Abstract
Background:
Tuberculosis (TB) affects various aspects of quality of life (QoL), and self-care is the most important form of primary care and one of the main factors involved in the process of treating chronic diseases and improving the patients’ QoL.Objectives:
This study aimed to investigate the effect of self-care education on the QoL of TB patients.Methods:
In this quasi-experimental study, 110 TB patients referred to the TB coordinating Center in Zahedan, Southeastern Iran, in 2018, are studied. Participants were selected using convenience sampling and were randomly assigned to the intervention (n = 55) and control (n = 55) groups. Data were collected using the tuberculosis quality of life-version 2 (TBQol-v2). For the intervention group, first, patients and their caregivers were divided into groups compromising of 4 to 6 members, and then three sessions of self-care education, including lectures and questions and answers meetings, each lasted for 30 minutes (in total 90 minutes) were provided to each group. Data were analyzed in SPSS version 21 using descriptive statistical tests, independent t-test, paired t-test, and chi-squared test.Results:
Mean of the total QoL score of the two groups before the intervention was 67.56 ± 5.99 and 67.09 ± 5.03, respectively, indicating no significant difference (P = 0.65). But after providing the intervention, the mean score of patients QoL in the intervention group (74.84 ± 4.90) was significantly higher than the control group (67.98 ± 0.68) (P = 0.001).Conclusions:
Since self-care education can effectively enhance the QoL of TB patients, it is recommended to provide such educations for both treatment and follow-up of these patients along with directly observed treatment, short-course (DOTS).Keywords
1. Background
As one of the top 10 causes of mortality worldwide, tuberculosis (TB) is a growing public health challenge in many parts of the world, especially in developing countries (1, 2). Next to human immunodeficiency virus infection, TB is the second leading cause of death due to infectious diseases (3).
According to the World Health Organization, ten million people fell ill with TB worldwide and claimed 1.5 million lives in 2018. “over 95% of TB cases and deaths occur in developing countries”. In 2018, most cases of TB (44%) were reported in Southeast Asia. “growing poverty, migration, and unemployment are factors that heighten the incidence and prevalence of this infection” (2).
In the Eastern Mediterranean Region, where Iran is also located, the estimated annual incidence rate of TB is 810,000, that only 537,761 of them were reported in 2018 (4). In Iran, a total of 8,819 cases of TB were reported in 2017, that most of them are reported in Sistan-and-Baluchestan and Golestan provinces (5, 6).
TB usually presents as a disease of the lungs, but it can affect any organ in the body. The lesions caused by TB that remain in the lungs are both an important factor that leads to and a prognosis for physical disability, cor pulmonale, and opportunistic infections, which all decrease the quality of life (QoL) of patients (7).
The disease affects all domains of health (that is, physical, mental, occupational, and social) (8). QoL is a broad and complex concept that encompasses physical health, mental status, personal beliefs, social relationships, and environmental factors (9). Similar to other chronic diseases, TB causes many challenges such as the pressure of trying to control and treat the disease, following long-term treatment-care plans, multiple side effects of medication, frequent visits to the physician, worries about the consequences of the disease, disruption in social and family relationships, anxiety, depression, despair, and fear of economic problems, all of which negatively affect the QoL (10-12). There is ample evidence that TB negatively affects patients’ QoL and general health (13-16).
Self-care enables the patients to better prevent the acute and chronic complications caused by the diseases as well as to enhance their QoL through recovering their health sooner (17, 18). Also, by adopting self-care behaviors which emphasize on evaluating and controlling the symptoms of the diseases (e.g., following diet therapy, maintaining a healthy lifestyle, and curbing negative impacts of the disease on daily functioning, emotions, and social relationships), it plays an important role in controlling many chronic diseases (19).
Several studies reported that effective treatment, adherence to diet therapy, counseling, and self-care, enhance the QoL of TB patients, especially in the physical and mental dimensions (14, 20, 21).
Since QoL has increasingly replaced traditional criteria, including mortality and morbidity, of assessing outcomes of the treatment, it is crucial to address patients’ QoL, especially in the case of chronic diseases such as tuberculosis that have long-term effects on physical, mental, and social domains of health. Besides, studying the QoL of TB patients is useful for designing better interventions that improve patients’ health status (22).
2. Objectives
The current study aimed to investigate the effect of self-care education on QoL of TB patients referred to the TB Coordinating Center in Zahedan in 2018.
3. Methods
This is a quasi-experimental study with a pretest-posttest design. The study population comprised all patients with pulmonary TB referred to the TB Coordinating Center in Zahedan, southeastern Iran, in 2018. The eligibility criteria included being aged 18 - 65 years, having a pulmonary TB diagnosis for the first time, passage of at least 2 - 3 months from treatment, Iranian nationality, no hearing problems, no known psychiatric illness, no history of using neuroleptics, and having no underlying condition such as heart disease, diabetes, kidney disease, and AIDS. Exclusion criteria included absence from training sessions, migration, and the patient’s death.
The sample size of each group was calculated based on the following assumptions: Confidence interval = 95%; power = 80%. The mean and standard deviation of patients’ performance scores towards self-care promoting behaviors were obtained from the study by Jadgal et al. (23). Then, using the following formula, the sample size in each group was estimated at 55 subjects.
The data collection instrument included a questionnaire consisting of two parts: demographic characteristics (age, gender, marital status, education, occupation, ethnicity), and Tuberculosis Quality of life version 2 (TBQol-v2). TBQol-v2 was designed by Chaoyang et al. (24) and includes 24 items classified in 6 dimensions: physical (6 items), psychological/emotional (5 items), functional/independence (4 items), social/family (3 items), environmental (3 items), and beliefs and spirituality (3 items). Items should be answered using a five-point Likert scale (never = 1, rarely = 2, to some extent = 3, almost high = 4, very high = 5), which a score of one represents a poor status, while a score of five indicates “excellent status concerning the QoL”. The physical, psychological/emotional, functional/independence, social/family, environmental, and beliefs and spirituality dimensions of this scale are respectively scored 6 - 30, 5 - 25, 4 - 20, 3 - 15, 3 - 15, and 3 - 15. The total score of TBQol-v2 ranges from 24 to 120, with the higher the score, the better the QoL. In this study, the score of each sub-scale was converted to 100 in order to compare different dimensions of QoL.
Using Cronbach's alpha coefficient, Chaoyang et al. (24) reported the following reliability scores for different domains of this questionnaire: Physical = 0.81, emotional = 0.88, independence = 0.89, social = 0.79, environmental = 0.74, and spiritual = 0.77. The authors, however, did not report the total reliability score of this scale. In Iran, Robabi et al. (25) reported a coefficient of 0.84. In the present study, the reliability of this questionnaire was confirmed using Cronbach's alpha coefficient (0.83). Since all domains of the questionnaire have a similar number of items, we converted their respective scores to 100 to facilitate the intra-comparison of domains.
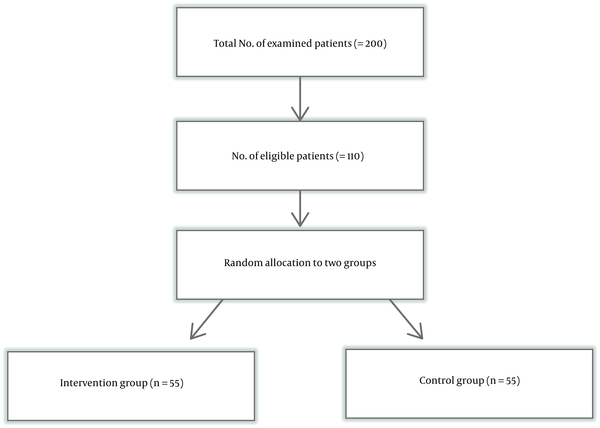
After obtaining the approval of the University Ethics Committee and making the necessary arrangements, we prepared a list of patients by referring to the TB Coordinating Center in Zahedan. Afterward, based on the inclusion criteria, patients were contacted, and, if they were agreeing, the objectives of the study were explained to them, and then they were invited to participate in the research by referring to their respective comprehensive health centers. Participants were selected using convenience sampling. Informed written consent was taken from all participants. Then, they were randomly divided into groups of intervention and control (Figure 1).
Method of sampling
Participants were randomly allocated to the groups using special cards that were defined as intervention or control. Then, participants were asked to choose a card to determine their respective groups.
Afterward, the demographic form and the TBQol-v2 were completed through interviews with the members of both groups. Then, patients in the intervention group and their caregivers received three thirty-minute sessions of self-care education. The sessions were organized every other day with the help of an assistant researcher who was competent in the Balochi language. The training sessions were conducted in small groups of 4 to 6 members and included lectures, questions and answers, pamphlets, and educational booklets. The content of these sessions is described in Table 1. During the intervention and two months after, we made weekly phone calls to answer patients’ questions and to ensure observing the instructions by patients. No special training program was held for the control group, and they received only the routine guidelines provided by the health staff. After two months, the questionnaires were completed by both groups again. To do so, patients were invited to refer to their local health centers. If a patient was failed to attend, we met him/her living area. At the end of the study, all educational material was provided to the members of the control group.
Content of the Educational Program
| Details | |
|---|---|
| Session 1 | Presenting the objectives of the training sessions; definition of transmission methods of tuberculosis; symptoms and their control; treatment methods; early diagnosis and prevention; self-care and its dimensions; and How to improve QoL of TB patients. |
| Session 2 | Acceptance of treatment and its effective factors; treatment and referring to medical centers; following a proper medication plan and regular use of medication; and drug side effects and their management. |
| Session 3 | Importance of continuing treatment and its consequences; physical, mental, and psychological rehabilitation; motivation; and returning to normal life. |
Data were analyzed using SPSS version 21. As the data had a normal distribution, Shapiro-Wilk test, independent t-test, paired t-test, and chi-squared test were used. A P value of < 0.05 was considered statistically significant.
4. Results
The mean and standard deviation of patients’ age in the intervention and control groups were 46.78 ± 14.40 and 46.76 ± 15.99 years, respectively. The independent t-test did not show a significant difference between the two groups concerning the age of participants. The demographic characteristics of the participants are provided in Table 2. Besides, the chi-square test did not reveal a statistically significant difference between the two groups concerning gender, marital status, education level, occupation, and ethnicity.
| Variable | Intervention Group | Control Group | Result |
|---|---|---|---|
| Gender | 0.33b | ||
| Female | 34 (61.8) | 29 (52.7) | |
| Male | 21 (38.2) | 26 (47.3) | |
| Total (%) | 55 (100) | 55 (100) | |
| Marital status | 0.42b | ||
| Single | 7 (12.7) | 10 (18.2) | |
| Married | 48 (87.3) | 45 (81.8) | |
| Total (%) | 55 (100) | 55 (100) | |
| Education | 0.86b | ||
| Illitrate | 25 (45.5) | 25 (45.5) | |
| Primary school | 19 (34.5) | 21 (38.2) | |
| High school diploma and above | 11 (20) | 9 (16.3) | |
| Total (%) | 55 (100) | 55 (100) | |
| Occupation status | 0.18b | ||
| Employed | 22 (40) | 26 (47.3) | |
| Unemployed | 33 (60) | 29 (52.7) | |
| Total (%) | 55 (100) | 55 (100) | |
| Ethnicity | 0.65b | ||
| Fars | 13 (23.6) | 22 (40) | |
| Baloch | 42 (76.4) | 33 (60) | |
| Total (%) | 55 (100) | 55 (100) | |
| Main caregiver | 0.88b | ||
| Parent | 27 (49.1) | 25 (45.5) | |
| Sibling | 11 (20) | 13 (23.6) | |
| Child | 17 (30.9) | 17 (30.9) | |
| Total (%) | 55 (100) | 55 (100) |
As shown in Table 3, the mean score of patients’ QoL in the control group before and after self-care education was 67.09 (5.03) and 67.98 (3.68), respectively. The paired t-test indicated no significant difference in this regard (P = 0.15). On the other hand, the mean and standard deviation of patients’ QoL scores in the intervention group before and after self-care education were, respectively, 67.56 (5.99) and 74.84 (4.90), suggesting a significant difference, as shown by paired t-test (P = 0.001). Also, the mean and standard deviation of patients’ QoL scores in the control and intervention groups before self-care education were, respectively, 67.09 (5.03) and 67.56 (5.99), implying no significant difference (P = 0.65). However, the mean and standard deviation in the control and intervention groups after self-care training were 67.98 (3.68) and 74.84 (4.90), respectively, which shows a significant difference (P = 0.001).
Comparison of the Mean Scores of QoL and Its Dimensions in TB Patients Before and After Self-Care Education in the Two Study Groups
| Quality of Life and Its Dimensions | Groupsa | P Value b | |
|---|---|---|---|
| Intervention | Control | ||
| Physical dimension | |||
| Before intervention | 64.30 ± 15.02 | 58.72 ± 12.36 | 0.0.03 |
| After intervention | 66.84 ± 1.35 | 60.24 ± 9.55 | < 0.001 |
| P valuec | 0.02 | 0.39 | |
| Psychological/emotional dimension | |||
| Before intervention | 70.25 ± 18.06 | 71.63 ± 10.97 | 0.0.63 |
| After intervention | 75.92 ± 12.13 | 72.00 ± 15.02 | 0.0.13 |
| P valuec | 0.008 | 0.86 | |
| Functional/independence dimension | |||
| Before intervention | 64.09 ± 12.09 | 65.09 ± 9.69 | 0.0.63 |
| After intervention | 73.63 ± 8.13 | 66.27 ± 10.05 | < 0.001 |
| P valuec | < 0.001 | 0.43 | |
| Social/family dimension | |||
| Before intervention | 67.75 ± 15.59 | 65.21 ± 11.87 | 0.0.33 |
| After intervention | 77.33 ± 9.48 | 65.57 ± 10.48 | < 0.001 |
| P valuec | < 0.001 | 0.86 | |
| Environmental dimension | |||
| Before intervention | 72.84 ± 12.36 | 74.42 ± 10.56 | 0.0.47 |
| After intervention | 84.48 ± 7.80 | 76.48 ± 11.02 | < 0.001 |
| P valuec | < 0.001 | 0.3 | |
| Beliefs and spirituality dimension | |||
| Before intervention | 68.72 ± 16.82 | 72.84 ± 12.42 | 0.14 |
| After intervention | 79.51 ± 11.46 | 73.81 ± 13.07 | 0.01 |
| P valuec | < 0.001 | 0.66 | |
| Total score | |||
| Before intervention | 67.56 ± 5.99 | 67.09 ± 5.03 | 0.65 |
| After intervention | 74.84 ± 4.90 | 67.98 ± 3.68 | < 0.001 |
| P valuec | < 0.001 | 0.15 | |
According to the independent t-test, the mean QoL score in the following subscales differed significantly in the two groups after providing the self-care education: physical (P = 0.001), functional/independence (P = 0.001), social/family (P = 0.001), environmental (P = 0.001), and beliefs and spirituality (P = 0.01); but this difference was not significant in the psychological/emotional subscale (P = 0.86).
The mean score of the physical dimension of [QoL in] the two groups was significantly different before the intervention, and the necessary conditions for using analysis of covariance were met in this study, based on two reasons: the results of Shapiro-Wilk test (statistical = 0.97 and Sig = 0.09) and Levene’s test (F = 1.11, P = 0.1) confirmed the assumptions of approximate normality and consistency of variances, and the homogeneity of regression slope supported that the interaction of the independent variable (group) with the covariate variable (pre-test) (Sig = 0.32) was not significant. The results of covariance analysis, aimed at moderating the effect of pretest scores, showed that the mean score of the physical dimension of [QoL of] patients with pulmonary TB in the two groups was significantly different (P = 0.01) after self-care education.
5. Discussion
This study showed that both groups had a low QoL score before the intervention. In the current study, the physical, functional, independence, social, and family dimensions [of QoL] were more affected by tuberculosis than other dimensions, which is consistent with the results of previous studies. In this regard, Jaber et al. study (26) conducted in Yemen suggested that all eight domains [of QoL] were low at the start of treatment, with the lowest scores were for physical dimension and limited activity due to emotional problems. In Indonesia, Sartika et al. (22) reported that the mean QoL score of TB patients for all dimensions was low, and the physical dimension had the lowest score.
Chung et al. (27) in Taiwan observed that the scores of the physical and social dimensions of TB patients’ QoL significantly declined two months after initiating the treatment but increased during the next six months.
In Iran, Robabi et al. (25), in a study performed in Zahedan, found that various dimensions of patients’ QoL were significantly affected by tuberculosis, and the lowest scores at the beginning of treatment were associated with the functional/independence, physical, and psychological/emotional dimensions. Salehitalia (28), in a study conducted in Shahrekord, reported that the lowest QoL score was for limitations in physical activity due to physical problems and social functioning issues. Darvishpoor Kakhki et al. (16) noted that tuberculosis had a significant negative impact on various domains of patients’ QoL. In this study, the lowest QoL score was related to limitations in playing one’s roles due to physical problems. Mamani et al. (29), in a study conducted in Hamedan showed that all domains of patients’ QoL had significantly lower scores than the control group (healthy individuals), but the scores were significantly improved two months after treatment.
The results also indicated that tuberculosis -from the most to the least- mostly affects the physical, functional/independence, and social/family domains of QoL. Prolonged cough, fever, weakness and fatigue, chest pain, and weight loss are among the most common physical problems caused by TB (2), which in turn reduce the patient’s ability and physical function and pave the way for the emergence of social and family problems (30).
Based on the results, the intervention could significantly improve the QoL of patients in the intervention group, so that the mean score of QoL and its domains were different before and after the intervention. Meanwhile, such an increase was not observed in the control group.
A comparison of patients’ QoL in both groups showed that they were homogeneous concerning the total QoL score before providing the intervention. This comparison also showed a significant difference between the two groups after providing the intervention. Also, a significant difference was found between the two groups in most domains of QoL, including physical, functional/independence, social/family, environmental, and beliefs and spirituality. These findings are consistent with the results of previous studies.
In this regard, Geeravani (31) stated that all domains of TB patients’ QoL before treatment were significantly lower than the control group, but the educational intervention and counseling could gradually promote the QoL.
Kastien-Hilka et al. (21) in South Africa reported that six months after treatment, all aspects of patients’ QoL were improved. The authors also reported a positive association between adherence to the treatment and QoL.
In India, Banerjee (32) reported that directly observed treatment, short-course (DOTS) could improve the QoL of TB patients.
In Kiribati, Li et al. (33) noted that DOTS and self-care training significantly enhanced the QoL of patients with pulmonary TB.
Agrrawal et al. (14) and Saleem et al. (34) concluded that TB negatively affects the QoL of patients, but it can improve quickly and significantly through treatment programs.
In Malaysia, Awaisu et al. (35) found that the intervention group, six months after DOTS and a smoking cessation program, experienced a significantly better QoL than did the group who received routine treatment.
Howyida et al. (36) also concluded that counseling for adult TB patients promoted their self-care abilities and caused a significant difference in the physical, mental, and social status of patients.
A follow-up study in Thailand also reinforced that the highest mean of QoL belonged to patients who were successfully treated (37).
In South Africa, Louw et al. (38) reported a significant improvement six months after treatment in all domains of QoL, except for the energy-fatigue.
Jadgal et al. (23) found that health education based on the health belief model strengthens self-care behaviors and raises the QoL of patients with smear-positive pulmonary TB.
According to these findings, it seems that self-care education can increase patients’ awareness and promote their self-care behaviors, which in turn translates into increased QoL.
Based on the findings of the current study, the intervention could significantly increase QoL scores (in most of the domains) of TB patients, and this increase can be attributed to self-care education. However, no difference was observed in the psychological/emotional domains between the two groups. (Thus, self-care education could not enhance this domain after two months). In this regard, various studies have affirmed that tuberculosis treatment has a greater impact on enhancing the physical dimension rather than the psychological dimension of QoL (39, 40). For example, Louw et al. (38) reported that patients’ QoL, especially in the physical domain, was considerably better six months after initiating the treatment.
Kastien-Hilka et al. (21) concluded that although standard TB treatment improves most domains of QoL, it does not considerably affect patients’ psychological status and social functioning, and these domains remain impaired after treatment.
In the study by Geeravani (31), the psychological and social dimensions of patients’ QoL were more affected by tuberculosis, and it was recommended that to better control the disease, in addition to medication, the psychosocial reactions of patients should be considered in centers providing DOTS services.
In the study by Atif et al. (41), 23% of patients were at risk of depression at the end of treatment. Jaber et al. (26) in Yemen also showed that the mean score of patients’ psychological QoL at the end of treatment was lower than normal, which increased the risk of TB patients towards depression.
In Taiwan, Chung et al. (27) found that the least effect of the TB on patients’ QoL is for psychological and environmental domains.
The study by Salehitalia et al. (28) in Shahrekord, Iran, highlighted the negative effect of long-term treatment of tuberculosis on various areas of QoL, including social and psychological domains.
Since tuberculosis is a contagious disease, friends and family members are less inclined to communicate with patients, which paves the way for their social isolation, loneliness, depression, and psychological problems. Moreover, it worth noting that the psychological domain of QoL is related to people’s attitudes and beliefs, whose change requires deep and long-term cognitive-emotional processes. It seems that, at least in the short term, self-help education cannot cease this process, and using appropriate long-term educational methods with longer follow-up periods to produce such profound behavioral changes is necessary.
Based on the findings, in the control group, the scores related to all domains of QoL were increased in the second stage compared to the first stage, but this change was not statistically significant, which is consistent with the results of previous studies. In the same vein, Atif et al. (41) suggested that although TB treatment improves patients’ perception of health, but it also has negative effects on their QoL. Chung et al. (27) reported that while effective treatment of tuberculosis has positive effects for both overall health and the QoL, special attention should be paid to the side effects of anti-tuberculosis drugs. Dhuria et al. (39) demonstrated that although TB treatment improved different aspects of patients’ QoL, this improved life quality was still lower than the quality of life of the control group (i.e., healthy people).
The current study also had limitations, including the low level of literacy of patients, which probably has affected their learning, and the short duration of the study (two months). In this respect, the authors recommend performing studies with longer periods to measure the effect of self-care education as well as comparing its effects with other methods along with teaching aids; also, it would be desirable to examine the effect of the intervention over longer periods (at least four months).
Given that it is a non-pharmaceutical, non-invasive, and low-cost method, self-care education can be easily taught to [TB] patients and their families to raise their QoL. Based on the results of this study, healthcare workers, including community health nurses, should regard comprehensive self-care education as one of their main tasks. Moreover, they also should assess the educational needs of patients, who are, in fact, the basic elements of the education process, and help them learn how to achieve and maintain maximum health and how to reduce the complications caused by the disease as well as other physical and mental problems.
5.1. Conclusions
Since self-care education can effectively enhance the QoL of TB patients, it is recommended to provide such educations for both treatment and follow-up of these patients along with directly observed treatment, short-course (DOTS).
Acknowledgements
References
-
1.
Tavakoli A. Incidence and Prevalence of Tuberculosis in Iran and Neighboring Countries. Zahedan J Res Med Sci. 2017;19(7). https://doi.org/10.5812/zjrms.9238.
-
2.
WHO. Global tuberculosis report 2019. 2020, [cited 2020 Sep 8]. Available from: https://apps.who.int/iris/bitstream/handle/10665/329368/9789241565714-eng.pdf?ua=1.
-
3.
Endris M, Moges F, Belyhun Y, Woldehana E, Esmael A, Unakal C. Treatment outcome of tuberculosis patients at enfraz health center, northwest ethiopia: a five-year retrospective study. Tuberc Res Treat. 2014;2014:726193. [PubMed ID: 24891948]. [PubMed Central ID: PMC4027020]. https://doi.org/10.1155/2014/726193.
-
4.
Tuberculosis. 2020, [cited 2020 Jul 8]. Available from: http://www.emro.who.int/health-topics/tuberculosis/.
-
5.
The situation of tuberculosis in Iran. 2020, [cited 2020 Jul 8]. Available from: https://www.mehrnews.com/news/4429943.
-
6.
Department of Tuberculosis and Leprosy Control. The incidence of tuberculosis in Iran. 2019, [cited 2020 Jul 8]. Available from: http://tb-lep.behdasht.gov.ir/TB_Situation_in_Iran.aspx.
-
7.
Vecino M, Pasipanodya JG, Slocum P, Bae S, Munguia G, Miller T, et al. Evidence for chronic lung impairment in patients treated for pulmonary tuberculosis. J Infect Public Health. 2011;4(5-6):244-52. [PubMed ID: 22118719]. https://doi.org/10.1016/j.jiph.2011.08.005.
-
8.
WHO. Global Tuberculosis Report. Geneva: World Health Organization; 2015, [cited 2018 Jul 21]. Available from: http://www.apps.who.int/iris/bitstream/1665/191102/1/9789241565059_eng.pdf.
-
9.
Haery SM, Tehrani H, Olyaeimanesh A, Nedjat S. Factors influencing the social health of employees of the ministry of health and medical education in Iran. Iran J Health Educ Health Prom. 2016;3(4):311-8.
-
10.
Aggarwal AN. Health-related quality of life: A neglected aspect of pulmonary tuberculosis. Lung India. 2010;27(1):1-3. [PubMed ID: 20539762]. [PubMed Central ID: PMC2878705]. https://doi.org/10.4103/0970-2113.59259.
-
11.
Wardhana MF, Milanda T, Sumiwi SA. Assessment of Risk Factors of Hepatotoxicity among Tuberculosis Patients. Pharmacol Clin Pharm Res. 2018;3(1). https://doi.org/10.15416/pcpr.v3i1.16450.
-
12.
Dujaili JA, Sulaiman SA, Hassali MA, Awaisu A, Blebil AQ, Bredle JM. Health-related quality of life as a predictor of tuberculosis treatment outcomes in Iraq. Int J Infect Dis. 2015;31:4-8. [PubMed ID: 25486011]. https://doi.org/10.1016/j.ijid.2014.12.004.
-
13.
Masumoto S, Yamamoto T, Ohkado A, Yoshimatsu S, Querri AG, Kamiya Y. Factors associated with health-related quality of life among pulmonary tuberculosis patients in Manila, the Philippines. Qual Life Res. 2014;23(5):1523-33. [PubMed ID: 24264802]. https://doi.org/10.1007/s11136-013-0571-x.
-
14.
Aggarwal AN, Gupta D, Janmeja AK, Jindal SK. Assessment of health-related quality of life in patients with pulmonary tuberculosis under programme conditions. Int J Tuberc Lung Dis. 2013;17(7):947-53. [PubMed ID: 23743314]. https://doi.org/10.5588/ijtld.12.0299.
-
15.
Babikako HM, Neuhauser D, Katamba A, Mupere E. Feasibility, reliability and validity of health-related quality of life questionnaire among adult pulmonary tuberculosis patients in urban Uganda: cross-sectional study. Health Qual Life Outcomes. 2010;8:93. [PubMed ID: 20813062]. [PubMed Central ID: PMC2944342]. https://doi.org/10.1186/1477-7525-8-93.
-
16.
Darvishpoor Kakhki A, Masjedi MR. Factors Associated with Health-Related Quality of Life in Tuberculosis Patients Referred to the National Research Institute of Tuberculosis and Lung Disease in Tehran. Tuberc Respir Dis (Seoul). 2015;78(4):309-14. [PubMed ID: 26508916]. [PubMed Central ID: PMC4620322]. https://doi.org/10.4046/trd.2015.78.4.309.
-
17.
Ansaropour S, Khosrav M, Fouladband F, Hashemia V. Triple components of self-care. Behvarz. 2015;90(25):9-11.
-
18.
Hassani M, Farahani B, Zohour A, Panahi Azar S. Self-care ability based on Orem's theory in coronary artery disease patients. Iran J Critic Care Nurs. 2010;3(2):87-91.
-
19.
Morowatisharifabad M, Rouhani Tonekaboni N. Perceived self-efficacy in self-care behaviors among diabetic patients referring to Yazd Diabetes Research Center. J Birjand Univ Med Sci. 2008;15(4):91-9.
-
20.
Bauer M, Leavens A, Schwartzman K. A systematic review and meta-analysis of the impact of tuberculosis on health-related quality of life. Qual Life Res. 2013;22(8):2213-35. [PubMed ID: 23232952]. [PubMed Central ID: PMC3825536]. https://doi.org/10.1007/s11136-012-0329-x.
-
21.
Kastien-Hilka T, Rosenkranz B, Schwenkglenks M, Bennett BM, Sinanovic E. Association between Health-Related Quality of Life and Medication Adherence in Pulmonary Tuberculosis in South Africa. Front Pharmacol. 2017;8:919. [PubMed ID: 29326591]. [PubMed Central ID: PMC5741974]. https://doi.org/10.3389/fphar.2017.00919.
-
22.
Sartika I, Insani WN, Abdulah R. Assessment of Health-Related Quality of Life among Tuberculosis Patients in a Public Primary Care Facility in Indonesia. J Glob Infect Dis. 2019;11(3):102-6. [PubMed ID: 31543651]. [PubMed Central ID: PMC6733192]. https://doi.org/10.4103/jgid.jgid_136_18.
-
23.
Jadgal K, Zareban I, Alizadeh-Siuki H, Izadirad H. The impact of educational intervention based on health belief model on promoting self-care behaviors in patients with smear-positive pulmonary TB. J Health Educ Health Prom Summer. 2014;2(2):143-52.
-
24.
Chaoyang H, Chongsuvivatwong V, Geater A. Predictors for Quality of life pulmonary Toberculosis Patient in Yunnan Province of China. J Popul Soc Stud. 2004;13(1):77-91.
-
25.
Robabi H, Navidian A, Pishkar Mofrad Z. Quality of life of patients with pulmonary tuberculosis during the course of treatment. J Mazandaran Univ Med Sc. 2012;22(93):104-13.
-
26.
Jaber AA, Khan AH, Syed Sulaiman SA, Ahmad N, Anaam MS. Evaluation of Health-Related Quality of Life among Tuberculosis Patients in Two Cities in Yemen. PLoS One. 2016;11(6). e0156258. [PubMed ID: 27257990]. [PubMed Central ID: PMC4892669]. https://doi.org/10.1371/journal.pone.0156258.
-
27.
Chung WS, Li CR, Liao LY, Yang WT. Quality of life among pulmonary tuberculosis patients under treatment in Eastern Taiwan. Taiwan Gong Gong Wei Sheng Za Zhi. 2014;33(1):23.
-
28.
Salehitali S, Noorian K, Hafizi M, Dehkordi AH. Quality of life and its effective factors in tuberculosis patients receiving directly observed treatment short-course (DOTS). J Clin Tuberc Other Mycobact Dis. 2019;15:100093. [PubMed ID: 31720420]. [PubMed Central ID: PMC6830121]. https://doi.org/10.1016/j.jctube.2019.100093.
-
29.
Mamani M, Majzoobi MM, Ghahfarokhi SM, Esna-Ashari F, Keramat F. Assessment of Health-related Quality of Life among Patients with Tuberculosis in Hamadan, Western Iran. Oman Med J. 2014;29(2):102-5. [PubMed ID: 24715935]. [PubMed Central ID: PMC3976728]. https://doi.org/10.5001/omj.2014.25.
-
30.
Aggarwal AN. Quality of life with tuberculosis. J Clin Tuberc Other Mycobact Dis. 2019;17:100121. [PubMed ID: 31788563]. [PubMed Central ID: PMC6880022]. https://doi.org/10.1016/j.jctube.2019.100121.
-
31.
Geeravani M. Studies on medication adherence and quality of life in Tuberculosis patients. 2020, [cited 2020 Jun 13]. Available from: https://www.longdom.org/proceedings/studies-on-medication-adherence-and-quality-of-life-in-tuberculosis-patients-15646.html.
-
32.
Banerjee S, Bandyopadhyay K, Taraphdar P, Dasgupta A. Effect of DOTS on quality of life among tuberculosis patients: A follow-up study in a health district of Kolkata. J Family Med Prim Care. 2019;8(3):1070-5. [PubMed ID: 31041253]. [PubMed Central ID: PMC6482798]. https://doi.org/10.4103/jfmpc.jfmpc_347_18.
-
33.
Li CT, Chu KH, Reiher B, Kienene T, Chien LY. Evaluation of health-related quality of life in patients with tuberculosis who completed treatment in Kiribati. J Int Med Res. 2017;45(2):610-20. [PubMed ID: 28415942]. [PubMed Central ID: PMC5536668]. https://doi.org/10.1177/0300060517694491.
-
34.
Saleem S, A. Malik A, Ghulam A, Ahmed J, Hussain H. Health-related quality of life among pulmonary tuberculosis patients in Pakistan. Qual Life Res. 2018;27(12):3137-43. [PubMed ID: 30073472]. https://doi.org/10.1007/s11136-018-1954-9.
-
35.
Awaisu A, Haniki Nik Mohamed M, Noordin NM, Muttalif AR, Aziz NA, Syed Sulaiman SA, et al. Impact of connecting tuberculosis directly observed therapy short-course with smoking cessation on health-related quality of life. Tob Induc Dis. 2012;10:2. [PubMed ID: 22373470]. [PubMed Central ID: PMC3305504]. https://doi.org/10.1186/1617-9625-10-2.
-
36.
Howyida S, Heba A, Abeer Y. Effect of Counseling on Self-Care Management among Adult Patients with Pulmonary Tuberculosis. Life Sci J. 2012;9(1).
-
37.
Kittikraisak W, Kingkaew P, Teerawattananon Y, Yothasamut J, Natesuwan S, Manosuthi W, et al. Health related quality of life among patients with tuberculosis and HIV in Thailand. PLoS One. 2012;7(1). e29775. [PubMed ID: 22253777]. [PubMed Central ID: PMC3256183]. https://doi.org/10.1371/journal.pone.0029775.
-
38.
Louw JS, Mabaso M, Peltzer K. Change in Health-Related Quality of Life among Pulmonary Tuberculosis Patients at Primary Health Care Settings in South Africa: A Prospective Cohort Study. PLoS One. 2016;11(5). e0151892. [PubMed ID: 27137914]. [PubMed Central ID: PMC4854485]. https://doi.org/10.1371/journal.pone.0151892.
-
39.
Dhuria M, Sharma N, Narender Pal S, Ram Chander J, Saha R, Gopal Krishan I. A study of the impact of tuberculosis on the quality of life and the effect after treatment with DOTS. Asia Pac J Public Health. 2009;21(3):312-20. [PubMed ID: 19443879]. https://doi.org/10.1177/1010539509336242.
-
40.
Kruijshaar ME, Lipman M, Essink-Bot ML, Lozewicz S, Creer D, Dart S, et al. Health status of UK patients with active tuberculosis. Int J Tuberc Lung Dis. 2010;14(3):296-302. [PubMed ID: 20132620].
-
41.
Atif M, Sulaiman SA, Shafie AA, Asif M, Sarfraz MK, Low HC, et al. Impact of tuberculosis treatment on health-related quality of life of pulmonary tuberculosis patients: a follow-up study. Health Qual Life Outcomes. 2014;12:19. [PubMed ID: 24528499]. [PubMed Central ID: PMC3925792]. https://doi.org/10.1186/1477-7525-12-19.
