Abstract
Background:
Moyamoya disease (MMD) is a chronic steno-occlusive cerebrovascular condition initially described in 1957 in a Japanese patient. The classic angiographic findings include bilateral stenosis or occlusion at the terminal portion of the internal carotid artery, with an abnormal vascular network at the base of the brain. There are few epidemiological descriptions of non-Asian cases.Objectives:
This study aimed at evaluating a cohort of patients with the MMD admitted in a quaternary, open-access rehabilitation hospital in central Brazil.Methods:
This was a retrospective, observational study. Two neurologists reviewed data from electronic records of patients with MMD admitted to SARAH Hospital in Brasilia in the past sixteen years. Data on etiology, associated conditions and general characteristics were collected. The modified Rankim scale (mRS) was used to determine morbidity.Results:
Twenty-one patients were identified and selected for this research. The average age at presentation was 20.5 years (range: 0 - 69 years), 62% were females, and 43% reported Asian ancestry. Ischemic stroke (IS) occurred in 95%, hemorrhagic stroke (HS) in 19%, and both IS and HS in 14%. Stroke recurred in 76% during follow-up; of these, 87% had IS. Because no other associated condition was found, 80% of the patients could be classified as MMD; 15% had the Moyamoya syndrome, with the presence of other conditions associated with the disease. Our hospital-based study showed a lower average age of onset than that in the literature, a much higher incidence of IS, and similar rates of HS. Patients with HS scored worse on an initial and final mRS, and surgical procedures did not significantly alter the prognosis. In comparison with those reported in international literature, we did not find significant differences in disability rates between younger and older patients. The average mRS score at admission was 3.4 (range: 2 - 4), with 2.9 (range: 1 - 4) at discharge.Conclusions:
Rehabilitation was able to improve the quality of life, as shown by the mRS at admission and discharge. Patients with HS tended to have worse outcomes.Keywords
1. Introduction
Moyamoya disease (MMD) is a chronic steno-occlusive cerebrovascular condition initially described in 1957 in a Japanese patient (1). The classic angiographic findings include bilateral stenosis or occlusion at the terminal portion of the internal carotid artery, with an abnormal vascular network at the base of the brain (2, 3).
Most epidemiological studies of this condition have been conducted in Asian countries, mainly Japan and Korea (4). The prevalence is estimated at 6.03/100 000 (5). There have been few studies in Latin American populations; one study in Brazil reported only 16 cases (6). The last epidemiological report for Brazil was a case series published in 2009 (7), and described surgical treatment in children. Only case reports so far have been conducted in a rehabilitation setting, with evaluation of prognosis or the effect of a multidisciplinary approach (8). For this study, we focused on the results and experience of follow-up of patients with MMD and stroke in our rehabilitation hospital. Because this is a rare disease with few descriptions in Western countries, the results of our work could add to the epidemiological data and possible differences between populations studied so far.
2. Objectives
The aim of the present study was to evaluate a cohort of patients with MMD managed and admitted in a quaternary, open-access rehabilitation hospital in central Brazil, and to analyze the most frequent neurological symptoms, associated conditions, duration of follow-up, and quality of life at admission and discharge.
3. Methods
In this retrospective, observational study, two neurologists reviewed data from electronic records of patients with MMD admitted to SARAH hospital in Brasilia in the past sixteen years. All patients were admitted due to stroke. Epidemiological information was collected and frequencies were analyzed.
The diagnostic criteria adopted were from the Japanese ministry of health and welfare (2). We divided patients into a group with the Moyamoya syndrome, when an associated condition (such as sickle cell disease) was identified, and a group with MMD, when no other condition was found. Patients not meeting the diagnostic criteria and those without confirmation of stroke (hemorrhagic, ischemic or both) by neuroimaging were excluded from the study.
For the quality of life assessment, we used the modified Rankin score (mRS). This is a classic score of morbidity used in most stroke trials, ranging from zero (absence of sequelae) to six (death) (9). Both neurologists independently analyzed the blinded information at admission and discharge. Any differences were discussed after data collection to achieve consensus. All patients with the diagnosis criteria for MMD and presence of stroke were evaluated (21 in total).
For statistical analysis, SPSS IBM® version 23 was used. Categorical data were presented as numbers or percentages and continuous data as means or medians. The hospital ethics committee approved this research, according to Brazilian regulations.
4. Results
Twenty-one patients were identified and selected for this research. The average age at presentation was 20.5 years (range: 0 - 69 years), and 62% were females. Admission to our rehabilitation service occurred at a mean of 1.5 years after a stroke, and there was a mean of 7.9 years of follow-up (range: 1 - 34 years); 42% of the patients were under 18 years at the time of the stroke. Table 1 summarizes the data on presentation, recurrence, follow-up, and mRS scores.
Population Characteristics
| Minimum | Maximum | Mean | |
|---|---|---|---|
| Age at stroke, y | 0 | 69 | 20.57 |
| Recurrence, mo | 0 | 120 | 11.06 |
| Initial mRs | 2 | 5 | 3.24 |
| Final mRS | 1 | 5 | 2.90 |
| Follow-up | 1 | 34 | 7.90 |
Patients mainly came from central regions of Brazil, and 43% reported Asian ancestry. Ischemic stroke (IS) occurred in 95%, hemorrhagic stroke (HS) in 19%, both HS and IS in 14%, and HS alone in 1 patient. Stroke recurred in 76% during follow-up; of these, 87% had IS.
Among those with IS, 45% received secondary prevention with an antiplatelet therapy. Two subjects underwent an indirect bypass surgery (encephaloduroarteriosynangiosis). All patients were followed up by another service because our hospital is a quaternary center focused on rehabilitation.
Since no other associated condition was found, 80% of the patients were classified as MMD; 15% were classified as the Moyamoya syndrome, as the sickle cell disease was present in 5%, hyperhomocysteinemia in 5%, and neurosyphilis in 5%. Another 5% were not evaluated for associated conditions.
The average mRS score at admission was 3.4 (range: 2 - 4) and 2.9 (range: 1 - 4) at discharge. On admission, those with HS had a mean mRS score of 4, while those without HS had a mean score of 3.05. Patients with HS also had a higher discharge mRS score than those without HS (Figures 1 and 2). The final mRS score did not differ between younger (< 18 years) and older (> 18 years) patients (3.1 and 3.3, respectively).
The Modified Rankim Scale at Discharge in the Ischemic stroke Group. Abbreviation: mRS, the modified Rankim scale.
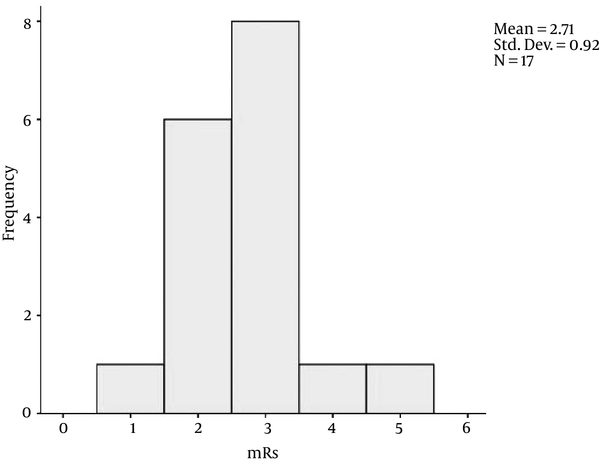
The Modified Rankim Scale (MRS) at Discharge in the Hemorrhagic Stroke Group (including the patients with Ischemic stroke and hemorrhagic stroke)

All patients with HS and 47% with IS alone developed cognitive deficits. Stroke recurred in 42% of the patients, at a mean of 11 months (range: 0 - 10 months). Only 22% of such patients were not using secondary prevention. In the surgery group, one patient had recurrence of IS and the other did not (prior to surgery, both had a history of recurrent IS only).
5. Discussion
Moyamoya syndrome is an arteriopathy associated with cerebral ischemia and stroke. The MMD prevalence peaks at two ages, with different clinical presentations: around 10 years, and at 30 - 45 years. Ischemic symptoms, including transient ischemic attacks, are the most important clinical manifestation in both children and adults. Intracranial hemorrhage is more frequent in adults than in children (10). Genetic susceptibility loci have been found on 3p, 6p, 17q, and band 8q23. Mineharu et al. identified a specific gene locus, q25.3, on chromosome (11). A genome-wide association study identified RNF213 as the first gene associated with Moyamoya.
Although MMD may occur in a previously healthy individual, many disease states have been reported in association with MMD, including thyrotoxicosis (12).
Epidemiological data on MMD show predominance in Asian populations, although there is a growing evidence of increased prevalence in non-Asian populations (13-15). Latin American and Brazilian data are still lacking (4, 6).
Our hospital-based study showed a lower average age of onset than that in the literature, a much higher incidence of IS, and similar rates of HS (4, 16). Selection bias may explain such differences, since patients with greater disability are more likely to present to our service.
The basis for treatment is neurosurgical direct or indirect arterial for HS or recurrent IS (17). Recently endovascular treatment with embolization of aneurisms also has been proposed (11).
Conservative treatment can be used; some risk factors have been associated with recurrence, such as female sex, Graves’ disease and presence of prior HS (17). There also has been an indication that hemodynamic dysfunction could be a risk factor for stroke occurrence. In general, there has been an indication for an early surgical procedure in children or symptomatic patients (17).
Patients with HS scored worse on initial and final mRS and surgical procedures did not significantly alter the prognosis. In comparison with those reported in international literature, we did not find significant differences in disability rates between younger and older patients.
After participating in a rehabilitation program, most patients showed an improved mRS score, and some achieved independence for activities of daily living. Because most patients did not undergo surgical treatment, we cannot assess the value of this intervention in the morbidity in our subjects.
The main limitations of this study include: 1) selection bias, as stated above; 2) the small number of subjects, which prevents further statistical analysis; and 3) the fact that the data were acquired retrospectively, from electronic records not originally intended for research.
5.1. Conclusions
In our experience, the rehabilitation process improves the quality of life and can have an impact on morbidity, as shown by the mRS scores on admission and discharge. Patients with HS tend to have worse outcomes. More epidemiological data from non-Asian populations are needed.
References
-
1.
Takeuchi K, Shimizu K. Hypoplasia of the bilateral internal carotid arteries. Brain Nerve. 1957;9:37-43.
-
2.
Fukui M. Guidelines for the diagnosis and treatment of spontaneous occlusion of the circle of Willis ('moyamoya' disease). Research Committee on Spontaneous Occlusion of the Circle of Willis (Moyamoya Disease) of the Ministry of Health and Welfare, Japan. Clin Neurol Neurosurg. 1997;99 Suppl 2:S238-40. [PubMed ID: 9409446].
-
3.
Fukui M, Kono S, Sueishi K, Ikezaki K. Moyamoya disease. Neuropathology. 2000;20 Suppl:S61-4. [PubMed ID: 11037190].
-
4.
Mohr JP, Grotta C, Wolf PA, Moskowitz MA, Mayberg MR, Von Kummer R. Stroke: pathophysiology, diagnosis, and management. Elsevier Health Sciences; 2011.
-
5.
Hishikawa T, Sugiu K, Date I. Moyamoya Disease: A Review of Clinical Research. Acta Med Okayama. 2016;70(4):229-36. [PubMed ID: 27549666].
-
6.
Lima TTF, Gallo P, Raupp SF, Mendonca R, Soares VB. Doença de Moyamoya: relato de caso e revisão de literatura brasileira. Arq Bras Neurocir. 2006:34-9.
-
7.
Oliveira RS, Amato MC, Simao GN, Abud DG, Avidago EB, Specian CM, et al. Effect of multiple cranial burr hole surgery on prevention of recurrent ischemic attacks in children with moyamoya disease. Neuropediatrics. 2009;40(6):260-4. [PubMed ID: 20446218]. https://doi.org/10.1055/s-0030-1249069.
-
8.
Nam KS. Long-term Outcome of Motor Function in a Child with Moyamoya Disease: A Case Report. J Phys Ther Sci. 2013;25(12):1647-9. [PubMed ID: 24409040]. https://doi.org/10.1589/jpts.25.1647.
-
9.
Cao Y, Wang S, Sun W, Dai Q, Li W, Cai J, et al. Prediction of favorable outcome by percent improvement in patients with acute ischemic stroke treated with endovascular stent thrombectomy. J Clin Neurosci. 2017. [PubMed ID: 28117261]. https://doi.org/10.1016/j.jocn.2016.12.045.
-
10.
Fujimura M, Bang OY, Kim JS. Moyamoya Disease. Front Neurol Neurosci. 2016;40:204-20. [PubMed ID: 27960175]. https://doi.org/10.1159/000448314.
-
11.
Kim SH, Kwon OK, Jung CK, Kang HS, Oh CW, Han MH, et al. Endovascular treatment of ruptured aneurysms or pseudoaneurysms on the collateral vessels in patients with moyamoya disease. Neurosurgery. 2009;65(5):1000-4. discussion 1004. [PubMed ID: 19834414]. https://doi.org/10.1227/01.NEU.0000345648.46096.CE.
-
12.
Mineharu Y, Takenaka K, Yamakawa H, Inoue K, Ikeda H, Kikuta KI, et al. Inheritance pattern of familial moyamoya disease: autosomal dominant mode and genomic imprinting. J Neurol Neurosurg Psychiatry. 2006;77(9):1025-9. [PubMed ID: 16788009]. https://doi.org/10.1136/jnnp.2006.096040.
-
13.
Goto Y, Yonekawa Y. Worldwide distribution of moyamoya disease. Neurol Med Chir (Tokyo). 1992;32(12):883-6. [PubMed ID: 1282678].
-
14.
Yonekawa Y, Ogata N, Kaku Y, Taub E, Imhof HG. Moyamoya disease in Europe, past and present status. Clin Neurol Neurosurg. 1997;99 Suppl 2:S58-60. [PubMed ID: 9409407].
-
15.
Chiu D, Shedden P, Bratina P, Grotta JC. Clinical features of moyamoya disease in the United States. Stroke. 1998;29(7):1347-51. [PubMed ID: 9660385].
-
16.
Fukui M, Kawano T. Follow-up study of registered cases. In: Fukui M, editor. Annual report (1995) by research committee on spontaneous occlusion of the circle of Willis (moyamoya disease). Tokyo, Japan: Ministry of Health and Welfare; 1995.
-
17.
Kim T, Oh CW, Bang JS, Kim JE, Cho WS. Moyamoya Disease: Treatment and Outcomes. J Stroke. 2016;18(1):21-30. [PubMed ID: 26846757]. https://doi.org/10.5853/jos.2015.01739.