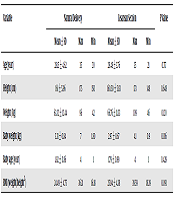
A total of 120 primiparous women participated in this study. The demographic characteristics of both groups, including age, height, weight, and age of the baby, birth weight, and body mass index, are presented in Table 1.
Demographic Characteristics of Participants (n=59 for the Vaginal Delivery Group and n=61 for the C-Section Group)
| Variable | Natural Delivery | Cesarean Section | P Value | ||||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Max | Min | Mean ± SD | Max | Min | ||
| Age(year) | 28.15 ± 4.62 | 35 | 20 | 28.48 ± 3.76 | 35 | 21 | 0.717 |
| Height (cm) | 161 ± 5.96 | 175 | 150 | 160.50 ± 5.83 | 173 | 148 | 0.648 |
| Weight (kg) | 63.32 ± 12.44 | 96 | 42 | 66.76 ± 11.33 | 109 | 46 | 0.120 |
| Baby weight (kg) | 3.31 ± 0.84 | 7 | 1.80 | 2.97 ± 0.67 | 4.1 | 0.9 | 0.016 |
| Baby age (year) | 1.92 ± 0.86 | 4 | 1 | 1.79 ± 0.99 | 4 | 1 | 0.429 |
| BMI (weight/height2) | 24.49 ± 4.75 | 36.31 | 16.18 | 25.94 ± 4.38 | 39.59 | 18.39 | 0.091 |
The results of the independent t-test showed no statistically significant difference between the two groups concerning the mean scores of the ASLR, BKFO, and KLAT (P > 0.05) (Table 2). But in the SB test, based on the results of the chi-square test, those in the vaginal delivery group had a significantly lower mean motor control score than those in the C-section group (value = 6.51, P = 0.011).
Results of the Independent t-test on Comparing the Lumbopelvic Motor Control in Women with a History of Vaginal Delivery or Cesarean Delivery
| Variable | Delivery | Mean ± SD | t | P Value |
|---|---|---|---|---|
| Active straight leg Raising | Natural | 46.18 ± 6.18 | 1.73 | 0.086 |
| C-section | 43.99 ± 7.59 | |||
| Knee lift Abdominal | Natural | 64.89 ± 14.90 | -0.20 | 0.840 |
| C-section | 65.53 ± 19.28 | |||
| Bent knee fall out | Natural | 53.77 ± 7.56 | 1.93 | 0.056 |
| C-section | 51.30 ± 6.57 |
The Mann-Whitney test revealed a significant difference between the vaginal delivery and C-section groups concerning the mean pelvic floor muscle function scores (P < 0.05) (Table 3).
The Results of the Mann-Whitney Test on Comparing Pelvic Floor Muscle Function in Women with a History of Vaginal Delivery or c-Section
| Variable | Delivery | Mean ± SD | Z | P Value |
|---|---|---|---|---|
| Pelvic Organ Prolapse Distress | Natural | 8.12 ± 9.89 | -2.118 | 0.034 |
| C-section | 5.42 ± 9.47 | |||
| Colorectal-Anal Distress | Natural | 8.20 ± 12.48 | -2.083 | 0.037 |
| C-section | 3.91 ± 7.86 | |||
| Urinary Distress | Natural | 14.23 ± 14.23 | 2.846 | 0.04 |
| C-section | 8.78 ± 15.66 | |||
| Pelvic Floor Distress | Natural | 30.57 ± 28.57 | -3.330 | 0.01 |
| C-section | 18.12 ± 27.81 |
Also, there was a significant difference between the two groups concerning the mean pelvic floor muscular strength scores (P = 0.009) (Table 4).
The Results of the Mann-Whitney Test on Comparing Pelvic Floor Muscular Strength Between the Two Groups
| Variable | Delivery | Number of participants in each grade | Z | P Value | |||||
|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | ||||
| Pelvic floor muscular strength | Natural | 0 | 3 | 16 | 20 | 16 | 4 | -2.630 | 0.009 |
| C-section | 0 | 3 | 6 | 17 | 28 | 7 | |||
5. Discussion
This study demonstrated a significant difference between the vaginal delivery and C-section groups concerning the mean scores of pelvic floor motor control in ASLR and SB tests, pelvic floor muscle function, and pelvic floor muscular strength.
Based on the findings, the motor control impairment score was higher in women with a history of vaginal delivery. Although no study to date has investigated this issue, our results are in agreement with those of previous studies on the association between pelvic floor motor control and LBP (27). In fact, normal postural control without feeling fatigued and pain indicates the proper utilization of the deep muscles that stabilize the body (28). Accordingly, in the present study, observed differences in the results of ASLR and SB tests between the two delivery modes may be associated with the mechanisms of improper spinal stabilization. During pregnancy, inserting a constant strain on the pelvic floor and abdominal muscles can alter the activity of the pelvic floor muscles, which may affect timely response and proper pattern regulating intra-abdominal pressure and spinal stabilization (28, 29). It seems that vaginal delivery increases the risk of major injuries to the pelvic floor muscles, compared to C-section; therefore, women with a history of vaginal delivery may show poorer motor control strategies. Hence, women with a history of vaginal delivery are at increased risk of low back pain. The results showed that pelvic organ prolapse, fecal and urinary incontinence symptoms, and total pelvic floor function scores were better in the C-section group than the vaginal delivery group. According to the findings, the rate of pelvic floor disorders in the vaginal delivery group was higher than the elective C-section group, which is consistent with the findings of previous studies (30, 31). In this regard, it was found that vaginal delivery is associated with pelvic floor disorders, and the C-section delivery has a protective effect on pelvic floor muscles compared to vaginal delivery (13, 32, 33). Pelvic floor muscles provide several functions that can be categorized into three categories: bladder control, participation in maintaining intra-abdominal pressure, and pelvic and abdominal organ support (34). The findings showed that in the C-section group, pelvic floor disorders were less common than the vaginal delivery group. These changes may be because of pelvic floor muscle injuries such as puborectalis injuries during labor, which can play an important role in supporting the pelvic diaphragm (35). On the other hand, a defect or weakness in pelvic floor muscles may lead to altered concurrent abdominal muscle activity as well as pelvic and respiratory problems (36). Considering these findings, it can be argued that women with a history of vaginal delivery are at increased risk of postpartum complications, which indicates the necessity of developing a comprehensive rehabilitation program. It's well proved that exercise after pregnancy may reduce the incidence of pelvic floor disorders (37).
Moreover, the results showed a significant difference between vaginal delivery and C-section groups concerning pelvic floor muscular strength. The pelvic floor muscles are rich in slow-twitch muscle fibers. Tonic contraction of the slow twitch-fibers protects the urinary tract and prevents excessive pressure on the connective tissues during routine activities in the standing position (38). The findings of this study also showed that pelvic floor muscles in the vaginal delivery group are weaker than those in the C-section group, which is consistent with the findings of previous studies (15, 22, 39). It seems that vaginal delivery may lead to postpartum injuries and reduced pelvic floor muscular strength (40). However, Li et al. found no association between urinary incontinence and pelvic floor muscular strength (41). Based on the results of this study and given that urinary incontinence in women may be a consequence of decreased pelvic floor muscular strength, an appropriate exercise regimen can greatly improve postpartum complications caused by muscle weakness.
The results of this study may be criticized in some ways. To assess pelvic floor muscular strength, tools like the perineometer are more accurate than Oxford scoring methods; therefore, the authors recommend using this tool in future studies to increase the validity of the findings. This was a cross-sectional study, and such a framework cannot be used to determine the possible associations between the aforementioned findings and future musculoskeletal disorders. Also, only women with a history of single childbirth were investigated in the present study. Therefore, the findings might not be generalizable to all delivery modes or women with multiple births. Finally, women who had a difficult vaginal delivery were excluded from the study, so the results may not be generalizable to these individuals. Moreover, the birth weight of children was higher in the C-section group than the vaginal delivery, so the results may have been affected by this variable.
In conclusion, this study demonstrated that women with a history of C-section had better pelvic floor motor control, muscular strength, and function scores than women with a history of vaginal delivery. Therefore, it seems that special attention should be paid to the health of the pelvic floor area after vaginal delivery.
Acknowledgements
References
-
1.
Murphy AC, Muldoon SF, Baker D, Lastowka A, Bennett B, Yang M, et al. Structure, function, and control of the human musculoskeletal network. PLoS Biol. 2018;16(1). e2002811. [PubMed ID: 29346370]. [PubMed Central ID: PMC5773011]. https://doi.org/10.1371/journal.pbio.2002811.
-
2.
Movahed M, Salavati M, Sheikhhoseini R, Arab AM, O'Sullivan K. Single leg landing kinematics in volleyball athletes: A comparison between athletes with and without active extension low back pain. J Bodyw Mov Ther. 2019;23(4):924-9. [PubMed ID: 31733784]. https://doi.org/10.1016/j.jbmt.2019.01.012.
-
3.
Sheikhhoseini R, Alizadeh M, Salavati M, O'Sullivan K, Shirzad E, Movahed M. Altered Lower Limb Kinematics during Jumping among Athletes with Persistent Low Back Pain. Annals of Applied Sport Science. 2018;6(2):23-30. https://doi.org/10.29252/aassjournal.6.2.23.
-
4.
Sheikhhoseini R, O'Sullivan K, Alizadeh MH, Sadeghisani M. Altered Motor Control in Athletes with Low Back Pain: a Literature Review. Annals of Applied Sport Science. 2016;4(4):43-50. https://doi.org/10.18869/acadpub.aassjournal.4.4.43.
-
5.
Hungerford B, Gilleard W, Hodges P. Evidence of altered lumbopelvic muscle recruitment in the presence of sacroiliac joint pain. Spine (Phila Pa 1976). 2003;28(14):1593-600. [PubMed ID: 12865851].
-
6.
Danneels LA, Vanderstraeten GG, Cambier DC, Witvrouw EE, De Cuyper HJ. CT imaging of trunk muscles in chronic low back pain patients and healthy control subjects. Eur Spine J. 2000;9(4):266-72. [PubMed ID: 11261613]. [PubMed Central ID: PMC3611341]. https://doi.org/10.1007/s005860000190.
-
7.
Oblasser C, McCourt C, Hanzal E, Christie J. Vibrating vaginal balls to improve pelvic floor muscle performance in women after childbirth: a protocol for a randomised controlled feasibility trial. J Adv Nurs. 2016;72(4):900-14. [PubMed ID: 26708615]. https://doi.org/10.1111/jan.12868.
-
8.
Hodges PW, Sapsford R, Pengel LH. Postural and respiratory functions of the pelvic floor muscles. Neurourol Urodyn. 2007;26(3):362-71. [PubMed ID: 17304528]. https://doi.org/10.1002/nau.20232.
-
9.
Sapsford RR, Hodges PW. Contraction of the pelvic floor muscles during abdominal maneuvers. Arch Phys Med Rehabil. 2001;82(8):1081-8. [PubMed ID: 11494188]. https://doi.org/10.1053/apmr.2001.24297.
-
10.
Hympanova L, Rynkevic R, Urbankova I, Blacher S, de Landsheere L, Mackova K, et al. Morphological and Functional Changes in the Vagina following Critical Lifespan Events in the Ewe. Gynecol Obstet Invest. 2019;84(4):360-8. [PubMed ID: 30636254]. https://doi.org/10.1159/000495348.
-
11.
Bozkurt M, Yumru AE, Sahin L. Pelvic floor dysfunction, and effects of pregnancy and mode of delivery on pelvic floor. Taiwan J Obstet Gynecol. 2014;53(4):452-8. [PubMed ID: 25510682]. https://doi.org/10.1016/j.tjog.2014.08.001.
-
12.
Huser M, Janku P, Hudecek R, Zbozinkova Z, Bursa M, Unzeitig V, et al. Pelvic floor dysfunction after vaginal and cesarean delivery among singleton primiparas. Int J Gynaecol Obstet. 2017;137(2):170-3. [PubMed ID: 28171703]. https://doi.org/10.1002/ijgo.12116.
-
13.
Blomquist JL, Munoz A, Carroll M, Handa VL. Association of Delivery Mode With Pelvic Floor Disorders After Childbirth. JAMA. 2018;320(23):2438-47. [PubMed ID: 30561480]. [PubMed Central ID: PMC6583632]. https://doi.org/10.1001/jama.2018.18315.
-
14.
Gregory KD, Jackson S, Korst L, Fridman M. Cesarean versus vaginal delivery: whose risks? Whose benefits? Am J Perinatol. 2012;29(1):7-18. [PubMed ID: 21833896]. https://doi.org/10.1055/s-0031-1285829.
-
15.
Hilde G, Staer-Jensen J, Siafarikas F, Engh ME, Braekken IH, Bo K. Impact of childbirth and mode of delivery on vaginal resting pressure and on pelvic floor muscle strength and endurance. Am J Obstet Gynecol. 2013;208(1):50 e1-7. [PubMed ID: 23103345]. https://doi.org/10.1016/j.ajog.2012.10.878.
-
16.
Cookson G, Laliotis I. Promoting normal birth and reducing caesarean section rates: An evaluation of the Rapid Improvement Programme. Health Econ. 2018;27(4):675-89. [PubMed ID: 29114977]. https://doi.org/10.1002/hec.3624.
-
17.
Hantoushzadeh S, Javadian P, Shariat M, Salmanian B, Ghazizadeh S, Aghssa M. Stress urinary incontinence: pre-pregnancy history and effects of mode of delivery on its postpartum persistency. Int Urogynecol J. 2011;22(6):651-5. [PubMed ID: 21125217]. https://doi.org/10.1007/s00192-010-1335-6.
-
18.
Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S, Norwegian ES. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med. 2003;348(10):900-7. [PubMed ID: 12621134]. https://doi.org/10.1056/NEJMoa021788.
-
19.
de Abreu DL, Rodrigues PTV, Amaral Corrêa L, Lacombe ADC, Andreotti D, Nogueira LAC. The relationship between urinary incontinence, pelvic floor muscle strength and lower abdominal muscle activation among women with low back pain. European Journal of Physiotherapy. 2018;21(1):2-7. https://doi.org/10.1080/21679169.2018.1435720.
-
20.
de Brito Cancado TO, Omais M, Ashmawi HA, Torres ML. Chronic pain after cesarean section. Influence of anesthetic/surgical technique and postoperative analgesia. Rev Bras Anestesiol. 2012;62(6):762-74. [PubMed ID: 23176985]. https://doi.org/10.1016/S0034-7094(12)70177-0.
-
21.
Garshasbi A, Faghih Zadeh S. The effect of exercise on the intensity of low back pain in pregnant women. Int J Gynaecol Obstet. 2005;88(3):271-5. [PubMed ID: 15733880]. https://doi.org/10.1016/j.ijgo.2004.12.001.
-
22.
Zhao Y, Zou L, Xiao M, Tang W, Niu HY, Qiao FY. Effect of different delivery modes on the short-term strength of the pelvic floor muscle in Chinese primipara. BMC Pregnancy Childbirth. 2018;18(1):275. [PubMed ID: 29970030]. [PubMed Central ID: PMC6029267]. https://doi.org/10.1186/s12884-018-1918-7.
-
23.
Spencer J, Hadden K, Brown H, Oliphant SS. Considering Low Health Literacy: How Do the Pelvic Floor Distress Inventory-Short Form 20 and Pelvic Floor Impact Questionnaire-Short Form 7 Measure Up? Female Pelvic Med Reconstr Surg. 2019;25(2):145-8. [PubMed ID: 30807417]. [PubMed Central ID: PMC6572727]. https://doi.org/10.1097/SPV.0000000000000672.
-
24.
Hakimi S, Hajebrahimi S, Bastani P, Aminian E, Ghana S, Mohammadi M. TRANSLATION AND VALIDATION OF THE PELVIC FLOOR DISTRESS INVENTORY SHORT FORM (PFDI-20), IRANIAN VERSION. BMJ Open. 2017;7(Suppl 1).
-
25.
Azevedo DC, Lauria AC, Pereira AR, Andrade GT, Ferreira ML, Ferreira PH, et al. Intraexaminer and interexaminer reliability of pressure biofeedback unit for assessing lumbopelvic stability during 6 lower limb movement tests. J Manipulative Physiol Ther. 2013;36(1):33-43. [PubMed ID: 23380212]. https://doi.org/10.1016/j.jmpt.2012.12.008.
-
26.
Roussel NA, Nijs J, Mottram S, Van Moorsel A, Truijen S, Stassijns G. Altered lumbopelvic movement control but not generalized joint hypermobility is associated with increased injury in dancers. A prospective study. Man Ther. 2009;14(6):630-5. [PubMed ID: 19179101]. https://doi.org/10.1016/j.math.2008.12.004.
-
27.
Tsang SMH, Szeto GPY, Li LMK, Wong DCM, Yip MMP, Lee RYW. The effects of bending speed on the lumbo-pelvic kinematics and movement pattern during forward bending in people with and without low back pain. BMC Musculoskelet Disord. 2017;18(1):157. [PubMed ID: 28415980]. [PubMed Central ID: PMC5392990]. https://doi.org/10.1186/s12891-017-1515-3.
-
28.
Comerford MJ, Mottram SL. Movement and stability dysfunction--contemporary developments. Man Ther. 2001;6(1):15-26. [PubMed ID: 11243905]. https://doi.org/10.1054/math.2000.0388.
-
29.
O'Sullivan P, Dankaerts W, Burnett A, Straker L, Bargon G, Moloney N, et al. Lumbopelvic kinematics and trunk muscle activity during sitting on stable and unstable surfaces. J Orthop Sports Phys Ther. 2006;36(1):19-25. [PubMed ID: 16494070]. https://doi.org/10.2519/jospt.2006.36.1.19.
-
30.
Lipschuetz M, Cohen SM, Liebergall-Wischnitzer M, Zbedat K, Hochner-Celnikier D, Lavy Y, et al. Degree of bother from pelvic floor dysfunction in women one year after first delivery. Eur J Obstet Gynecol Reprod Biol. 2015;191:90-4. [PubMed ID: 26103101]. https://doi.org/10.1016/j.ejogrb.2015.05.015.
-
31.
Handa VL, Blomquist JL, Knoepp LR, Hoskey KA, McDermott KC, Munoz A. Pelvic floor disorders 5-10 years after vaginal or cesarean childbirth. Obstet Gynecol. 2011;118(4):777-84. [PubMed ID: 21897313]. [PubMed Central ID: PMC3178744]. https://doi.org/10.1097/AOG.0b013e3182267f2f.
-
32.
Lukacz ES, Lawrence JM, Contreras R, Nager CW, Luber KM. Parity, mode of delivery, and pelvic floor disorders. Obstet Gynecol. 2006;107(6):1253-60. [PubMed ID: 16738149]. https://doi.org/10.1097/01.AOG.0000218096.54169.34.
-
33.
Larsson C, Hedberg CL, Lundgren E, Soderstrom L, TunOn K, Nordin P. Anal incontinence after caesarean and vaginal delivery in Sweden: a national population-based study. Lancet. 2019;393(10177):1233-9. [PubMed ID: 30799061]. https://doi.org/10.1016/S0140-6736(18)32002-6.
-
34.
Talasz H, Kofler M, Kalchschmid E, Pretterklieber M, Lechleitner M. Breathing with the pelvic floor? Correlation of pelvic floor muscle function and expiratory flows in healthy young nulliparous women. Int Urogynecol J. 2010;21(4):475-81. [PubMed ID: 19997721]. https://doi.org/10.1007/s00192-009-1060-1.
-
35.
Grob AT, Withagen MI, van de Waarsenburg MK, Schweitzer KJ, van der Vaart CH. Changes in the mean echogenicity and area of the puborectalis muscle during pregnancy and postpartum. Int Urogynecol J. 2016;27(6):895-901. [PubMed ID: 26676911]. [PubMed Central ID: PMC4879173]. https://doi.org/10.1007/s00192-015-2905-4.
-
36.
Iglesia CB, Smithling KR. Pelvic Organ Prolapse. Am Fam Physician. 2017;96(3):179-85. [PubMed ID: 28762694].
-
37.
Ussing A, Dahn I, Due U, Sorensen M, Petersen J, Bandholm T. Supervised pelvic floor muscle training versus attention-control massage treatment in patients with faecal incontinence: Statistical analysis plan for a randomised controlled trial. Contemp Clin Trials Commun. 2017;8:192-202. [PubMed ID: 29696209]. [PubMed Central ID: PMC5898528]. https://doi.org/10.1016/j.conctc.2017.07.006.
-
38.
Critchley HO, Dixon JS, Gosling JA. Comparative study of the periurethral and perianal parts of the human levator ani muscle. Urol Int. 1980;35(3):226-32. [PubMed ID: 6446182]. https://doi.org/10.1159/000280326.
-
39.
Van de Waarsenburg MK, van der Vaart CH, Withagen MIJ. Structural changes in puborectalis muscle after vaginal delivery. Ultrasound Obstet Gynecol. 2019;53(2):256-61. [PubMed ID: 29947067]. https://doi.org/10.1002/uog.19170.
-
40.
Bailey PE, van Roosmalen J, Mola G, Evans C, de Bernis L, Dao B. Assisted vaginal delivery in low and middle income countries: an overview. BJOG. 2017;124(9):1335-44. [PubMed ID: 28139878]. https://doi.org/10.1111/1471-0528.14477.
-
41.
Li H, Wu RF, Qi F, Xiao AM, Ma Z, Hu Y, et al. Postpartum pelvic floor function performance after two different modes of delivery. Genet Mol Res. 2015;14(2):2994-3001. [PubMed ID: 25966063]. https://doi.org/10.4238/2015.April.10.9.