Abstract
Background:
Pain after surgery is highly inevitable, and the use of nonsteroidal anti-inflammatory drugs (NSAIDs) has been reported with side effects.Objectives:
This study evaluated the effectiveness of transcutaneous electrical nerve stimulation (TENS) on pain intensity and disability of patients who underwent hip arthroplasty.Methods:
A purposive sampling technique was used to recruit 56 subjects that underwent hip arthroplasty. They were randomly allocated to the TENS group (TG) and control group (CG) equally. The subjects in the TG group were treated with conventional TENS twice a day for three weeks, but the CG group was treated with normal drugs only. Pain intensity and hip disability were measured in both groups with the Visual Analogue scale (VAS) and Oxford hip score before the treatment and after the intervention, respectively.Results:
The results showed that there was a significant reduction between the pre-treatment and post-treatment pain intensity (t = 3.83, P = 0.003) and hip disability (t = -4.45, P < 0.001) in the TG group. A significant reduction was also observed in pain intensity (t = 3.16, P = 0.01) and hip disability (t = -6.71, P = 0.000) between the pre-treatment and post-treatment periods in the CG group. There was a significant reduction in post-treatment pain intensity (t = 10, P = 0.000) and hip disability (t = -3.51, P = 0.006) when the TG group was compared with the CG group.Conclusions:
TENS was effective in the management of acute post-surgical pain and disability of patients with hip arthroplasty.Keywords
1. Background
There has been a continuous increase in hip and knee replacement surgeries with a record of an upsurge in the total percentage of patients with total hip arthroplasties among patients less than 60 years of age (1). The procedure can be total arthroplasty or a hemiarthroplasty (partial joint replacement) to relieve pain, improve mobility, and provide freedom to perform activities of daily living (2). Discomfort, pain, and restlessness have been reported as the aftermath of anesthesia and surgery, which could have been caused by incision (3). In addition, reawakening of the patient from anesthesia and relieve of pain are very significant in the postoperative care of the patient that have just undergone operation (3). The management of postoperative pain consists of pharmacological and non-pharmacological methods. Pharmacological methods include balanced (multimodal) analgesia, opioids, non-opioids, adjuvants, and regional analgesia (4). Non-pharmacological modalities include acupuncture, physical therapy, and relaxation therapy. There was a misconception that no matter the severity of pain, opioid analgesics can effectively abase it (5). However, studies have reported that a large percentage of postoperative pain was undertreated (6, 7).
Physical therapy management of pain includes transcutaneous electrical nerve stimulation (TENS), cryotherapy, acupuncture, heat therapy, and pulsed electromagnetic field (PEMF) therapy. In fact, TENS is a small portable device that transmits low voltage electrical impulses through the electrode and the skin to the body. It is cheap and involves no blood or opening of the patient's body with no undesirable effects compared to pharmacologic pain-relieving drugs. It is widely used in the relief of pain, but its efficacy in the relief of acute postoperative pain has not been established (8).
The treatment of post-surgical pain is multimodal, which involves a series of nonsteroidal anti-inflammatory drugs (NSAIDs) and selective cyclooxygenase-2 (COX-2) inhibitors (Coxibs). Research has shown that coxibs were associated with increased risks of myocardial infarction compared with placebo (9). Literature has established a series of side effects such as gastrointestinal, cardiovascular, and renal complications upon the usage of NSAIDs (10). In a study by Golladay et al. (11) on the oral multimodal analgesia for total joint arthroplasty, they concluded that the primary outcomes on the usage of oral medication are to reduce the consumption of opioids, minimize side effects, and prevent chronic pain, which can positively affect long-term outcomes.
Various studies have highlighted that TENS is helpful in the treatment of post operational pain. A study by Bennet et al. (12) reported that the inconclusiveness in the findings of TENS may be due to methodical fault, poor assessment outcomes, and inadequacy of TENS intervention. In the study of Lan et al. (13) in patients with hip arthroplasty, they found no great change in the intensity of pain. Also, the study by Unterrainer et al. (14) using TENS for patients with spinal surgeries revealed a reduction in pain on activity only. In the study of Solak et al. (15) on pain management among post-thoracotomy patients using TENS, they reported pain reduction in the first 3 days post-thoracotomy, which is comparable to patient-controlled analgesia. Based on these reports, there was no agreement on the efficacy of TENS in the management of postoperative pain. Moreover, there are a lot of side effects upon the usage of NSAIDs.
2. Objectives
This study was, therefore, designed to investigate whether electrical stimulation would have any effect on the treatment of postoperative hip arthroplasty pain intensity and hip disability to complement the usage of NSAIDs.
3. Methods
3.1. Ethical Approval
The research protocol was approved (ERC/2017/12/04) by the Ethics and Research Committee of the OAUTHC, Ile Ife, Nigeria.
3.2. Subjects
The subjects that participated in this study were just concluded post-surgical in-patients with hip arthroplasty admitted to the Teaching Hospitals Complex of the Obafemi Awolowo University (OAUTHC), Ile-Ife.
The inclusion and exclusion criteria: patients that were recruited for the study were those who underwent operation of the hip joint and without any other comorbidity. Patients with the operation but have another comorbidity such as diabetes, peripheral neuropathy, renal issues, and patients with post-surgery thrombophlebitis were excluded from the study.
3.2.1. Sampling Technique
A purposive sampling technique was used to recruit subjects for this study. The number of patients used for the study was calculated by the following formula (16):
where Ζα∕2 represents the critical value of the normal distribution at α∕2. (i.e., for a confidence level of 95%, α is 0.05, and the critical value is 1,96), Ζ1–β represents the critical value of the typical distribution at 1-β (i.e., for a power of 80%, β is 0.2, and the critical value is 0.84), µ1 and µ2 are means from 2 independent groups = Δ. δ is the effect size, which is the standardized difference and equal to the absolute difference (Δ) divided by the standard deviation (σ). Thus, n (size per group) = 25 for a group (16). However, 28 subjects were recruited per group with respect to attrition; thus, 56 individuals were considered.
3.2.2. Consent From the Patient
A copy of the consent form was provided for each subject. For those that did not understand the English language, the content of the consent was interpreted into the Yoruba language for a better understanding. Each subject then signed the form before the commencement of the study.
3.3. Research Design
3.3.1. Instruments
The instruments used in this study were as follows:
i) A TENS unit (MH6000 Combo, MH6100 EMS, MH6200 TENS) manufactured by Medihightec Medical Co., LTD, Taiwan. A small handheld battery-powered device was used to generate low-voltage electrical impulses to excite the sensory nerves.
ii) Pre-gelled, self-adhesive electrodes (a square-shaped 40 by 40 MM produced by Civarc Ltd, Lagos) that transmitted the impulses to the area of the body.
iii) Cotton wool and methylated spirit for skin toileting of the area of skin the electrode was placed.
iv) Visual Analog Scale (VAS): A long flat plastic that consists of 100 mm scale that marked from 0 in the left, representing no feeling of pain, and finished by 100 mm in the right, standing for excruciating pain. It is used to assess pain intensity. Values that are more than 70 mm mean very severe pain, where value 45 - 54 means moderate pain, 35 - 45 represents mild pain and no pain is represented by 0 to 5. The VAS was validated with VRS by Williamson and Hoggart (17) who concluded that VRS provides a useful alternative to the VAS scores in the assessment of chronic pain. Bijur et al. (18) found a significant correlation between the VAS and the Numerical Rating Scale (r = 0.94, 95% CI = 0.93 to 0.95). They also found that the slope of the regression line was 1.01 (95% CI = 0.97 to 1.06), indicating a strong level of agreement between the two tools. The VAS was used to measure the present pain intensity.
v) Oxford Hip Score (OHS): Considering OHS, there are 12-items for which patients should report the outcome measure. It was designed to assess disability after surgery to the hip. There was an allocation of 0 - 4 to each item of the questionnaire. Four represents the best outcomes for a question. Accordingly, there will be a maximum of 48 points and a minimum of 0 points for the questionnaire. Forty-eight is the best outcome, values that results greater than 41 are considered excellent or outstanding; 34 - 41 are good, 27 - 33 are fair, and < 27 are poor. The inter-rater/intra-rater reliability = 0.679, construct validity between OHS and Harris hip score is Spearman’s p = -0.712. The validity and responsiveness of the OHS was reported by Uesugi et al. (19).
3.4. Site of Experiment
All interventions were performed at the Orthopedics ward, Teaching Hospitals Complex of the Obafemi Awolowo University (OAUTHC), Ile-Ife, Nigeria.
3.4.1. Randomization
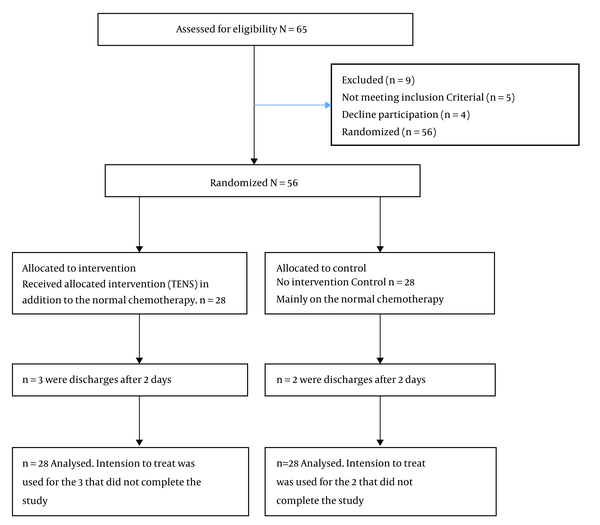
Subjects were allocated to two groups randomly. The fishbowl method was used for the allocation. Here, 56 pieces of paper were wrapped in an envelope with an inscription TENS and control of equal number. Once a patient was found eligible for the treatment, he/she would pick up a paper from the envelope. The patient was then allocated to the related group. In this regard, there were two groups of patients, the TENS group, which consisted of 28 patients, and likewise the control group, which consisted of 28 patients. The patient flow chart and randomization of subjects are shown in Figure 1.
Consort diagram of random allocation of the subjects to the two groups
3.5. Procedure
Before the treatment, the bio-data of each subject was collected. A brief interview was conducted before the intervention to find out the type of surgery, pain intensity, and functional limitation. The consent was obtained before the commencement of the treatment.
3.5.1. TENS Group
To apply the electrodes for the application of TENS, a tape rule was used to measure 5 cm away from the incision site, the marked place was thoroughly cleaned with a piece of methylated soaked cotton wool. The self-adhesive pre-gelled electrode was then applied. TENS unit was adjusted to the bearable mode for the patients. TENS was put on, with intensity of 100 μs and frequency of 100 Hz; the treatment was for 15 minutes. In addition to each patient’s routine analgesic and antibiotics, TENS was also applied twice a day for three weeks. The whole treatment lasted for three weeks for each patient. The patients underwent 20 treatment sessions before discharge.
3.5.2. Control Group
The patients received their normal analgesics and antibiotics only. There was no application of TENS.
3.6. Outcome Measures
3.6.1. Pain Intensity
Pain intensity was measured with VAS. Each patient was educated on how to place the finger on the scale that represents the severity of the pain. Zero is no pain, and 100 mm is the maximum or excruciating pain. This was done before the treatment and after the treatment on each session, three days for each patient in the TENS group. In the control group, VAS was administered on the first day that patient got back to the ward, and the last day before discharge.
3.6.2. Hip Disability
Oxford hip score (OHS) was used to measure hip disability. The OHS was administered at the same time the VAS was administered for the TENS and control groups.
3.7. Data Analysis
Data were analyzed using descriptive and inferential statistics. Dependent t-test was used to compare the pre-treatment and post-treatment pain intensity and hip disability within the groups. Moreover, an independent t-test was used to compare the outcome measures between the groups. A P value of less than 0.05 was considered statistically significant.
4. Results
4.1. Socio-Demographic Characteristics of the TEN Group and the Age Range of All Subjects
The socio-demographic characteristics of the subjects in the two groups are shown in Table 1. There were nine (33.3%) males and nineteen (66.7%) females in each group. Nineteen (66.7%) subjects had primary education, and nine (33.3%) had secondary education in the TENS group, but All 28 (100%) subjects had secondary education in the control group. The mean age of all subjects was 57.67 years.
Socio-Demographic Characteristics of the Subjects (N = 56)
| Variables | TENS Group (n = 28) | Control Group (n = 28) |
|---|---|---|
| Age, mean ± SD (min-max) | 57.67 ± 13.75 (40 - 68) | 57.67 ± 13.75 (42 - 66) |
| Sex, F (%) | ||
| Male | 9 (33.3) | 9 (33.3) |
| Female | 19 (66.7) | 19 (66.7) |
| Educational level, F (%) | ||
| Primary | 19 (66.7) | 0 (0) |
| Secondary | 9 (33.3) | 28 (100) |
4.2. Comparison Between the TENS and Control Groups
The comparison between pre- and post-treatment pain intensity and hip outcome measures for the experimental and control groups are shown in Table 2. There was a significant difference between the pain intensity (t = 10, P = 0.00) of the TENS and control groups. There was a significant difference between the hip outcome measure (t = -3.51, P = 0.006) of the TENS and control group. There was also a significant difference in the post-treatment pain intensity between the experimental and control groups. Furthermore, there was a significant difference in the hip outcome measure post-treatment.
| Outcomes | TENS Group (N = 28) | Control Group (N = 28) | Between Groups | |
|---|---|---|---|---|
| t | P Value | |||
| Pain intensity (VAS) | ||||
| Pre-treatment | 4.00 ± 0.89 | 4.33 ± 0.52 | 0.791 | 0.0448 |
| Post-treatment | 2.00 ± 0.89 | 3.00 ± 0.89 | 10.00 | 0.000 |
| Within Groups, t (P value) | 3.83 (0.003) | 3.16 (0.01) | ||
| Hip disability (HOS) | ||||
| Pre-treatment | 10.67 ± 1.86 | 8.67 ± 1.03 | 1.000 | 0.076 |
| Post-treatment | 18.00 ± 3.58 | 12.66 ± 1.03 | -3.508 | 0.006 |
| Within Groups, t (P value) | -4.45 (0.001) | -6.71 (0.00) | ||
5. Discussion
This study evaluated the effect of TENS on acute postoperative pain intensity in hip arthroplasty patients. In this study, women were more than men. This indicated that there may be more women with hip problems than men. The increase in hip problems in women could be attributed to osteoporosis, incontinence, and frailty, which is common in postmenopausal women (20). If there is an accidental fall, that is common in older individuals, there is a tendency to fracture the neck of the femur. Osteoporosis usually leads to bone fragility, which makes the patient susceptible to fracture. This may be attributed to low bone mass and microarchitectural deterioration of bone tissue (21). To recognize osteoporosis in a clinically setting, low-energy trauma will easily lead to a fracture, which is commonly found in the hip, vertebrae, and distal forearm (22). Osteoporosis has been reported to be common among individuals of 50 years; (women 5% and men 2.4%), for 50 to 85 years, it has increased to 50% for women and 20% for men (23).
The study indicated that post-treatment pain intensity was less than pre-treatment pain intensity, as well as pre-treatment hip outcome measure in the TENS group was higher than the control group. This indicates that TENS is effective in the treatment of acute postoperative pain in hip arthroplasty. The mechanism of the effect of TENS on pain intensity of primary hip arthroplasty is based on the pain gate theory, which explains how the transmission of the noxious stimulus from the C fibers in the spinal cord and to the higher centers is reduced after the excitation of A beta (Aβ) sensory fibers; thus, the stimulus of the pain cannot go through to the higher center and pain is relieved (24). The use of TENS and sterile electrodes around the incision was first used by Hymes et al. (25), who first reported the success of conventional TENS for acute post-surgical pain. In their study, which lasted for 4 to 5 days after surgery in which 115 patients were continuously or intermittently stimulated, there was a report of an 80% reduction in the intensity of pain. Adverse effects of concurrent opioid consumption and associated respiratory depression can be relieved using TENS. Reeve et al. (26), in their report in a systematic review on postoperative and acute pain, showed that 12 of 20 randomized control trials concluded that TENS might be of certain benefit to relieve acute and postoperative pain. This was consistent with the present study.
The current study further indicated that there was a significant reduction in pain intensity as well as an increase in hip outcome measures in the control group. It is noteworthy that these subjects were on pharmacological treatment throughout this period, which would enhance pain relief as well as wound healing. This is responsible for the reduction. The use of systemic analgesics, narcotics, and related drugs, as well as regional analgesia, can prevent patients from long-acting local anesthetics and can make patients feel free of pain (27).
Comparing the experimental and control groups' pain intensity and hip outcome measures, the study showed that there was significant pain reduction in the TENS group compared to the control group. Furthermore, there was a significant increase in hip outcome measures in the TENS group compared to the control group. Johnson (28), in their systematic review, documented that transcutaneous electrical nerve stimulation is a non-invasive, inexpensive, self-administered technique to relieve pain. The conventional TENS is used to selectively activate large-diameter non-noxious afferents (A-beta) to reduce nociceptor cell activity and sensitization at a segmental level in the central nervous system. Pain relief with conventional TENS is rapid in onset and offset and is maximal when the patient experiences strong but non-painful paranesthesia beneath the electrodes. Clinical experience suggests that TENS may be beneficial as an adjunct to pharmacotherapy for acute pain; however, systematic reviews are conflicting (28). Literature has also shown that the effects of TENS are mediated via a series of neurochemicals such as opioids, serotonin, acetylcholine, noradrenaline, and gamma-aminobutyric acid (GABA) (29). There has been the involvement of 5-HT2 and 5-HT3 receptors as well as mu-opioid in low-frequency TENS, but high-frequency TENS has been shown to involve delta-opioid receptors and reduce aspartate and glutamate levels in the spinal cord (29).
The cost of surgery and hospitalization eventually should be hypothetically reduced according to the report by Hymes et al. (25), who declared that TENS reduced the incidence of postoperative atelectasis, invariably reduced the length of stay in a postoperative intensive care unit (ICU). However, studies by Cooperman et a1. (30) and Rosenberg et a1. (31) were in contrast to our findings. Transcutaneous electrical nerve stimulation has been reported to have some modifications on pain-induced, decreases vital capacity, functional residual capacity, and arterial oxygen tension; therefore, postoperative pulmonary morbidity decreases, while postoperative pulmonary function increases. This study demonstrated that pain related to musculoskeletal trauma can be effectively modulated by TENS. There is something to the use of TENS that makes it attractive. In addition to the fact that it eliminates postoperative pain, there is no known side effect. This demonstrates that TENS is significantly effective in the treatment of acute postoperative pain in hip arthroplasty.
5.1. Conclusions
There was a significant difference between the pain intensity pre-treatment and post-treatment with TENS. This implies that TENS is effective in acute postoperative pain in patients with hip arthroplasty.
5.2. Recommendation
The use of Transcutaneous Electrical Nerve Stimulation (TENS) has been proven to be effective in the management of hip arthroplasty with no side effects.
5.3. Limitations
The study did not do the follow-up of the patients after discharge from the hospital. This can be a limitation in the sense that the sustenance of the relief of pain and the maintenance of the improvement of the disability may not be ascertained after the discharge.
References
-
1.
Liu X, Zi Y, Xiang L, Wang Y. Total hip arthroplasty: areview of advances, advantages and limitations. Int J Clin Exp Med. 2015;8(1):27.
-
2.
Seidlitz C, Kip M. Introduction to the indications and procedures. In: Bless HH, Kip M, editors. White Paper on Joint Replacement: Status of Hip and Knee Arthroplasty Care in Germany. Berlin (Germany); 2018. p. 1-14. eng. https://doi.org/10.1007/978-3-662-55918-5_1.
-
3.
Ramsay MA. Acute postoperative pain management. Proc (Bayl Univ Med Cent). 2000;13(3):244-7. [PubMed ID: 16389390]. [PubMed Central ID: PMC1317048]. https://doi.org/10.1080/08998280.2000.11927683.
-
4.
Schug SA, Palmer GM, Scott DA, Halliwell R, Trinca J. Acute pain management: scientific evidence. Melbourne; 2015.
-
5.
Fields HL. The doctor's dilemma: opiate analgesics and chronic pain. Neuron. 2011;69(4):591-4. [PubMed ID: 21338871]. [PubMed Central ID: PMC3073133]. https://doi.org/10.1016/j.neuron.2011.02.001.
-
6.
Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003;97(2):534-40. table of contents. [PubMed ID: 12873949]. https://doi.org/10.1213/01.ane.0000068822.10113.9e.
-
7.
Huang N, Cunningham F, Laurito CE, Chen C. Can we do better with postoperative pain management? Am J Surg. 2001;182(5):440-8. https://doi.org/10.1016/s0002-9610(01)00766-8.
-
8.
Kerai S, Saxena KN, Taneja B, Sehrawat L. Role of transcutaneous electrical nerve stimulation in post-operative analgesia. Indian J Anaesth. 2014;58(4):388-93. [PubMed ID: 25197104]. [PubMed Central ID: PMC4155281]. https://doi.org/10.4103/0019-5049.138966.
-
9.
Chen LC, Ashcroft DM. Risk of myocardial infarction associated with selective COX-2 inhibitors: meta-analysis of randomised controlled trials. Pharmacoepidemiol Drug Saf. 2007;16(7):762-72. [PubMed ID: 17457957]. https://doi.org/10.1002/pds.1409.
-
10.
Harirforoosh S, Asghar W, Jamali F. Adverse effects of nonsteroidal antiinflammatory drugs: an update of gastrointestinal, cardiovascular and renal complications. J Pharm Pharm Sci. 2013;16(5):821-47. [PubMed ID: 24393558]. https://doi.org/10.18433/j3vw2f.
-
11.
Golladay GJ, Balch KR, Dalury DF, Satpathy J, Jiranek WA. Oral multimodal analgesia for total joint arthroplasty. J Arthroplasty. 2017;32(9S):S69-73. [PubMed ID: 28705543]. https://doi.org/10.1016/j.arth.2017.05.002.
-
12.
Bennett MI, Hughes N, Johnson MI. Methodological quality in randomised controlled trials of transcutaneous electric nerve stimulation for pain: low fidelity may explain negative findings. Pain. 2011;152(6):1226-32. [PubMed ID: 21435786]. https://doi.org/10.1016/j.pain.2010.12.009.
-
13.
Lan F, Ma YH, Xue JX, Wang TL, Ma DQ. Transcutaneous electrical nerve stimulation on acupoints reduces fentanyl requirement for postoperative pain relief after total hip arthroplasty in elderly patients. Minerva anestesiologica. 2012;78(8):887.
-
14.
Unterrainer AF, Friedrich C, Krenn MH, Piotrowski WP, Golaszewski SM, Hitzl W. Postoperative and preincisional electrical nerve stimulation TENS reduce postoperative opioid requirement after major spinal surgery. J Neurosurg Anesthesiol. 2010;22(1):1-5. [PubMed ID: 19779370]. https://doi.org/10.1097/ANA.0b013e3181b7fef5.
-
15.
Solak O, Turna A, Pekcolaklar A, Metin M, Sayar A, Solak O, et al. Transcutaneous electric nerve stimulation for the treatment of postthoracotomy pain: a randomized prospective study. Thorac Cardiovasc Surg. 2007;55(3):182-5. [PubMed ID: 17410506]. https://doi.org/10.1055/s-2006-924631.
-
16.
Singh AS, Masuku MB. Sampling techniques & determination of sample size in applied statistics research: An overview. Int J Economics Commerce Manag. 2014;II(11):1-22.
-
17.
Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14(7):798-804. [PubMed ID: 16000093]. https://doi.org/10.1111/j.1365-2702.2005.01121.x.
-
18.
Bijur PE, Latimer CT, Gallagher EJ. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad Emerg Med. 2003;10(4):390-2. [PubMed ID: 12670856]. https://doi.org/10.1111/j.1553-2712.2003.tb01355.x.
-
19.
Uesugi Y, Makimoto K, Fujita K, Nishii T, Sakai T, Sugano N. Validity and responsiveness of the Oxford hip score in a prospective study with Japanese total hip arthroplasty patients. J Orthop Sci. 2009;14(1):35-9. [PubMed ID: 19214685]. https://doi.org/10.1007/s00776-008-1292-9.
-
20.
DuBeau CE, Kuchel GA, Johnson T2, Palmer MH, Wagg A, Fourth International Consultation on I. Incontinence in the frail elderly: report from the 4th International Consultation on Incontinence. Neurourol Urodyn. 2010;29(1):165-78. [PubMed ID: 20025027]. https://doi.org/10.1002/nau.20842.
-
21.
Curtis EM, Moon RJ, Harvey NC, Cooper C. Reprint of: The impact of fragility fracture and approaches to osteoporosis risk assessment worldwide. Int J Orthop Trauma Nurs. 2017;26:7-17. [PubMed ID: 28578992]. [PubMed Central ID: PMC5480618]. https://doi.org/10.1016/j.ijotn.2017.04.004.
-
22.
Yoo JH, Moon SH, Ha YC, Lee DY, Gong HS, Park SY, et al. Osteoporotic fracture: 2015 position statement of the korean society for bone and mineral research. J Bone Metab. 2015;22(4):175-81. [PubMed ID: 26713308]. [PubMed Central ID: PMC4691591]. https://doi.org/10.11005/jbm.2015.22.4.175.
-
23.
Pinheiro MM, Reis Neto ET, Machado FS, Omura F, Yang JH, Szejnfeld J, et al. Risk factors for osteoporotic fractures and low bone density in pre and postmenopausal women. Rev Saude Publica. 2010;44(3):479-85. [PubMed ID: 20549019]. https://doi.org/10.1590/s0034-89102010000300011.
-
24.
Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150(3699):971-9. [PubMed ID: 5320816]. https://doi.org/10.1126/science.150.3699.971.
-
25.
Hymes AC, Raab DE, Yonehiro EG, Nelson GD, Printy AL. Acute pain control by electrostimulation: a preliminary report. Advances in neurology. 1974;4:761-7.
-
26.
Reeve J, Menon D, Corabian P. Transcutaneous electrical nerve stimulation (TENS): a technology assessment. Int J Technol Assess Health Care. 1996;12(2):299-324. [PubMed ID: 8707503]. https://doi.org/10.1017/s026646230000965x.
-
27.
Abdolrazaghnejad A, Banaie M, Tavakoli N, Safdari M, Rajabpour-Sanati A. Pain management in the emergency department: a review article on options and methods. Adv J Emerg Med. 2018;2(4).
-
28.
Johnson M. Transcutaneous electrical nerve stimulation: Mechanisms, clinical application and evidence. Rev Pain. 2007;1(1):7-11. [PubMed ID: 26526976]. [PubMed Central ID: PMC4589923]. https://doi.org/10.1177/204946370700100103.
-
29.
Sluka KA, Vance CG, Lisi TL. High-frequency, but not low-frequency, transcutaneous electrical nerve stimulation reduces aspartate and glutamate release in the spinal cord dorsal horn. J Neurochem. 2005;95(6):1794-801. [PubMed ID: 16236028]. https://doi.org/10.1111/j.1471-4159.2005.03511.x.
-
30.
Cooperman AM, Hall B, Mikalacki K, Hardy R, Sadar E. Use of transcutaneous electrical stimulation in the control of postoperative pain. Am J Surg. 1977;133(2):185-7. https://doi.org/10.1016/0002-9610(77)90077-0.
-
31.
Rosenberg M, Curtis L, Bourke DL. Transcutaneous electrical nerve stimulation for the relief of postoperative pain. Pain. 1978;5(2):129-33. https://doi.org/10.1016/0304-3959(78)90034-9.
