Abstract
Background:
The choice of treatment for benign prostatic hyperplasia (BPH) and kidney stone disease (KSD) impacts the attainment of successful ageing and the level of patient care required in the long-term. Medications and surgeries typically used for these conditions have serious side effects and can interfere with healthy aging.Objectives:
This study assesses the impact of Dr Allen’s Therapeutic devices (DATD) and thermobalancing therapy® (TT) on the ageing process of people with BPH and KSD.Methods:
This study evaluated the outcomes of a clinical trial investigating the dynamics of symptoms and parameters in 124 male patients with BPH who used DATD as a monotherapy for six months at home and compared the results with a control group comprising 124 BPH patients who did not receive treatment with DATD. Furthermore, five case studies were randomly selected for assessment from 10-year empirical observations of patients with KSD treated with DATD.Results:
DATD with TT reduced prostate volume (PV) from 45 mL to 31 mL (P < 0.001) and reduced urinary symptoms score from 14.2 to 4.9 (P < 0.001). It also improved quality of life (QoL) as measured by the reduction in the International Prostate Symptom score (I-PSS) from 3.9 to 1.3 (P < 0.001), while the control group showed no positive changes. DATD with TT dissolved kidney stones without renal colic in all patients. No side effects were observed.Conclusions:
Using DATD and TT to treat BPH and KSD demonstrated high efficacy, safety, and easy disease management at home. In contrast, medications and surgeries for BPH and KSD often lead to sexual dysfunction, depression, hypertension, chronic kidney failure, and other morbidities, requiring an increased care level in the long-term. Thus, DATD and TT generate high treatment efficacy with lower exposure to coronavirus, reduce long-term care needs, and are vital to attaining successful ageing and longevity.Keywords
Thermobalancing Therapy Dr Allen’s Therapeutic Devices Ageing Longevity Coronavirus Benign Prostatic Hyperplasia Kidney Stone Disease Quality of Life
1. Background
Improved care for ageing individuals ultimately brings positive changes to their physical and psychosocial function. It has been observed that chronic diseases are closely linked to depressive symptoms in middle-aged and elderly people and can worsen their physical and psychosocial condition (1). However, most people with chronic diseases have unrealistically optimistic expectations of their prognosis (2). Therefore, a more active involvement of patients and their families in managing chronic diseases is necessary (3). Moreover, the means for effective disease management at home can improve treatment outcomes and reduce patients’ care needs in the long-term.
When treating urological conditions during the coronavirus crisis, two main recommendations are made. First, during the pandemic, patients with benign prostatic hyperplasia (BPH) should not undergo surgery, unless they require hospitalization due to an emergency, such as hematuria and clot retention. Second, all kidney stone disease (KSD) surgeries should be suspended, apart from emergency cases of patients with urolithiasis (4).
At the same time, surgical procedures are typically chosen by urologists as preferred treatment options for BPH. Adverse outcomes after various BPH surgeries, however, indicate the need for conducting medical treatments, which reduce the use of surgical interventions (5, 6).
One of the most commonly prescribed drugs for enlarged prostate is tamsulosin, the α-blocker with the highest persistence rate when compared to other α-blockers (7). Alarmingly, α-blockers produce troubling sexual side effects, including ejaculatory dysfunction, and do not provide adequate performance in the long-term (8). Therefore, enzyme inhibitors, namely 5-alpha-reductase inhibitors, became popular as a monotherapy or in combination with α-blockers, although they can lead to sexual dysfunction and depression even after drug discontinuation (9, 10).
Standard treatments for patients with nephrolithiasis are various surgical kidney stone removals. These surgeries include extracorporeal shock wave lithotripsy (ESWL) and percutaneous nephrolithotomy (PCNL). Unfortunately, these surgeries frequently cause serious side effects such as bleeding and infection (11), trauma of adjacent organs (12), hypertension, diabetes, and chronic kidney disease (13, 14).
Dr Allen’s Therapeutic devices (DATD) and thermobalancing therapy® (TT) have been patented in the USA as Therapeutic Device and Method (15). The results of 10-year-long observations on the use of DATD with TT as a physical monotherapy in people with KSD revealed their capacity to dissolve various types and sizes of kidney stones without pain, renal colic, and adverse events. The use of DATD with TT as a monotherapy in men over 55 years of age with BPH showed positive dynamics of clinical symptoms (16). It has also been discovered that DATD treats chronic prostatitis, which often accompanies BPH (17, 18).
As the population ages and individuals suffer from multiple illnesses or comorbidities, it is imperative that the various health care providers address the adverse effects of standard treatments in a timely and effective manner (19). The side effects of medications and surgeries used to treat urinary stones and BPH increase the number of chronic conditions that require additional treatment, which impedes successful ageing. Given the potential for side effects of treating chronic diseases, researchers and healthcare professionals must work together to ease the burden of treatment and optimise health outcomes (20).
A study of medical therapies for BPH, with the focus on the effects of different medications on sexual function, showed that α-blockers cause ejaculatory dysfunction at a rate of 30%. In comparison, the 5α-reductase inhibitor finasteride causes problems with erection (15.8%), ejaculation (7.7%), and libido (5.4%) (21). It has been observed that the physical health of BPH patients after a prostate surgery was poor, and many of them were experiencing moderate lower urinary tract symptoms (LUTS), sexual dysfunction, and anxiety (22).
The undesirable complications described above cause well-documented side effects on men’s quality of life (QoL) and, therefore, on their normal ageing process and longevity. Thus, the optimal treatment must demonstrate efficacy and safety with the least possible side effects.
2. Objectives
This study aimed to assess the impact of using DATD on the ageing process in patients with BPH and KSD based on the dynamics of symptoms and treatment outcomes, and to assess the role of TT in the provision of high-quality healthcare for successful ageing.
3. Methods
3.1. Study Protocol
The DATD was registered with the Medicines and Healthcare Products Regulatory Agency in Great Britain in 2010 as a class 1 medical device. The device is non-invasive and does not have a measuring function. In addition, it is permitted to use DATD at home. Empirical observations stretching over a 10-year-long period between 2010 and 2020 involving men and women with KSD and men with BPH receiving treatment with DATD and TT have been conducted. During 2013 - 2015, the Yerevan State Medical University’s Department of Urology conducted a clinical trial on DATD and TT in men with BPH. The University’s Ethics Committee approved the design of this study. The controlled clinical trial was registered at the German Clinical Trials Register (DRKS) of the World Health Organisation (WHO). The effect of DATD in men with BPH was compared with data obtained from the untreated control group by calculating prostate volume (PV), urinary symptoms, and QoL. A group of patients consisting of men and women with kidney stones and treated with DATD was also observed at the Department of Urology. The obtained data included the dynamics of KSD symptoms, kidney function, and the treatment effect of DATD on kidney stones.
3.2. Study Design
In this study, two distinct patient groups treated with DATD were assessed; the first group consisted of male patients with BPH, while the second group comprised of men and women with KSD.
The assessment of patients with BPH involved 124 male patients with enlarged prostate who used DATD for six months. Their clinical parameters were examined before and after this treatment period. The data were compared with the control group, i.e., with clinical parameters of other 124 men with BPH who were in watchful waiting. The dynamics of symptoms and QoL were measured by the International Prostate Symptom Score (I-PSS), while PV was measured with ultrasound. The I-PSS consisted of an 8-item questionnaire, in which seven questions measured urinary symptoms, and evaluated incomplete bladder emptying, frequency, intermittency, urgency, weak stream, straining, and nocturia on the scale of 0 - 35, with the higher score describing higher severity of these urinary symptoms. It also included one more question that measured QoL on the scale of 0–6, with the lower score describing a better QoL. The standard ellipsoid formula, calculated as length × width × height × 0.52, was used to determine PV. The parameters were compared between the treatment and control groups.
The assessment of patients with KSD involved five case studies of men and women with kidney stones randomly selected from a group of patients with various sizes and types of kidney stones and treated with DATD. The duration of their treatment with DATD varied on a case-by-case basis. Patient observations before and after treatment with DATD were recorded. The data included patient age, gender, history of KSD before treatment, dynamics of KSD symptoms (renal colic and pain), kidney function, and the treatment effect of DATD on kidney stones.
3.3. Patient Selection and Evaluation
In this study, 124 men with LUTS due to BPH with PV < 60 mL who received treatment with DATD were investigated. Baseline evaluations consisted of medical history, complete physical examination, digital rectal examination, serum biochemistry, measurement of prostate-specific antigen and electrolytes, urinalysis, and renal function tests. Evaluations were recorded at baseline and six months after treatment with DATD. Baseline evaluation demonstrated that characteristics of men were identical between treatment and control groups.
Also, five patients with nephrolithiasis who received treatment with DATD were investigated. The samples with the age range of 23 - 69 years were randomly selected from a group of men and women treated with DATD at some point during a 10-year period between 2010-2020. The males constituted 80% (n = 4), while females constituted 20% (n = 1) of cases. Baseline evaluations consisted of medical history, symptoms of kidney stones, and size of kidney stones. Evaluations were obtained at baseline and after treatment with DATD.
3.4. Statistical Analysis
Statistical analysis was performed on the data obtained from the controlled clinical trial. Since the independent-samples t-test and paired-samples t-test are suitable only for interval and ratio data, the Wilcoxon signed-rank test was employed. A P-value < 0.05 was considered as significant. Statistical analysis was carried out using SPSS v22 (IBM, Armonk, NY, USA).
3.5. Dr Allen’s Therapeutic Device
Dr Allen’s Therapeutic Device (DATD) consists of a supporting apparel, such as a belt, with one or more supporting pockets for one or more thermoelements. Such design applies the thermoelements topically to the area of the skin in projection of the affected organs. The thermoelements consist of a special mixture of waxes. For treating prostate, the thermoelements are applied to the coccyx area (Figure 1). For treating kidneys, the thermoelements are applied to the area of the back in projection of the kidneys (Figure 2). The thermoelements accumulate the emitted body heat and maintain the temperature constant, while worn on the body. The material of the DATD and its design ensure a comfortable and adjustable fit for its users.
DATD for prostate treatment covers the low back/coccyx area

DATD for kidney treatment covers the area of the back in projection of the kidneys

4. Results
4.1. BPH Treatment with DATD
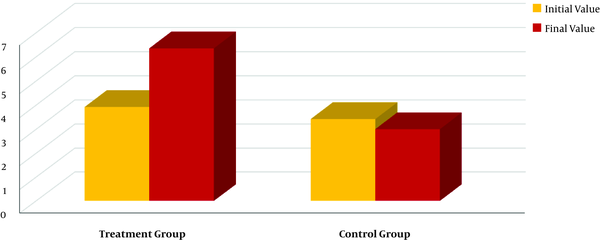
The QoL due to urinary symptoms (UrS) score was measured by the International Prostate Symptom Score (I-PSS). In this study, 124 men with BPH were assessed before and after the 6-month course of DATD with TT and the results were compared with 124 men with BPH in the control group. In the treatment group, the I-PSS QoL due to UrS score decreased from 3.92 to 1.49 (P < 0.001), indicating the increase in QoL by 62%. In the control group, the I-PSS QoL due to UrS score increased from 3.42 to 3.83 (P < 0.01), demonstrating the reduction of QoL by 12%. These results demonstrated that DATD with TT significantly improved QoL (Figure 3).
The dynamics of the I-PSS QoL score after six months of DATD with TT in the treatment group and after six months of watchful waiting in the control group
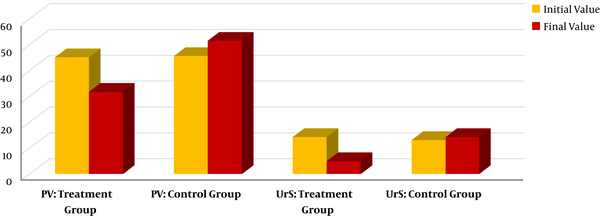
Other parameters that were assessed during the clinical trial were PV (in mL) and UrS measured by the I-PSS. These parameters were assessed in 124 men with BPH before and after the 6-month course of DATD with TT and compared with 124 men with BPH in the control group. In the treatment group, PV decreased from 45.1 mL to 31.8 mL (P < 0.001) and the UrS score decreased from 14.3 to 4.9 (P < 0.001). In the control group, changes were either insignificant or worsened. These results demonstrated that DATD with TT significantly reduced PV and UrS (Figure 4).
The changes in the I-PSS scores showing the dynamics of PV (in mL) and UrS after six months of DATD with TT in the treatment group and watchful waiting in the control group
4.2. KSD or Nephrolithiasis Treatment with DATD
KSD history and symptoms, including renal colic, and the size of kidney stones were the parameters assessed during the evaluation of five randomly selected cases. DATD with TT successfully dissolved kidney stones ranging in size between 6 mm and 5 cm. The symptomatic relief occurred within the first few weeks of therapy. No renal colic and other symptoms of kidney stones were experienced by patients during the treatment with DATD and TT. The improvement of kidney function was also observed. While the age of the selected patients with nephrolithiasis ranged from 23 to 69 years, it is likely that younger and older men and women would respond to the treatment with DATD and TT similarly. The efficacy of this therapy was evident even in patients with chronic KSD history (20 - 30 years) (Table 1).
Results of Five Cases with Nephrolithiasis Treated with DATD and TT
| Patient | Results of Five Cases with Nephrolithiasis Treated with DATD and TT | ||||||
|---|---|---|---|---|---|---|---|
| Age | Gender | History of Kidney Stone Disease (KSD) | Renal Colic Incidence | Prior Treatments | Treatment with DATD and TT: Duration | Treatment with DATD and TT: Outcomes | |
| A | 69 | Male | 5-year history of KSD in both kidneys, 5 cm stone in left kidney | 1 - 2 times a year | no | 2-year use of DATD (2010-2011) | 5 cm kidney stone dissolved, no renal colic during or after treatment |
| B | 58 | Male | 30-year history of KSD, 3 cm stone, chronic kidney disease (CKD) | 1 - 2 times a year | 2 prior lithotripsies | 9-month use of DATD (2014) | 3 cm kidney stone dissolved, no renal colic during or after treatment, kidney function improved |
| C | 44 | Female | 20-year history of chronic KSD | Annually | no | 5-month use of DATD (2016) | Pain and other symptoms resolved within 2 weeks, no renal colic during and after treatment |
| D | 41 | Male | 5-month history of diagnosed KSD | 1 renal colic episode, severe | no | 6-month use of DATD (2010) | Some twinges during first 2 - 3 months, no recurrences since, no renal colic |
| E | 23 | Male | 8-year history of KSD in both kidneys, 6 mm stone in left kidney | Annually | 2 prior lithotripsies | 6-month use of DATD (2018 - 2019) | 6 mm kidney stone dissolved, no renal colic during or after treatment |
5. Discussion
5.1. Importance of DATD for the Ageing Population
According to our results, the DATD significantly improved the QoL in men with BPH, while the QoL score deteriorated without this treatment. This QoL improvement was associated with a decrease in the size of the enlarged prostate resulting in the relief of LUTS. In patients with nephrolithiasis, the use of DATD dissolved kidney stones gradually without renal colic, side effects, and complications. TT demonstrated high efficacy in men and women of all ages with kidney stones of various sizes (small and large), with nephrolithiasis lasting from a few months to over 30 years. Thus, DATD with TT can provide an effective innovative treatment for people with BPH and KSD and contribute to their successful ageing.
The effectiveness of DATD is essential as it addresses the health concerns of the growing ageing population. For instance, BPH with LUTS is a common non-malignant disease in older men: nearly one in four men will suffer from BPH during their lifetime (23). In the case of KSD, a population-based study showed that the proportion of men with kidney stones remained stable for ten years, increasing from 82 to 83 per 100,000, while the number of women, as well as the number of urolithiasis patients over 64 years of age, significantly increased (24). In addition, with age, the prevalence of kidney stones in humans increases in almost all countries (25).
5.2. Treatment of the Cause of BPH and KSD with DATD and TT
DADT offers a new physiotherapeutic approach to the treatment of BPH and KSD. In this respect, a recent study on thermobalancing therapy and Dr Allen’s Device showed that the unique design of DATD utilises the emitted body heat for the reduction of the abnormal size of the enlarged or inflamed prostate gland and LUTS (26). These positive changes in clinical symptoms and parameters are achieved by tackling the cause of common urological conditions.
The pathology emerges as a result of a chain of processes at the capillary level. A progressive increase of pressure in the tissue of the affected organ, whether the prostate or the kidneys, due to the pathological activity of capillaries plays the leading role in the development of their chronic diseases (27). As described by physiologists, the constriction of capillaries in response to various triggers is associated with the formation of local hypothermia. It leads to the spontaneous expansion of the capillary net, which causes abnormal pressure in the organ, its dysfunction and, consequently, a chronic disease. These changes in the prostate gland or the kidneys lead to chronic pelvic pain, prostate inflammation or prostate enlargement, and the formation of kidney stones.
The novel treatment with DATD is aimed at the cause of these chronic diseases. Its innovative design accumulates the emitted body heat and uses it as the source of energy to then spread it to the affected prostate or kidneys, terminating the focal hypothermia in their tissues. Gradually, this therapy relieves pressure in the tissue terminating the symptoms (28, 29).
5.3. Side Effects of Standard Treatments for BPH
It is known that the prevalence of BPH increases with age (30). This health condition is very common in ageing men and can affect individuals and their families (31). At the same time, BPH is a non-life-threatening condition, so the aspect of treatment safety should be prioritised. Most urologists, however, do not discuss the pros and cons of standard medical treatments for BPH with their patients and do not present alternative options to them (32).
Additionally, standard BPH drugs have serious side effects, especially in the long-term, and do not provide an acceptable performance (33, 34). Moreover, none of the new drugs or combinations of drugs for the treatment of LUTS associated with BPH showed that the results were superior to conventional drugs, i.e., α-blockers and 5-alpha reductase inhibitors (35). Therefore, watchful waiting was introduced in the guidelines for treating BPH (36).
Polypharmacy and the increased use of medications is a growing problem, especially among people over 65, and has many negative consequences, such as a higher risk of adverse reactions to drugs. It has led to the introduction of a comprehensive geriatric assessment, which is effective in reducing the number of daily doses of drugs by stopping inappropriate or unnecessary drugs (37). As DATD can be used as an effective and safe monotherapy, it should be included in the management guidelines for BPH that, in turn, can decrease use of drugs and surgeries, increasing the healthy lifespan of ageing men (38, 39).
5.4. Side Effects of Standard Treatments for KSD
The KSD affects approximately one in 13 women and one in seven men, becoming increasingly common across the older population, which represents nearly 20% of all stone formers (40). Age, together with male gender and obesity, might be independent risk factors for the development of nephrolithiasis (41). It should be noted that urolithiasis is related to an increased risk of coronary heart disease and stroke; moreover, this association increases with age (42).
ESWL and PCNL are responsible for severe bleeding, infection, sepsis, hypertension, damages of other organs, and diabetes. In many cases, additional surgical procedures are needed. Moreover, recurrence of kidney stones reaches over 50% after five years from the first stone, and 75% within 25 years (43). Recurrent renal colic is associated with the symptoms of both anxiety and depression (44). Therefore, non-surgical management of urolithiasis is needed (45).
Dissolving kidney stones with DATD represents a new physiotherapeutic approach, which is not associated with renal colic and any adverse effects. The choice of this innovative treatment improves patients’ QoL, ultimately leading to successful ageing and increased longevity. Therefore, DATD with TT should be introduced into the healthcare system as a standard treatment for KSD, thereby preserving human well-being and supporting active ageing (46).
5.5. The Role of DATD with TT in Patient Protection from Coronavirus (COVID-19)
The standard strategies of urology care have been affected by SARS-COV2 infection (COVID-19), as most urological patients are older than 65 and belong to the higher risk group during the coronavirus pandemic. Many urological procedures, such as prostate biopsies, urodynamics, cystoscopy, and intravesical treatment, are invasive and performed at hospitals. Therefore, most surgeries for urolithiasis and BPH, both of which are non-cancerous chronic conditions, are elective and can be delayed (47).
The chance of a male with BPH and LUTS experiencing acute urinary retention is approximately 1 % per year, with a similar risk of developing infections. Therefore, given the low risk of adverse events and the high risks associated with COVID-19, it is reasonable to monitor BPH and KSD symptom progression without active interventions (48). Urinary stone disease also represents a benign condition. Therefore, renal colic patients should be managed conservatively as much as possible, while scheduled surgeries for kidney stone patients should be carefully sorted according to surgical priority (49).
Patients with urolithiasis and BPH and affected by the complications of drugs and surgery are likely to age faster. The ageing process is accompanied by the gradual development of a chronic subclinical systemic inflammation (inflamm-aging). It is also associated with acquired immune system impairment (immune senescence). Both of these factors explain why older men with age-related diseases are most likely to be affected by the adverse outcomes of COVID-19 (50).
The COVID-19-related mortality rates of older men are higher compared to older women and people at all ages (51). Elderly patients with BPH are especially vulnerable during a pandemic, so it is imperative to take preventive measures and choose an at-home treatment whenever possible. A study showed that out of 18 patients with BPH who were admitted and treated at a hospital, 10 (55.5%) men contracted the coronavirus, two of whom were transferred to the intensive care unit and one patient died (52).
Given that no side effects are associated with the use of DATD, in contrast to what is routinely expected from BPH drugs and surgeries, DATD and TT should be recommended as the first-line treatment for men with LUTS due to BPH, in order to improve men’s health and well-being. DATD reduces the need for long-term courses of medications, and allows to decrease patients’ visits to hospitals, diminishing the risks of contracting a viral infection during a coronavirus outbreak (53).
The demonstrated safety and effectiveness of DATD for the treatment of BPH stem from its innovatively designed property to provide continuous heat exposure to the target area without exceeding the normal body temperature. This TT terminates the trigger responsible for the development and progression of BPH, namely focal hypothermia (54). Thus, by tackling the cause of chronic KSD and BPH, this physiotherapeutic therapy ought to be used as the preferred first-line treatment during the COVID-19 or other pandemics (55).
5.6. Conclusions
The choice of inappropriate or unnecessary treatment for BPH and KSD impedes successful ageing and undoubtedly shortens the healthy lifespan of the affected individuals. In BPH patients, the use of DATD with TT reduces PV, and improves LUTS and QoL. In KSD patients, the use of DATD with TT dissolves kidney stones without renal colic. Improving physical and psychosocial functions in patients with the innovative TT and DATD has a positive effect on the ageing process. Furthermore, the disease management with DATD at home allows the reduction of patients’ hospital visits and is a way to protect people from the spread of viral infections. This is particularly important during a coronavirus or other pandemics, as COVID-19 and other viral infections are especially dangerous for the elderly. The safety and effectiveness of DATD and TT suggest that they ought to be used as the first-line treatment for BPH and KSD contributing to successful ageing and longevity.
Acknowledgements
References
-
1.
Seo J, Choi B, Kim S, Lee H, Oh D. The relationship between multiple chronic diseases and depressive symptoms among middle-aged and elderly populations: results of a 2009 korean community health survey of 156,747 participants. BMC Public Health. 2017;17(1):844. [PubMed ID: 29070021]. [PubMed Central ID: PMC5657127]. https://doi.org/10.1186/s12889-017-4798-2.
-
2.
Hole B, Salem J. How long do patients with chronic disease expect to live? A systematic review of the literature. Clin Med (Lond). 2016;16 Suppl 3. s32. [PubMed ID: 27252336]. [PubMed Central ID: PMC4989951]. https://doi.org/10.7861/clinmedicine.16-3-s32.
-
3.
Whitehead L, Jacob E, Towell A, Abu-Qamar M, Cole-Heath A. The role of the family in supporting the self-management of chronic conditions: A qualitative systematic review. J Clin Nurs. 2018;27(1-2):22-30. [PubMed ID: 28231630]. https://doi.org/10.1111/jocn.13775.
-
4.
Carneiro A, Wroclawski ML, Nahar B, Soares A, Cardoso AP, Kim NJ, et al. Impact of the COVID-19 Pandemic on the Urologist's clinical practice in Brazil: a management guideline proposal for low- and middle-income countries during the crisis period. Int Braz J Urol. 2020;46(4):501-10. [PubMed ID: 32271512]. [PubMed Central ID: PMC7239291]. https://doi.org/10.1590/S1677-5538.IBJU.2020.04.03.
-
5.
Robert G, Descazeaud A, de la Taille A. Lower urinary tract symptoms suggestive of benign prostatic hyperplasia: who are the high-risk patients and what are the best treatment options? Curr Opin Urol. 2011;21(1):42-8. [PubMed ID: 21045706]. https://doi.org/10.1097/MOU.0b013e32834100b3.
-
6.
Cindolo L, Pirozzi L, Fanizza C, Romero M, Sountoulides P, Roehrborn CG, et al. Actual medical management of lower urinary tract symptoms related to benign prostatic hyperplasia: temporal trends of prescription and hospitalization rates over 5 years in a large population of Italian men. Int Urol Nephrol. 2014;46(4):695-701. [PubMed ID: 24136187]. https://doi.org/10.1007/s11255-013-0587-8.
-
7.
Moon HW, Yang JH, Choi JB, Bae WJ, Cho HJ, Hong SH, et al. Prescription pattern of alpha-blockers for management of lower urinary tract symptoms/benign prostatic hyperplasia. Sci Rep. 2018;8(1):13223. [PubMed ID: 30185936]. [PubMed Central ID: PMC6125595]. https://doi.org/10.1038/s41598-018-31617-w.
-
8.
Gacci M, Ficarra V, Sebastianelli A, Corona G, Serni S, Shariat SF, et al. Impact of medical treatments for male lower urinary tract symptoms due to benign prostatic hyperplasia on ejaculatory function: a systematic review and meta-analysis. J Sex Med. 2014;11(6):1554-66. [PubMed ID: 24708055]. https://doi.org/10.1111/jsm.12525.
-
9.
Traish AM. The Post-finasteride Syndrome: Clinical Manifestation of Drug-Induced Epigenetics Due to Endocrine Disruption. Curr Sex Health Rep. 2018;10(3):88-103. https://doi.org/10.1007/s11930-018-0161-6.
-
10.
Giatti S, Diviccaro S, Panzica G, Melcangi RC. Post-finasteride syndrome and post-SSRI sexual dysfunction: two sides of the same coin? Endocrine. 2018;61(2):180-93. [PubMed ID: 29675596]. https://doi.org/10.1007/s12020-018-1593-5.
-
11.
Skolarikos A, Alivizatos G, de la Rosette J. Extracorporeal shock wave lithotripsy 25 years later: complications and their prevention. Eur Urol. 2006;50(5):981-90. discussion 990. [PubMed ID: 16481097]. https://doi.org/10.1016/j.eururo.2006.01.045.
-
12.
Marinkovic SP, Marinkovic CM, Xie D. Spleen injury following left extracorporeal shockwave lithotripsy (ESWL). BMC Urol. 2015;15:4. [PubMed ID: 25972225]. [PubMed Central ID: PMC4429660]. https://doi.org/10.1186/1471-2490-15-4.
-
13.
Krambeck AE, Gettman MT, Rohlinger AL, Lohse CM, Patterson DE, Segura JW. Diabetes mellitus and hypertension associated with shock wave lithotripsy of renal and proximal ureteral stones at 19 years of followup. J Urol. 2006;175(5):1742-7. [PubMed ID: 16600747]. https://doi.org/10.1016/S0022-5347(05)00989-4.
-
14.
Malik I, Wadhwa R. Percutaneous Nephrolithotomy: Current Clinical Opinions and Anesthesiologists Perspective. Anesthesiol Res Pract. 2016;2016:9036872. [PubMed ID: 27110239]. [PubMed Central ID: PMC4826713]. https://doi.org/10.1155/2016/9036872.
-
15.
Allen S, Adjani A. Therapeutic Device and Method, United States Patent and Trademark Office. US; 2016. Report No.: Patent No: US 9,408,744 B2.
-
16.
Allen S, Adjani A. Benign Prostatic Hyperplasia Treatment with New Physiotherapeutic Device. Urol J. 2015;12(5):2371-6. [PubMed ID: 26571324].
-
17.
Allen S, Aghajanyan IG. New Independent Thermobalancing Treatment with Therapeutic Device for Chronic Prostatitis/Chronic Pelvic Pain Syndrome. Nephro Urol Mon. 2017;9(2). https://doi.org/10.5812/numonthly.44694.
-
18.
Allen S. Personalized care using thermobalancing therapy can help men with chronic prostatitis and chronic pelvic pain to recover. Pers Med Univ. 2019;8:48-52. https://doi.org/10.1016/j.pmu.2019.04.002.
-
19.
Raghupathi W, Raghupathi V. An Empirical Study of Chronic Diseases in the United States: A Visual Analytics Approach. Int J Environ Res Public Health. 2018;15(3). [PubMed ID: 29494555]. [PubMed Central ID: PMC5876976]. https://doi.org/10.3390/ijerph15030431.
-
20.
Sav A, King MA, Whitty JA, Kendall E, McMillan SS, Kelly F, et al. Burden of treatment for chronic illness: a concept analysis and review of the literature. Health Expect. 2015;18(3):312-24. [PubMed ID: 23363080]. [PubMed Central ID: PMC5060781]. https://doi.org/10.1111/hex.12046.
-
21.
Carbone DJ, Hodges S. Medical therapy for benign prostatic hyperplasia: sexual dysfunction and impact on quality of life. Int J Impot Res. 2003;15(4):299-306. [PubMed ID: 12934061]. https://doi.org/10.1038/sj.ijir.3901017.
-
22.
Yim PW, Wang W, Jiang Y, Zakir HA, Toh PC, Lopez V, et al. Health-related quality of life, psychological well-being, and sexual function in patients with benign prostatic hyperplasia after prostatic surgery. Appl Nurs Res. 2015;28(4):274-80. [PubMed ID: 26608425]. https://doi.org/10.1016/j.apnr.2015.02.007.
-
23.
Lee SWH, Chan EMC, Lai YK. The global burden of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: A systematic review and meta-analysis. Sci Rep. 2017;7(1):7984. [PubMed ID: 28801563]. [PubMed Central ID: PMC5554261]. https://doi.org/10.1038/s41598-017-06628-8.
-
24.
Ordon M, Urbach D, Mamdani M, Saskin R, Honey RJ, Pace KT. A population based study of the changing demographics of patients undergoing definitive treatment for kidney stone disease. J Urol. 2015;193(3):869-74. [PubMed ID: 25261806]. https://doi.org/10.1016/j.juro.2014.09.096.
-
25.
Romero V, Akpinar H, Assimos DG. Kidney stones: a global picture of prevalence, incidence, and associated risk factors. Rev Urol. 2010;12(2-3):e86-96. [PubMed ID: 20811557]. [PubMed Central ID: PMC2931286].
-
26.
Allen S. Innovative Thermobalancing therapy and Dr Allen’s Device for the first time employ body energy to treat chronic prostatic diseases effectively. Int J Qual Innovation. 2020;6(1). https://doi.org/10.1186/s40887-020-00035-0.
-
27.
Allen S. The Origin of Chronic Diseases Can Be in Capillary Pathology: An Evidence From Clinical Trials on Thermobalancing Treatment of Prostate Reveals. Ach Life Sci. 2016;10(2):197-202. https://doi.org/10.1016/j.als.2016.11.005.
-
28.
Allen S. The Vascular Factor Plays the Main Role in the Cause of Pain in Men with Chronic Prostatitis and Chronic Pelvic Pain Syndrome: The Results of Clinical Trial on Thermobalancing Therapy. Diseases. 2017;5(4). [PubMed ID: 29117111]. [PubMed Central ID: PMC5750536]. https://doi.org/10.3390/diseases5040025.
-
29.
Allen S. The cause of chronic prostatitis and prostate enlargement is a change in the vascular level and requires similar treatment: innovative Thermobalancing therapy. Innovative J Med Health Sci. 2019;9(2):290-3. https://doi.org/10.15520/ijmhs.v9i2.2453.
-
30.
Egan KB. The Epidemiology of Benign Prostatic Hyperplasia Associated with Lower Urinary Tract Symptoms: Prevalence and Incident Rates. Urol Clin North Am. 2016;43(3):289-97. [PubMed ID: 27476122]. https://doi.org/10.1016/j.ucl.2016.04.001.
-
31.
Mitropoulos D, Anastasiou I, Giannopoulou C, Nikolopoulos P, Alamanis C, Zervas A, et al. Symptomatic benign prostate hyperplasia: impact on partners' quality of life. Eur Urol. 2002;41(3):240-4. discussion 244-5. [PubMed ID: 12180222]. https://doi.org/10.1016/s0302-2838(02)00041-6.
-
32.
Giona S, Ganguly I, Muir G. Urologists' attitudes to sexual complications of LUTS/BPH treatments. World J Urol. 2018;36(9):1449-53. [PubMed ID: 29680951]. https://doi.org/10.1007/s00345-018-2283-x.
-
33.
Gandhi J, Weissbart SJ, Smith NL, Kaplan SA, Dagur G, Zumbo A, et al. The impact and management of sexual dysfunction secondary to pharmacological therapy of benign prostatic hyperplasia. Transl Androl Urol. 2017;6(2):295-304. [PubMed ID: 28540239]. [PubMed Central ID: PMC5422692]. https://doi.org/10.21037/tau.2017.03.57.
-
34.
Traish AM, Mulgaonkar A, Giordano N. The dark side of 5alpha-reductase inhibitors' therapy: sexual dysfunction, high Gleason grade prostate cancer and depression. Korean J Urol. 2014;55(6):367-79. [PubMed ID: 24955220]. [PubMed Central ID: PMC4064044]. https://doi.org/10.4111/kju.2014.55.6.367.
-
35.
Dahm P, Brasure M, MacDonald R, Olson CM, Nelson VA, Fink HA, et al. Comparative Effectiveness of Newer Medications for Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia: A Systematic Review and Meta-analysis. Eur Urol. 2017;71(4):570-81. [PubMed ID: 27717522]. [PubMed Central ID: PMC5337128]. https://doi.org/10.1016/j.eururo.2016.09.032.
-
36.
Gratzke C, Bachmann A, Descazeaud A, Drake MJ, Madersbacher S, Mamoulakis C, et al. EAU Guidelines on the Assessment of Non-neurogenic Male Lower Urinary Tract Symptoms including Benign Prostatic Obstruction. Eur Urol. 2015;67(6):1099-109. [PubMed ID: 25613154]. https://doi.org/10.1016/j.eururo.2014.12.038.
-
37.
Sergi G, De Rui M, Sarti S, Manzato E. Polypharmacy in the elderly: can comprehensive geriatric assessment reduce inappropriate medication use? Drugs Aging. 2011;28(7):509-18. [PubMed ID: 21721596]. https://doi.org/10.2165/11592010-000000000-00000.
-
38.
Aghajanyan IG, Allen S. Positive Response to Thermobalancing Therapy Enabled by Therapeutic Device in Men with Non-Malignant Prostate Diseases: BPH and Chronic Prostatitis. Diseases. 2016;4(2). [PubMed ID: 28933398]. [PubMed Central ID: PMC5456275]. https://doi.org/10.3390/diseases4020018.
-
39.
Allen S, Aghajanyan IG, Schumacher U. Thermobalancing conservative treatment for moderate-to-low-degree lower urinary tract symptoms (LUTS) secondary to prostate enlargement. Cogent Med. 2016;3(1). https://doi.org/10.1080/2331205x.2016.1195067.
-
40.
Kates M, Matlaga BR. Stones in the Elderly. Curr GeriatrRep. 2014;3(1):14-8. https://doi.org/10.1007/s13670-013-0072-3.
-
41.
Moudi E, Hosseini SR, Bijani A. Nephrolithiasis in elderly population; effect of demographic characteristics. J Nephropathol. 2017;6(2):63-8. [PubMed ID: 28491855]. [PubMed Central ID: PMC5418072]. https://doi.org/10.15171/jnp.2017.11.
-
42.
Peng JP, Zheng H. Kidney stones may increase the risk of coronary heart disease and stroke: A PRISMA-Compliant meta-analysis. Medicine (Baltimore). 2017;96(34). e7898. [PubMed ID: 28834909]. [PubMed Central ID: PMC5572031]. https://doi.org/10.1097/MD.0000000000007898.
-
43.
Lu YM, Chien TM, Chou YH, Wu WJ, Huang CN. Is Extracorporeal Shock Wave Lithotripsy Really Safe in Long-Term Follow-Up? A Nationwide Retrospective 6-Year Age-Matched Non-Randomized Study. Urol Int. 2017;98(4):397-402. [PubMed ID: 27732982]. https://doi.org/10.1159/000451005.
-
44.
Diniz DH, Blay SL, Schor N. Anxiety and depression symptoms in recurrent painful renal lithiasis colic. Braz J Med Biol Res. 2007;40(7):949-55. [PubMed ID: 17653448]. https://doi.org/10.1590/s0100-879x2007000700009.
-
45.
Jung H, Andonian S, Assimos D, Averch T, Geavlete P, Kohjimoto Y, et al. Urolithiasis: evaluation, dietary factors, and medical management: an update of the 2014 SIU-ICUD international consultation on stone disease. World J Urol. 2017;35(9):1331-40. [PubMed ID: 28160089]. https://doi.org/10.1007/s00345-017-2000-1.
-
46.
Allen S. Dr Allen’s Therapeutic Devices Should be Implemented in the Healthcare System for the Treatment of Chronic Noncancerous Prostate and Kidney Diseases Saving People’s Well-Being and Money. Ann Mil Health Sci Res. 2018;16(2). https://doi.org/10.5812/amh.81033.
-
47.
Naspro R, Da Pozzo LF. Urology in the time of corona. Nat Rev Urol. 2020;17(5):251-3. [PubMed ID: 32203310]. [PubMed Central ID: PMC7095235]. https://doi.org/10.1038/s41585-020-0312-1.
-
48.
Witherspoon L, Fitzpatrick R, Patel P, Flannigan R, Roberts MT, Krakowsky Y, et al. Clinical pearls to managing men's health conditions during the COVID-19 pandemic. Can Urol Assoc J. 2020;14(5):E161-6. [PubMed ID: 32369009]. [PubMed Central ID: PMC7197963]. https://doi.org/10.5489/cuaj.6631.
-
49.
Proietti S, Gaboardi F, Giusti G. Endourological Stone Management in the Era of the COVID-19. Eur Urol. 2020;78(2):131-3. [PubMed ID: 32303384]. [PubMed Central ID: PMC7195508]. https://doi.org/10.1016/j.eururo.2020.03.042.
-
50.
Bonafe M, Prattichizzo F, Giuliani A, Storci G, Sabbatinelli J, Olivieri F. Inflamm-aging: Why older men are the most susceptible to SARS-CoV-2 complicated outcomes. Cytokine Growth Factor Rev. 2020;53:33-7. [PubMed ID: 32389499]. [PubMed Central ID: PMC7252014]. https://doi.org/10.1016/j.cytogfr.2020.04.005.
-
51.
Promislow DEL. A Geroscience Perspective on COVID-19 Mortality. J Gerontol A Biol Sci Med Sci. 2020;75(9):e30-3. [PubMed ID: 32300796]. [PubMed Central ID: PMC7184466]. https://doi.org/10.1093/gerona/glaa094.
-
52.
Topaktas R, Tokuc E, Ali Kutluhan M, Akyuz M, Karabay E, Caliskan S. Clinical features and outcomes of COVID-19 patients with benign prostatic hyperplasia in ageing male: A retrospective study of 18 cases. Int J Clin Pract. 2020;74(8). e13574. [PubMed ID: 32506768]. [PubMed Central ID: PMC7300559]. https://doi.org/10.1111/ijcp.13574.
-
53.
Allen S, Adjani A. Benign Prostatic Hyperplasia and Chronic Prostatitis Thermobalancing Therapy Can Prevent Sexual Dysfunction and Depression Linked to Medications: Importance During a Pandemic. Andrology. 2020;9:207. https://doi.org/10.35248/2167-0250.2020.9.207.
-
54.
Allen S, Aghajanyan I. Use of thermobalancing therapy in ageing male with benign prostatic hyperplasia with a focus on etiology and pathophysiology. Aging Male. 2017;20(1):28-32. [PubMed ID: 27960590]. https://doi.org/10.1080/13685538.2016.1247151.
-
55.
Allen S. Thermobalancing therapy as a self-management tool. World News of Nat Sci. 2019;23:84-93.
