Abstract
Background:
Imbalance between the vastus medialis oblique (VMO) muscle and the vastus lateralis oblique (VTO) Vastus lateralis has been thought to be a primary cause of abnormal patellar tracking, possibly leading to patellofemoral pain syndrome (PFPS).Objectives:
The purpose of this study was to investigate the effect of quadriceps muscle strengthening exercises on the ratio of VMO to VL oblique and longus muscle fiber angles.Patients and Methods:
Thirty-five subjects (23 females and 12 males, mean age 26.6 years ± 1.1 SD) with PFPS were randomized into an exercise group or a control group. The exercise group performed knee extension exercises for four weeks based on the Kaya exercise program (three times per week), while the control group received no treatment. Measurements included knee extensor concentric and eccentric muscle torque using a Biodex isokinetic machine and the fiber angle of the VMO, VL oblique and longus muscles using ultrasonography, all of which were evaluated at the time of the initial examination and at the end of the four-week period.Results:
There were no significant differences in the muscle strength and fiber angle of the VMO, VL oblique and longus muscles after training between the control and experimental groups (P > 0.05).Conclusions:
The study findings indicate that short-term exercises had no significant effect on the ratio of VMO to VL muscle fiber angles in patients with PFPS.Keywords
Patellofemoral Pain Syndrome Torque Ultrasonography Muscle Fiber Angle
1. Background
Patellofemoral pain syndrome (PFPS) is one of the most common knee disorders experienced by active adults and adolescents (1, 2). PFPS can be defined as either retropatellar or peripatellar pain (1, 3) and is the most frequently diagnosed condition in patients under 50 with knee complaints (4). The cause is thought to be multi-factoral (4-6), with some of the main contributing factors being abnormal tracking (7, 8), lateral patellar malalignments (9, 10), and decreased patellofemoral joint contact area, such as in patella alta (11). These factors may induce uneven stresses on both the patella itself and the peripatellar tissues (12). Abnormal patellar tracking may be due to excessive foot pronation, patellofemoral ligament properties, joint conformity, a large quadriceps angle, and altered muscle recruitment at the hip joint with increased femoral rotation (13). Under normal conditions, the vastus medialis oblique (VMO) muscle is able to counterbalance the lateral pull of the large vastus lateralis (VL) muscle to ensure patellar stability (6). The VM and VL muscles are countervail each other to adjust the location of the patella in the patellofemoral joint (14). Although few studies have found any link between patellar malalignment and PFPS (8), it has been noted that an imbalance between the VMO and the VL can alter patellar alignment during knee extension, leading to pathological problems in the patellofemoral joint (15).
Various studies have demonstrated morphological changes, such as significantly smaller VMO volume (6, 8, 16, 17), insertion volume, and fiber angles in PFPS (17). Furthermore, there is a significant correlation between decreased VMO fiber angle and patellar malalignment (8, 18). To understand the involvement of the VL muscle in the pathogenesis of knee dysfunction, precise knowledge of its anatomical structure is essential. However, there is a lack of information on the architecture of the VL muscle (19, 20). In one study, the authors compared the VMO and VL in individuals with PFPS and found atrophy in both muscles, although no significant difference was found in the amount of atrophy (16). There is insufficient data to determine if there is greater atrophy of the VMO than of the VL (6, 16). In addition, tightness of these muscles has been reported to contribute to this dysfunction (20). Studies about other morphological characteristics of VL, such as fiber angles, are sparse. Most studies only report on healthy groups and not on those with PFPS (19), thus resulting in a dearth of information (21).
Investigation of VMO fiber angles, VL fiber angles, and the ratio of VMO fiber angles to VL fiber angles will provide a better understanding of the relationship between the morphological parameters of the VMO and VL to patellar kinematics and the etiology of PFPS.
PFPS patients who possess lower VMO activation compared to VL activation do not necessarily have quadriceps weakness (22), and the patellar tilt angle has not been reported to change after improvements in quadriceps strength (11). Nonetheless, there is a gap in determining the effect of quadriceps exercise on the fiber angles of VMO and VL muscles in PFPS.
2. Objectives
The purpose of this study was to investigate the effect of quadriceps strengthening exercises on the ratio of VMO to VL muscle fiber angles.
3. Patients and Methods
3.1. Subjects
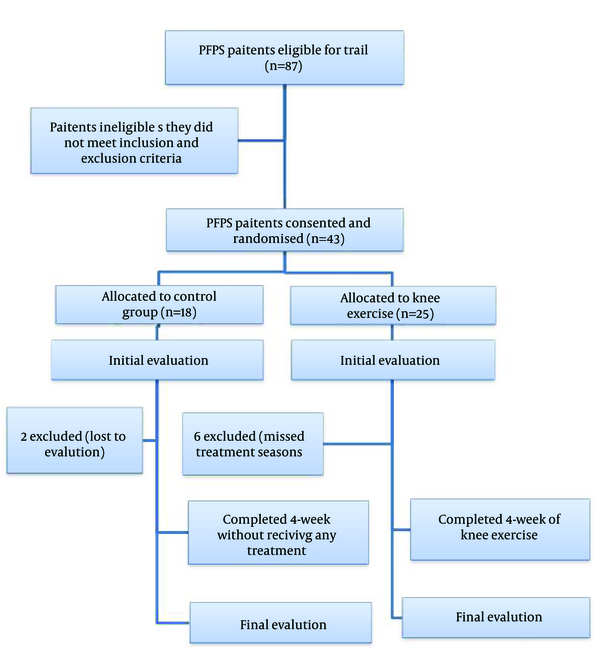
This study was a randomized controlled trial approved by the ethics committee of Semnan university of medical sciences. All subjects were recruited from the orthopedics outpatient clinics of Tehran university of medical sciences and gave written informed consent before joining the study. Forty-three subjects with PFPS between 12 and 40 years of age were examined by trained physiotherapists to ensure they met the required inclusion and exclusion criteria. They were randomized into two groups, an experimental group that performed quadriceps strengthening exercises for four weeks and a control group that received no treatment. Knee extensor muscle strength and VMO, VL oblique and longus muscle fiber angles were evaluated at the time of the initial examination and at the end of the four-week period (Figure 1).
Study Flow Diagram
The inclusion criteria for this study were 1) pre- or retropatellar knee pain on at least two of the following activities: prolonged sitting, climbing stairs, squatting, running, kneeling, or hopping/jumping; 2) the presence of two of the following clinical criteria on assessment: pain during the apprehension test, pain during the patellar compression test, and crepitation during the compression test; 3) age between 12 and 40 (to reduce the likelihood of osteoarthritic changes in the patellofemoral joint); and 4) symptoms of anterior knee pain for at least three months (6). The exclusion criteria consisted of 1) history or evidence of other knee disorders, such as ligament injury, bursitis, meniscal injury, or osteoarthritis; 2) history of lower limb surgery or trauma less than one 1 year previous; 3) patellar instability; 4) referred pain from the lumbar spine hip and ankle joint (1, 6, 8); 5) the presence of any abnormality in the lower extremities; 6) inflexibility of the soft tissue structures, such as quadriceps, hamstrings, triceps surae, and iliotibial band (7, 23); and 7) lateral deviation of the patella greater than 5 mm, lateral patella tilt, hypo or hypermobility on medial glide of the patella, determined using the method described by Herrington and Pearson (24).
3.2. Intervention
While the participants in the control group did not receive any form of treatment, the subjects in the experimental group undertook four weeks of exercises three times per week based on weeks 1 - 4 of the Kaya exercise program for patients with PFPS (Table 1) (25). All the patients in the exercise group received an exercise logbook (26), and the exercises were checked weekly by a physiotherapist (27).
The Kaya Quadriceps Exercise Protocol
| Exercises | Duration |
|---|---|
| Stretches (All session) | 3 sets of 10 repetitions/10 s hold |
| Hamstring stretch | NA |
| Quadriceps stretch | NA |
| Calf and iliotibial band stretch | NA |
| Weeks 1 - 2 | |
| Wall squat (0° - 40° of knee flexion) | 15 repetitions/10 s hold |
| Quadriceps isometric | 4 sets of 25 repetitions |
| Straight leg raises | 3 sets of repetitions |
| Weeks 3 - 4 | |
| Wall squat (0° - 60° of knee flexion) | 15 repetitions/10 s hold |
| Quadriceps isometric | 4 sets of 25 repetitions |
| Straight leg raises | 3 sets of repetitions |
| Terminal knee extension | 3 sets of 10 repetitions |
3.3. Measurements
The subjects’ ages, heights, weights, and BMIs were documented prior to the testing procedures. All measurements were performed by an examiner at a specific time of the day at the beginning and end of the four weeks.
3.4. Knee Muscle Strength
The knee muscle strength was measured using an isokinetic dynamometer (Biodex system 3) at an angular speed of 120 degrees/s. The reliability of the Biodex isokinetic machine was confirmed in previous studies (28). The subjects were in a sitting position on an isokinetic test bench with the knee at 90° flexion. The anatomical axis of the subject’s knee was aligned with the mechanical axis of the dynamometer. The tibial plate on the input arm was positioned proximally 4.5 cm superior to the subject’s medial malleolus. Stabilization was provided by thoracic and waist belts and a tight strap.
Subjects were oriented to the procedure to activate the input arm for a concentric quadriceps muscle contraction and eccentric quadriceps muscle contraction. The concentric quadriceps muscle contraction was performed first, began with the knee positioned at 90° flexion, and stopped with the knee positioned at 0° flexion. Next, the subjects were asked to control the input arm movement when the eccentric quadriceps muscle contraction began with the knee positioned at 0˚ flexion and ended at 0° flexion. The subjects performed two sets of five repetitions with maximal effort, and the higher value of the concentric and eccentric torque was used for analysis (11, 29).
3.5. Ultrasound Protocol
The ultrasonography was performed using an HS-2600 ultrasonic scanner. A 5-12 MHZ linear array transducer was used, and all parameters were set at ranges suitable for assessment of the knee joint (8).
The sonographic knee measurements were obtained with the subjects lying supine on a bed. The tests were performed in two positions, with the subjects’ knees flexed at 0° and 45° (the knee bend was used to reduce fascicle curvature); both legs were relaxed and supported with a holder to prevent lower limb rotation (8, 30). A water-soluble gel was applied to the probe to aide acoustic contact and to remove the need for contact with the skin, thus eliminating the deformation of muscle that might occur if pressure was applied. The probe was oriented parallel to the muscle fascicle and perpendicular to the skin (30).
The fiber angle of the VMO was calculated based on the direction of the rectus femoris (estimated based on a line from the anterior superior iliac spine to the center of the patella) (12). The direction of the VMO fiber angle at the level of their insertion to the patella was determined by rotating the ultrasound probe until the fibers were displayed parallel to each other on the sonographic image. In this position, the line along the ultrasound probe represented the direction of the VMO fibers. The fiber angles of the VMO were, therefore, measured as the angle between the line along the border of the ultrasound probe when the VMO fibers were displayed parallel to each other on the sonographic image and the line from the anterior superior iliac spine to the center of the patella (31). All the measurements were taken three times, and the average of these three measurements were used for analysis (32). The VL oblique and longus muscle fiber angles were measured at 2 cm from the most distal part of muscle (33) at two separate locations on the VL muscle (32). The rest of the procedures were then performed, such as testing of the VMO fiber angles.
3.6. Intra-Rater Reliability Study
A preliminary study was conducted on 10 subjects with no PFPS. To assess the intra-rater reliability of the VMO, VL oblique, and VL longus fiber angles at 0° and 45° knee flexion on the sonographic images, repeated measurements were obtained one week later by one investigator (17).
3.7. Data Analysis
The intra-class correlation coefficient was used to evaluate the intra-rater reliability of muscle fiber angle measurements. The Kolmogorov-Smirnoff test was used to identify normal data distribution. An independent sample t test was used to compare the mean change between the experimental and control groups. All statistical analyses were performed using SPSS 20 statistical software. An alpha level of P<0.05 was considered statistically significant for all analyses.
4. Results
Forty-three patients with PFPS participated in this study; 18 participants in the control group did not receive treatment, and 25 participants in the experimental group undertook the exercise program. Eight patients did not complete the study. Table 2 shows the demographic data of all the subjects. There were no significant differences among the groups in terms of age, sex, and BMI. The intra-rater reliability of the ultrasound measurement technique for all the tested parameters was good (Table 3).
| Variable | Control Group | Exercise Group | P Value |
|---|---|---|---|
| Age, y | 26.6 ± 1.1 | 27.5 ± 1.3 | .89 |
| BMI, kg/m² | 23.8 ± 0.6 | 23.7 ± 0.7 | .93 |
The Intra-Class Correlation Coefficient (ICC) From Two Ultrasonography Sessions of Muscle Fiber Angles
| Variable | ICC | |
|---|---|---|
| r | P Value | |
| FAVM0°F | 0.95 | < .0001 |
| FAVM45°F | 0.91 | < .0001 |
| FAVLO0°F | 0.94 | < .0001 |
| FAVLO45°F | 0.80 | < .0001 |
| FAVLL0°F | 0.88 | < .0001 |
| FAVLL45°F | 0.68 | < .0001 |
Regarding the variables of maximum eccentric and concentric quadriceps torque, VMO fiber angle, VL oblique and longus muscle fiber angle, there was no statistically significant difference between two control and exercise groups (P > 0.05) (Table 4).
Within Group and Between Group Comparison of Knee Strength and Muscles Fiber Angle of Vastus Medialis and Vastus Lateralis Muscles at 0° and 45° Knee Flexion
| Variable | Control Group (n = 16) | Exercise Group (n = 19) | Between group P Value | ||||
|---|---|---|---|---|---|---|---|
| Before | After | Mean Change (within group P value) | Before | After | Mean Change (within group P value) | ||
| MEQT (Newton) | 63.4 ± 16.6 | 65.1 ± 17.3 | 1.8 ± 11.6, (0.52) | 66.6 ± 20.5 | 75.1 ± 19.2 | 8.4 ± 12.5 (0.08) | .11 |
| MCQT (Newton) | 44.3 ± 14.5 | 46.7 ± 16.9 | 2.3 ± 9.4 (0.71) | 44.4 ± 17.4 | 53.2 ± 20.1 | 8.9 ± 11.3 (0.06) | .07 |
| FAVM0°F (Degree) | 50.6 ± 5.9 | 50.4 ± 6.5 | 0.2 ± 2.3 (0.81) | 49.0 ± 3.4 | 50.3 ± 2.7 | 1.3 ± 2.3 (0.56) | .06 |
| FAVM45°F (Degree) | 41.9 ± 4.7 | 40.9 ± 5.5 | 2.0 ± 3.6 (0.91) | 39.7 ± 3.5 | 38.7 ± 4.8 | 1.0 ± 3.1 (0.68) | .08 |
| FAVLO0°F (Degree) | 34.9 ± 6.2 | 35.1 ± 6.5 | 0.3 ± 3.9 (0.76) | 33.5 ± 4.7 | 33.2 ± 4.2 | 0.2 ± 2.3 (0.75) | .65 |
| FAVLO45°F (Degree) | 25.7±5.3 | 26.4 ± 6.9 | 0.7±3.1 (0.63) | 23.2 ± 4.1 | 23.4 ± 3.8 | 0.3 ± 2.7 (0.84) | .59 |
| FAVLL0°F (Degree) | 14.9 ± 4.9 | 15.3 ± 3.9 | 0.4±2.5 (0.59) | 12.3 ± 2.3 | 15.4±3.9 | 0.8 ± 2.1 (0.18) | .65 |
| FAVLL45°F (Degree) | 9.1 ± 2.4 | 9.6 ± 2.7 | 0.6 ± 1.9 (0.64) | 7.4 ± 1.7 | 8.1 ± 1.6 | 0.7 ± 1.5 (0.37) | .77 |
After four weeks, a comparison of mean changes did not show any significant difference in isokinetic quadriceps strength or the fiber angles of the muscles between and within groups (P > 0.05) (Table 4).
5. Discussion
In this study, there were no significant differences between maximum eccentric quadriceps torque and maximum concentric quadriceps torque for the control and experimental groups. Contradictory to our results, Herrington et al. reported an increase in maximum isometric quadriceps torque after six weeks of both close kinematic chain exercises and open kinematic chain exercises performed three times per week (34). However, this discrepancy might be due to the modest total training in our study. Mason et al. showed a significant improvement after a daily program of non-weight bearing terminal range quadriceps exercises for one week. The exercises were performed as home exercise, and the authors attributed the changes in strength to central changes rather than to the physiological changes in the muscle (35). Although we did not find any significant changes in quadriceps strength between the two groups, the experimental group was found to have more improvements in mean changes of maximum eccentric (8.4 ± 12.5) and concentric (8.9 ± 11.3) quadriceps torque compared to the mean changes of maximum eccentric (1.8 ± 11.5) and concentric (2.3 ± 9.4) quadriceps torque in the control group. However, it seems that using the Kaya exercise protocol for four weeks was not enough to strengthen the quadriceps muscle. Therefore, it may need to develop special exercises for these patients (25).
We found no significant differences in the VMO and VL oblique on 0° and 45° knee flexion between the experimental group and the control group.
The mean angle of VMO at 0° knee flexion for the experimental group was (49.0 ± 3.4) and was (50.6 ± 5.9) for the control group. Jan et al. (2009) (17) and Lin et al. (2008) (8) reported the VMO angle to be 51.6 ± 9 and 52.6 ± 8.8 in patients with PFPS. Engelina et al. (2014) reported a baseline value for VMO fiber angle in young asymptomatic adults (57.4° for males and 56.0 for females), a larger VMO angle than that previously reported in people suffering with PFPS (36). Nonetheless, it is important to note that 11 out of a sample of 40 healthy knees assessed in the study by Engelina et al. (2014) (27.5%) and 18 out of 54 pathological knees examined by Jan et al. (2009) (33.3 %) exhibited an angle less than 51°, indicating a degree of overlap between normal and pathological values (8, 17, 36).
In our study, VLL fiber angles were within the normal range reported by Becker et al. in their cadaveric study (12° - 15°). The mean fiber angle of the VL oblique at 0° flexion of the knee in the experimental group was 34.8 ± 6.20, while it was 33.5 ± 4.67 for the control group. However, the cadaveric studies that were performed on non-pathological knee specimens, reported some different muscle fiber angle for VL muscles (19).
The mean angles of the VMO, VL oblique, and longus at 45° knee flexion in both the experimental and control groups were smaller than 0° knee flexion. These results were confirmed in a study by Aagaard et al. who suggested steeper pennation angles in conditions of shortened muscle length, that is, during full knee extension (37).
In the present study, a comparison of the mean changes between the two groups revealed no significant differences in any muscle fiber angles. In agreement with our results, Baroni et al. (2013) reported no pennation angle changes in the rectus femoris or the VL after four weeks of isokinetic eccentric training (38). However, in this studies, the pennation angle was defined as the angle between the echo of the deep aponeurosis and the echo of the space between the fascicles. According to Benjafield et al. (2015), the mean VMO fiber angles for the athletic group are significantly higher than for the sedentary group (39). However, by comparing our findings with other reported results, it may be concluded that using quadriceps exercise for a short time, such as four weeks, may not affect the muscle fiber angle; therefore, no beneficial effect may be expected from short-term exercise training. This argument may be supported by other studies that advise more prolonged exercise protocols (11, 22).
5.1. Conclusion
The four weeks of strength training had no effect on the ratio of the VMO and the VL muscle fiber angles in patients with PFPS. According to the results, the effect of the short -term strengthening program on PFPS is not related to any changes in the VMO fiber angle or the VL fiber angle. However, the short duration of the exercise program, the constant training load for all participants, and the non-adjustable progressive resistive exercise during the training program without considering the participants’ physical condition are the limitations of this study and may explain the findings. The other limitation was the small number of subjects who participated in the study. We recommend larger studies about VMO and VL morphological adaptation in patients with PFPS using adjustable progressive resistive exercises and taking participants’ physical strength into consideration.
The present study examined the effect of strengthening quadriceps exercise on the muscle fiber alignment of VM and VL muscles in patients with patellofemoral pain syndrome. The results showed that four weeks of quadriceps strengthening exercise may affect neither the muscle fiber structure, nor quadriceps muscle torques. It may be concluded from these findings that a much longer strengthening exercise therapy protocol for quadriceps muscles is necessary to re-align the muscle fibers and thus modify pattelar tracking during knee extension, although this should be confirmed in future studies.
Acknowledgements
References
-
1.
Bolgla LA, Boling MC. An update for the conservative management of patellofemoral pain syndrome: A systematic review of the literature from 2000 to 2010. Int J Sports Phys Ther. 2011;6(2):112-25. [PubMed ID: 21713229].
-
2.
Bolgla LA, Malone TR, Umberger BR, Uhl TL. Comparison of hip and knee strength and neuromuscular activity in subjects with and without patellofemoral pain syndrome. Int J Sports Phys Ther. 2011;6(4):285-96. [PubMed ID: 22163090].
-
3.
Botanlioglu H, Kantarci F, Kaynak G, Unal Y, Ertan S, Aydingoz O, et al. Shear wave elastography properties of vastus lateralis and vastus medialis obliquus muscles in normal subjects and female patients with patellofemoral pain syndrome. Skeletal Radiol. 2013;42(5):659-66. [PubMed ID: 22996306]. https://doi.org/10.1007/s00256-012-1520-4.
-
4.
Lankhorst NE, Bierma-Zeinstra SM, van Middelkoop M. Risk factors for patellofemoral pain syndrome: a systematic review. J Orthop Sports Phys Ther. 2012;42(2):81-94. [PubMed ID: 22031622]. https://doi.org/10.2519/jospt.2012.3803.
-
5.
Kaya D, Citaker S, Kerimoglu U, Atay OA, Nyland J, Callaghan M, et al. Women with patellofemoral pain syndrome have quadriceps femoris volume and strength deficiency. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):242-7. [PubMed ID: 20953760]. https://doi.org/10.1007/s00167-010-1290-2.
-
6.
Pattyn E, Verdonk P, Steyaert A, Vanden Bossche L, Van den Broecke W, Thijs Y, et al. Vastus medialis obliquus atrophy: Does it exist in patellofemoral pain syndrome? Am J Sports Med. 2011;39(7):1450-5. [PubMed ID: 21487120]. https://doi.org/10.1177/0363546511401183.
-
7.
Sheehan FT, Derasari A, Fine KM, Brindle TJ, Alter KE. Q-angle and J-sign: Indicative of maltracking subgroups in patellofemoral pain. Clin Orthop Relat Res. 2010;468(1):266-75. [PubMed ID: 19430854]. https://doi.org/10.1007/s11999-009-0880-0.
-
8.
Lin YF, Lin JJ, Cheng CK, Lin DH, Jan MH. Association between sonographic morphology of vastus medialis obliquus and patellar alignment in patients with patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2008;38(4):196-202. [PubMed ID: 18434663]. https://doi.org/10.2519/jospt.2008.2568.
-
9.
Song CY, Lin JJ, Jan MH, Lin YF. The role of patellar alignment and tracking in vivo: the potential mechanism of patellofemoral pain syndrome. Phys Ther Sport. 2011;12(3):140-7. [PubMed ID: 21802041]. https://doi.org/10.1016/j.ptsp.2011.04.004.
-
10.
Wilson T. The measurement of patellar alignment in patellofemoral pain syndrome: Are we confusing assumptions with evidence? J Orthop Sports Phys Ther. 2007;37(6):330-41. [PubMed ID: 17612360]. https://doi.org/10.2519/jospt.2007.2281.
-
11.
Chiu JK, Wong YM, Yung PS, Ng GY. The effects of quadriceps strengthening on pain, function, and patellofemoral joint contact area in persons with patellofemoral pain. Am J Phys Med Rehabil. 2012;91(2):98-106. [PubMed ID: 22248804]. https://doi.org/10.1097/PHM.0b013e318228c505.
-
12.
Elias DA, White LM. Imaging of patellofemoral disorders. Clin Radiol. 2004;59(7):543-57. [PubMed ID: 15208060]. https://doi.org/10.1016/j.crad.2004.01.004.
-
13.
Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20(5):725-30. [PubMed ID: 19765240]. https://doi.org/10.1111/j.1600-0838.2009.00996.x.
-
14.
Lee SE, Cho SH. The effect of McConnell taping on vastus medialis and lateralis activity during squatting in adults with patellofemoral pain syndrome. J Exerc Rehabil. 2013;9(2):326-30. [PubMed ID: 24278879]. https://doi.org/10.12965/jer.130018.
-
15.
Smith TO, Davies L, Donell ST. The reliability and validity of assessing medio-lateral patellar position: A systematic review. Man Ther. 2009;14(4):355-62. [PubMed ID: 18824392]. https://doi.org/10.1016/j.math.2008.08.001.
-
16.
Giles LS, Webster KE, McClelland JA, Cook J. Does quadriceps atrophy exist in individuals with patellofemoral pain? A systematic literature review with meta-analysis. J Orthop Sports Phys Ther. 2013;43(11):766-76. [PubMed ID: 24175596]. https://doi.org/10.2519/jospt.2013.4833.
-
17.
Jan MH, Lin DH, Lin JJ, Lin CH, Cheng CK, Lin YF. Differences in sonographic characteristics of the vastus medialis obliquus between patients with patellofemoral pain syndrome and healthy adults. Am J Sports Med. 2009;37(9):1743-9. [PubMed ID: 19521000]. https://doi.org/10.1177/0363546509333483.
-
18.
Lin YF, Lin JJ, Jan MH, Wei TC, Shih HY, Cheng CK. Role of the vastus medialis obliquus in repositioning the patella: A dynamic computed tomography study. Am J Sports Med. 2008;36(4):741-6. [PubMed ID: 18337358]. https://doi.org/10.1177/0363546507312171.
-
19.
Becker I, Woodley SJ, Baxter GD. Gross morphology of the vastus lateralis muscle: An anatomical review. Clin Anat. 2009;22(4):436-50. [PubMed ID: 19306318]. https://doi.org/10.1002/ca.20792.
-
20.
Becker I, Baxter GD, Woodley SJ. The vastus lateralis muscle: an anatomical investigation. Clin Anat. 2010;23(5):575-85. [PubMed ID: 20309954]. https://doi.org/10.1002/ca.20974.
-
21.
Nunes GS, Stapait EL, Kirsten MH, de Noronha M, Santos GM. Clinical test for diagnosis of patellofemoral pain syndrome: Systematic review with meta-analysis. Phys Ther Sport. 2013;14(1):54-9. [PubMed ID: 23232069]. https://doi.org/10.1016/j.ptsp.2012.11.003.
-
22.
Toumi H, Best TM, Pinti A, Lavet C, Benhamou CL, Lespessailles E. The role of muscle strength & activation patterns in patellofemoral pain. Clin Biomech (Bristol, Avon). 2013;28(5):544-8. [PubMed ID: 23664197]. https://doi.org/10.1016/j.clinbiomech.2013.04.005.
-
23.
Callaghan MJ, Oldham JA. Quadriceps atrophy: To what extent does it exist in patellofemoral pain syndrome? Br J Sports Med. 2004;38(3):295-9. [PubMed ID: 15155431].
-
24.
Herrington L, Pearson S. The applicability of ultrasound imaging in the assessment of dynamic patella tracking: A preliminary investigation. Knee. 2008;15(2):125-7. [PubMed ID: 18234499]. https://doi.org/10.1016/j.knee.2007.12.005.
-
25.
Kaya D, Doral MN, Callaghan M. How can we strengthen the quadriceps femoris in patients with patellofemoral pain syndrome? Muscles Ligaments Tendons J. 2012;2(1):25-32. [PubMed ID: 23738270].
-
26.
Bily W, Trimmel L, Modlin M, Kaider A, Kern H. Training program and additional electric muscle stimulation for patellofemoral pain syndrome: a pilot study. Arch Phys Med Rehabil. 2008;89(7):1230-6. [PubMed ID: 18586125]. https://doi.org/10.1016/j.apmr.2007.10.048.
-
27.
Loudon JK, Wiesner D, Goist-Foley HL, Asjes C, Loudon KL. intrarater reliability of functional performance tests for subjects with patellofemoral pain syndrome. J Athl Train. 2002;37(3):256-61. [PubMed ID: 12937582].
-
28.
Drouin JM, Valovich-mcLeod TC, Shultz SJ, Gansneder BM, Perrin DH. Reliability and validity of the Biodex system 3 pro isokinetic dynamometer velocity, torque and position measurements. Eur J Appl Physiol. 2004;91(1):22-9. [PubMed ID: 14508689]. https://doi.org/10.1007/s00421-003-0933-0.
-
29.
Sczepanski TL, Gross MT, Duncan PW, Chandler JM. Effect of contraction type, angular velocity, and arc of motion on VMO:VL EMG ratio. J Orthop Sports Phys Ther. 1991;14(6):256-62. [PubMed ID: 18796810]. https://doi.org/10.2519/jospt.1991.14.6.256.
-
30.
Blazevich AJ, Gill ND, Zhou S. Intra- and intermuscular variation in human quadriceps femoris architecture assessed in vivo. J Anat. 2006;209(3):289-310. [PubMed ID: 16928199]. https://doi.org/10.1111/j.1469-7580.2006.00619.x.
-
31.
Engelina S, Robertson CJ, Moggridge J, Killingback A, Adds P. Using ultrasound to measure the fibre angle of vastus medialis oblique: a cadaveric validation study. Knee. 2014;21(1):107-11. [PubMed ID: 22819896]. https://doi.org/10.1016/j.knee.2012.07.001.
-
32.
Wells AJ, Fukuda DH, Hoffman JR, Gonzalez AM, Jajtner AR, Townsend JR, et al. Vastus lateralis exhibits non-homogenous adaptation to resistance training. Muscle Nerve. 2014;50(5):785-93. [PubMed ID: 24616036]. https://doi.org/10.1002/mus.24222.
-
33.
Blazevich AJ, Gill ND, Bronks R, Newton RU. Training-specific muscle architecture adaptation after 5-wk training in athletes. Med Sci Sports Exerc. 2003;35(12):2013-22. [PubMed ID: 14652496]. https://doi.org/10.1249/01.MSS.0000099092.83611.20.
-
34.
Herrington L, Al-Sherhi A. A controlled trial of weight-bearing versus non-weight-bearing exercises for patellofemoral pain. J Orthop Sports Phys Ther. 2007;37(4):155-60. [PubMed ID: 17469667]. https://doi.org/10.2519/jospt.2007.2433.
-
35.
Mason M, Keays SL, Newcombe PA. The effect of taping, quadriceps strengthening and stretching prescribed separately or combined on patellofemoral pain. Physiother Res Int. 2011;16(2):109-19. [PubMed ID: 20632302]. https://doi.org/10.1002/pri.486.
-
36.
Engelina S, Antonios T, Robertson CJ, Killingback A, Adds PJ. Ultrasound investigation of vastus medialis oblique muscle architecture: an in vivo study. Clin Anat. 2014;27(7):1076-84. [PubMed ID: 24797580]. https://doi.org/10.1002/ca.22413.
-
37.
Aagaard P, Andersen JL, Dyhre-Poulsen P, Leffers AM, Wagner A, Magnusson SP, et al. A mechanism for increased contractile strength of human pennate muscle in response to strength training: changes in muscle architecture. J Physiol. 2001;534(Pt. 2):613-23. [PubMed ID: 11454977].
-
38.
Baroni BM, Geremia JM, Rodrigues R, De Azevedo Franke R, Karamanidis K, Vaz MA. Muscle architecture adaptations to knee extensor eccentric training: rectus femoris vs. vastus lateralis. Muscle Nerve. 2013;48(4):498-506. [PubMed ID: 23852989]. https://doi.org/10.1002/mus.23785.
-
39.
Benjafield AJ, Killingback A, Robertson CJ, Adds PJ. An investigation into the architecture of the vastus medialis oblique muscle in athletic and sedentary individuals: an in vivo ultrasound study. Clin Anat. 2015;28(2):262-8. [PubMed ID: 25244030]. https://doi.org/10.1002/ca.22457.