Abstract
Background:
Renal stone disease is a very common disease, and its lifetime prevalence is 1 - 15%, with a gradual rise in incidence and disease prevalence. There are significant financial implications of its management. Nowadays, for big (typically > 2 cm) renal and upper ureteric stones, PCNL is widely regarded as the first-line treatment. Because most of the intrarenal collecting systems can be accessed by superior calyceal puncture in PCNL, good stone clearance can be achieved. The “Guy’s Stone Score” is a useful technique for categorizing the complexity of PCNL.Objectives:
This study aimed to evaluate the role of Guys Stone Score based on KUB and intravenous urography to predict the success rate, grading, and complexity of PCNL, which are performed via the upper pole access.Methods:
The present prospective, non-randomized observational study was undertaken in the Department of Urology and Renal transplantation, SCBMCH, Cuttack, from 1st November 2017 to 31st October 2019. A total of 104 patients were enrolled in the study in whom PCNL was performed through superior calyceal puncture, based on preoperative intravenous pyelogram. The Guy's Stone Score was calculated, and the complexity of the procedure was graded using radiological studies, then the outcome was determined accordingly.Results:
In this study, 59.6% of the patients had immediate success among them 29.0% had grade 3, and 6.5% had grade 4 GSS. Moreover, 38.4% of the patients had clinically significant residual fragments among them, 75.0% had grade 4, and 20.0% had grade 3 GSS.23% of the patients underwent REDO-PCNL and 11.5% of the patients underwent accesory/ancillary procedure of ESWL.Conclusions:
The present study shows that an intravenous pyelogram-based Guy’s Stone Score (GSS) is an easy-to-use tool in predicting the early success rate and potential difficulties and complications in PCNL performed through superior calyceal puncture.Keywords
Renal Stones Upper Pole Complexity Residual Fragments Success Rate
1. Background
The estimated lifetime prevalence of kidney stone disease is 1 - 15% and varies by the age of life, gender, race, and geographic area (1). Its current treatment options apart from open surgery include percutaneous nephrolithotomy (PCNL), retrograde intra-renal surgery (RIRS), and extracorporeal shock wave lithotripsy (ESWL) (2, 3). Nowadays, for big (typically > 2 cm) renal and upper ureteric stones, PCNL is widely regarded as first-line treatment (4). Success rate and complication rate are assessment parameters of PCNL outcome. The definition of success in PCNL is lack of any residual stone fragments on X-ray or/and computed tomography (CT) or observation of residual fragments (CIRF) that are not clinically significant. The CIRF is an asymptomatic, non-infectious, non-obstructive residual fragment of less than four mm (5).
Because most of the intrarenal collecting systems can be accessed by superior calyceal puncture in PCNL, good stone clearance can be achieved (6). Nowadays, for post-PCNL complications and success prediction, various scoring tools are used, such as Guy’s Stone Scoring (GSS) system (7), STONE nephrolithometry scoring system (8), and CROES (Clinical Research Office of Endourological Society) nomogram (9). In this regard, GSS can be assigned by calculation based on simple X-ray, IVP, and CT scan. Although CT scan provides more accurate details, it is expensive that is associated with higher radiation exposure, and also is not widely available in developing countries. Plain X-ray KUB and IVP are cheap and commonly done in developing countries (4, 10).
2. Objectives
This study is a single institution-based prospective study, which aimed to focus on the association of an intravenous pyelogram (IVP) based GSS with post-superior calyceal puncture PCNL success rates and complications.
3. Methods
This prospective, observational and non-randomized study was done on 104 patients from 1st November 2017 to 31st October 2019. All patients with renal stone who underwent PCNL by upper calyceal access were included in the study. All other patients who were not suitable for operation (Un-controlled blood disorders, high heart/lung risk, sepsis), patients who underwent inferior and middle calyceal access, abnormal renal anatomy, and pediatric patients, were excluded from the study. All included patients were properly evaluated and assigned by Guy’s Stone Score based on IVP. The PCNL was done in prone position with Upper Calyceal Puncture with 18G IP needle under CARM fluoroscopy. Various preoperative and postoperative parameters (age, gender, BMI, comorbidity, history of previous surgery, stone size, stone location, stone laterality, Guy’s stone score, type of puncture, number of tracts, duration of surgery, any intra-operative events, residual fragments, change in hemoglobin and blood transfusion, change in renal parameters, complications according to Clavien-dindo grading, hospital stay, any ancillary procedure, readmission, immediate success) recorded and graded according to GSS.
Based on stone burden and the anatomy, Thomas et al. (7) graded “Guy’s Stone Score” into the following four groups: Grade I: Single calculous in the middle/inferior pole or single calculus in renal pelvis with simple anatomy. Grade II: Single calculous in superior pole or multiple calculi in patients with simple anatomy/single calculous in patients with abnormal anatomy. Grade III: Multiple calculi in patients with abnormal anatomy/calyceal diverticular stone/partial Staghorn stone. Grade IV: Staghorn stone/any type of stone in patients with spinal injury or spina bifida.
Possible pulmonary complications were evaluated by postoperative chest radiographs in recovery room. Postoperative X-ray KUB radiographs were also obtained in all cases and re-look PCNL, or any further procedure was decided based on that. Patients were usually discharged after 48 h with DJ stent in situ in uncomplicated cases. The DJ stents were removed after three weeks. The patients were followed up at three weeks for DJ stent removal if DJ stent was placed and then at six weeks with X-ray KUB.
All data were entered into a proforma created specifically for the study. Microsoft excel 2013 was used to store the information gathered. The data from 104 patients were examined, coded, and entered into IBM SPSS 24 for statistical analysis. The Chi-square test was used, as well as one-way analysis of variance (ANOVA) as a significance test for outcome analysis. A p-value of less than 0.05 was considered statistically significant.
4. Results
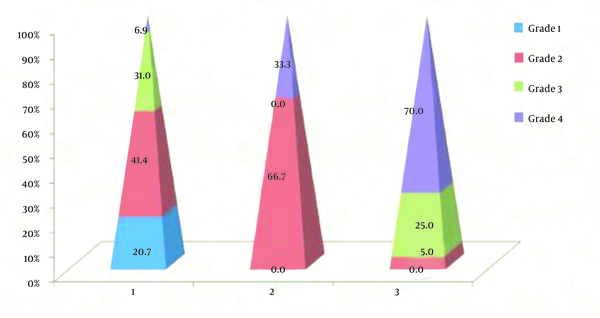
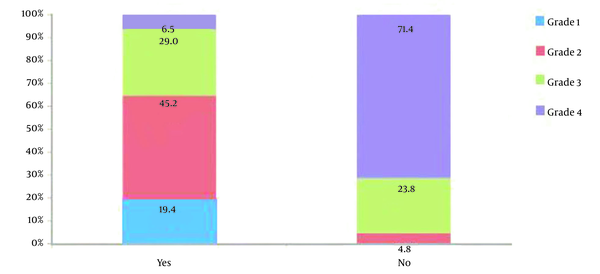
A total of 104 patients who underwent PCNL via upper calyceal access were analyzed. All relevant parameters of the study are summarized in Table 1. Totally, 12 patients were in GSS grade 1, 30 in GSS grade 2, 28 in grade 3, and 34 in grade 4. The mean age of patients was 41.6 ± 12.0. Males were highly predominant, with a share of 69.2%. The mean BMI was 24.29 ± 3.9 Kg/m2. Most of the obese and overweight patients were in GSS grades 3 and 4. Moreover, 25% of the patients had DM, and 30.8% with hypertension. Comorbidity were mainly in GSS grades 3 and 4. The mean ± SD of stone size was 25.1 ± 8.66 (15 - 45) mm. The mean stone size significantly increased with an increase in GSS grade. The mean ± SD of duration of completion of surgery was 80.73 ± 28.559 (40 - 135) minutes. Also, 38.4% of the patients had clinically significant residual fragments (CSRF), and 11.5% had clinically insignificant residual fragments (CIRF). Among the patients with CSRFs, 75.0% had grade 4, and 20.0% had grade 3 GSS, whereas among CIRFs, 66.7% had grade 3 and 33.3% had grade 4 of GSS. Moreover, 23% of patients underwent REDO-PCNL, while 13.5% of the patients underwent ESWL. There were 58 patients in CD grade 1, 40 patients in CD grade 3, and six in CD grade 2. Among the patients with CD grade 1 complications, 6.9% had grade 4 GSS, whereas, with CD grades 2 and 3, there were 33.0% and 70.0% grade 4 GSS (Figure 1). Six patients underwent intercostal tube drainage for pulmonary complications. In addition, 2.49 ± 1.08 percent was different in pre-and post-surgery mean hemoglobin (Hb). In the preoperative and postoperative difference of mean serum creatinine was 0.05 ± 0.14. Mean ± SD duration of hospital stay was 6.69 ± 6.4 days. Mean duration of hospital stay increased with higher grade of GSS. Sixty-two patients had immediate success among them, 29.0% had grade 3, and 6.5% had grade 4 GSS (Figure 2). Ten patients readmitted for urosepsis, six for sepsis and fever.
Parameters According to Guys Stone Score (N = 104)
| Guy’s Stone Score 1 (N = 12) | Guy’s Stone Score 2 (N = 30) | Guy’s Stone Score 3 (N = 28) | Guy’s Stone Score 4 (N = 34) | P-Value | |
|---|---|---|---|---|---|
| Age (mean), y | 36.7 | 38.6 | 45.9 | 42.3 | 0.51 |
| Gender (M: F) | 6:6 | 22:8 | 18:10 | 26:8 | 0.324 |
| Comorbidity | 2 | 14 | 16 | 20 | 0.00 |
| Overweight | 6 | 6 | 12 | 18 | 0.128 |
| DM | 2 | 6 | 8 | 8 | 0.12 |
| Hypertension | 0 | 4 | 12 | 12 | 0.12 |
| Previous renal surgery | 0 | 4 | 4 | 18 | 0.00 |
| Laterality (Rt: Lt) | 4:8 | 8:22 | 18:10 | 16:18 | 0.029 |
| Mean stone size (largest diameter in mm) | 18.67 | 17.4 | 23.07 | 35.82 | 0.00 |
| Puncture (supracostal/sub/supra + sub) | 6/6/0 | 16/14/0 | 28/0/0 | 14/20 | 0.00 |
| No. of track (1/> 1) | 12/0 | 30/0 | 28/0 | 14/20 | 0.00 |
| PCNL type (Classical/Tubeless/Total tubeless) | 0/4/8 | 0/20/10 | 28/0/0 | 34/0/0 | 0.00 |
| Residual fragments (CSRF/CIRF) | 0/0 | 2/0 | 8/8 | 30/4 | 0.00 |
| Ancillary procedure (PCNL/ESWL) | 0 | 2(0/2) | 10(4/6) | 30(20/10) | 0.00 |
| Complications Clavien-dindo grade (1/2/3) | 12/0/0 | 24/4/2 | 18/0/10 | 4/2/28 | 0.00 |
| UTI, Sepsis | 0 | 4 | 6 | 16 | 0.00 |
| Hematuria | 0 | 2 | 8 | 18 | 0.00 |
| Hemothorax | 0 | 0 | 0 | 6 | 0.00 |
| Colonic injury | 0 | 0 | 0 | 2 | 0.00 |
| Mean Hb change | 0.73 | 0.64 | 1.18 | 2.49 | 0.00 |
| Mean serum creatinine change | 0.05 | 0.03 | 0.05 | 0.07 | 0.63 |
| Mean hospital stay (day) | 2.67 | 3.47 | 4.79 | 12.53 | 0.00 |
| Immediate success (%) | 100 | 93 | 64.3 | 11.8 | 0.00 |
| Readmission | 0 | 0 | 4 | 14 | 0.01 |
Clavien-dindo grade complications
Immediate success rate
5. Discussion
Renal stone diseases are one of the major problems of patients presented to urology clinics, which affect about 12% of the world population at some stages in their lifetime (11). The PCNL varies in its complexity, and several preoperative nomograms have been used for the prediction of success rates and correlation with the complication rates with technical difficulty at present era. Thomas et al. (7) developed Guy's score using intravenous pyelogram findings to classify the patients. In the study by Singh et al. (12), the success rate for the management of complicated renal calculi was shown to be higher in the upper calyceal puncture group than in the lower calyceal puncture group. In the present study, patients had a mean age of 41.6 ± 12.0, which is comparable to the study by Kumar et al. (13), where the mean age of the patients was 40.8 ± 8.72 years. Thomas et al. (7) observed that the mean age was 51.7± 16.4 and in Khalil et al.’s study was 47.38 ± 14.6 years (14). Slightly lower mean age in the present study than aforementioned studies may be due to larger number of patients of younger age group presented in the hospital who are usually earning members of the family.
In Lojanapiwat et al.’s study (4), the number of previous open renal surgery did not affect outcome significantly (P = 0.79); however, Hu et al. (15) found that there were higher dip in hemoglobin, more need for renal angiographic embolization and secondary management, more operative duration and less early calculus free rate in patients who had a previous history of an open renal surgery. After surgery, there is retroperitoneal peri-renal scar, which may also involve in collecting system, thereby causing pelvicalyceal distortion and infundibular stenosis. This altered anatomy may affect stone formation and grade of GSS.
Although most intrarenal collecting systems can be accessed by superior calyceal puncture, it has a greater risk of pulmonary complications (16). Yan et al. (16) observed that supra-costal puncture was not associated with increased intrathoracic complication or morbidity if done by an experienced surgeon.
After the introduction of ESWL and the development of endourological interventions, residual calculi which, were small in diameter can be manageable, but insignificance of CIRF is questionable because small stones may become significant and result in infection and pain. In a study by Ganpule and Desai (17) residual fragments were identified in 7.57% of the patients.
In the study by de Souza Melo et al. (18) total complication rate was
14.3%, and most common complication was bleeding with transfusion rate of 4.8%. Hematuria during PCNL depends on stone size, location, number of access tracts, attempts with multiple punctures, supra-pole puncture, lesser trained surgeon, single kidney, and staghorn stone. Occasionally neighboring organs like gut, vessels, liver, and spleen can be injured. Pneumothorax can be developed due to close proximity of superior renal pole with thorax. This may require chest tube placement temporarily to drain air and fluid in case of pneumothorax or hemothorax.
In many studies, GSS one had minimum complications (18.9%), whereas GSS 4 had the highest (61.5%), but it is in discussion forum to establish a positive correlation of complications with GSS grade. It was observed by Jiang et al. (19) that one scoring system was Guy stone score to predict complications after PCNL.
In the present study, the definition of success in PCNL is the lack of any residual stone fragments on X-ray or/and computed tomography (CT) or observation of residual fragments (CIRF) that are not clinically significant on day one after operation and no intervention was required. Moreover, 29.0% of success cases had grade 3, and 6.5% had grade 4 of GSS. Higher proportion of immediate success was found among lower grade of GSS (P = 0.000). In the study by Lojanapiwat et al. (4), 87.50% success rate was observed in GSS1,71.43% success rate was observed in GSS2, 53.62% success was observed in GSS3, and 38.46% success rate was observed in GSS4 (P < 0.01). In the study by Kumar et al. (13), the success rate correlated with Guy's stone score (P < 0.0001). In the study by de Souza Melo et al. (18), it was found that success rate was inverse to the stone complexity graded with GSS. Mandal et al. (8) found the SFR for grade I, II, III, and IV were 81%, 72%, 35%, and 29%, respectively.
Readmission is hospitalization within 30 days of a discharge from the same or different hospital with the same well-being issue. In PCNL, uncontrolled pain, infection/sepsis, hematuria, urinary retention, and DJ stent displacement are usual causes of readmission. Readmission after PCNL were more associated with higher level of GSS (P = 0.001). Keskin et al. (20) found that total readmission of 27.1% in which hematuria was seen in 2.2%, sepsis 9.6%, and DJ stent replacement in 3.9%. Free bed in government hospital is also one reason for frequent readmission.
The “Guy’s Stone Score” is a useful technique for categorizing the complexity of PCNL. It is based on plain x-ray KUB, and x-ray intravenous urography is cheap, which is a useful investigation in low-income countries. It also has lower radiation hazards than computerized tomogram scan. This study confirmed that intravenous urography-based Guy’s Stone Score (GSS) is an easy tool to predict the early success rate and potential difficulties and complications in PCNL performed through superior calyceal puncture.
This study has some limitations as follows: it is a single institute-based observational study, small sample, only upper pole access PCNL, more than one surgeon operated the patients, no recruitment of kidney anomalies. No comparison was made with other nephrolithometry scores because they were based on computerized tomogram scans. Further study is required to overcome these limitations.
5.1. Conclusions
This study shows that intravenous pyelogram-based Guy’s Stone Score (GSS) is a reliable, easy to use technique to predict early success rate and potential post- PCNL complications performed via upper pole access.
References
-
1.
Pearle MS, Antonelli JA, Lotan Y. Urinary lithiasis and endourology. Etiology, Epidemiology, and Pathogenesis: Campbell-Walsh Urology. 11th ed. Elsevier; 2015. 1170 p.
-
2.
Chung DY, Kang DH, Cho KS, Jeong WS, Jung HD, Kwon JK, et al. Comparison of stone-free rates following shock wave lithotripsy, percutaneous nephrolithotomy, and retrograde intrarenal surgery for treatment of renal stones: A systematic review and network meta-analysis. PLoS One. 2019;14(2). e0211316. [PubMed ID: 30789937]. [PubMed Central ID: PMC6383992]. https://doi.org/10.1371/journal.pone.0211316.
-
3.
Kim BS. Recent advancement or less invasive treatment of percutaneous nephrolithotomy. Korean J Urol. 2015;56(9):614-23. [PubMed ID: 26366273]. [PubMed Central ID: PMC4565895]. https://doi.org/10.4111/kju.2015.56.9.614.
-
4.
Lojanapiwat B, Rod-Ong P, Kitirattrakarn P, Chongruksut W. Guy's Stone Score (GSS) Based on Intravenous Pyelogram (IVP) Findings Predicting Upper Pole Access Percutaneous Nephrolithotomy (PCNL) Outcomes. Adv Urol. 2016;2016:5157930. [PubMed ID: 28003822]. [PubMed Central ID: PMC5143681]. https://doi.org/10.1155/2016/5157930.
-
5.
Ozdedeli K, Cek M. Residual fragments after percutaneous nephrolithotomy. Balkan Med J. 2012;29(3):230-5. [PubMed ID: 25207006]. [PubMed Central ID: PMC4115827]. https://doi.org/10.5152/balkanmedj.2012.082.
-
6.
Lojanapiwat B, Prasopsuk S. Upper-pole access for percutaneous nephrolithotomy: comparison of supracostal and infracostal approaches. J Endourol. 2006;20(7):491-4. [PubMed ID: 16859462]. https://doi.org/10.1089/end.2006.20.491.
-
7.
Thomas K, Smith NC, Hegarty N, Glass JM. The Guy's stone score--grading the complexity of percutaneous nephrolithotomy procedures. Urology. 2011;78(2):277-81. [PubMed ID: 21333334]. https://doi.org/10.1016/j.urology.2010.12.026.
-
8.
Mandal S, Goel A, Kathpalia R, Sankhwar S, Singh V, Sinha RJ, et al. Prospective evaluation of complications using the modified Clavien grading system, and of success rates of percutaneous nephrolithotomy using Guy's Stone Score: A single-center experience. Indian J Urol. 2012;28(4):392-8. [PubMed ID: 23450640]. [PubMed Central ID: PMC3579117]. https://doi.org/10.4103/0970-1591.105749.
-
9.
Noureldin YA, Elkoushy MA, Andonian S. Which is better? Guy's versus S.T.O.N.E. nephrolithometry scoring systems in predicting stone-free status post-percutaneous nephrolithotomy. World J Urol. 2015;33(11):1821-5. [PubMed ID: 25678344]. https://doi.org/10.1007/s00345-015-1508-5.
-
10.
Okhunov Z, Helmy M, Perez-Lansac A, Menhadji A, Bucur P, Kolla SB, et al. Interobserver reliability and reproducibility of s.T.o.N.e. Nephrolithometry for renal calculi. J Endourol. 2013;27(10):1303-6. [PubMed ID: 23815088]. https://doi.org/10.1089/end.2013.0289.
-
11.
Alelign T, Petros B. Kidney Stone Disease: An Update on Current Concepts. Adv Urol. 2018;2018:3068365. [PubMed ID: 29515627]. [PubMed Central ID: PMC5817324]. https://doi.org/10.1155/2018/3068365.
-
12.
Singh R, Kankalia SP, Sabale V, Satav V, Mane D, Mulay A, et al. Comparative evaluation of upper versus lower calyceal approach in percutaneous nephrolithotomy for managing complex renal calculi. Urol Ann. 2015;7(1):31-5. [PubMed ID: 25657540]. [PubMed Central ID: PMC4310113]. https://doi.org/10.4103/0974-7796.148591.
-
13.
Kumar U, Tomar V, Yadav SS, Priyadarshi S, Vyas N, Agarwal N, et al. STONE score versus Guy's Stone Score - prospective comparative evaluation for success rate and complications in percutaneous nephrolithotomy. Urol Ann. 2018;10(1):76-81. [PubMed ID: 29416280]. [PubMed Central ID: PMC5791463]. https://doi.org/10.4103/UA.UA_119_17.
-
14.
Khalil M, Sherif H, Mohey A, Omar R. Utility of the Guy’s Stone Score in predicting different aspects of percutaneous nephrolithotomy. Afr J Urol. 2018;24(3):191-6. https://doi.org/10.1016/j.afju.2018.06.005.
-
15.
Hu H, Lu Y, Cui L, Zhang J, Zhao Z, Qin B, et al. Impact of previous open renal surgery on the outcomes of subsequent percutaneous nephrolithotomy: a meta-analysis. BMJ Open. 2016;6(4). e010627. [PubMed ID: 27126976]. [PubMed Central ID: PMC4854000]. https://doi.org/10.1136/bmjopen-2015-010627.
-
16.
Yan MY, Lin J, Chiang HC, Chen YL, Chen PH. Supra-costal tubeless percutaneous nephrolithotomy is not associated with increased complication rate: a prospective study of safety and efficacy of supra-costal versus sub-costal access. BMC Urol. 2018;18(1):112. [PubMed ID: 30537966]. [PubMed Central ID: PMC6290519]. https://doi.org/10.1186/s12894-018-0429-1.
-
17.
Ganpule A, Desai M. Fate of residual stones after percutaneous nephrolithotomy: a critical analysis. J Endourol. 2009;23(3):399-403. [PubMed ID: 19250022]. https://doi.org/10.1089/end.2008.0217.
-
18.
de Souza Melo PA, Vicentini FC, Beraldi AA, Hisano M, Murta CB, de Almeida Claro JF. Outcomes of more than 1 000 percutaneous nephrolithotomies and validation of Guy's stone score. BJU Int. 2018;121(4):640-6. [PubMed ID: 29322602]. https://doi.org/10.1111/bju.14129.
-
19.
Jiang K, Sun F, Zhu J, Luo G, Zhang P, Ban Y, et al. Evaluation of three stone-scoring systems for predicting SFR and complications after percutaneous nephrolithotomy: a systematic review and meta-analysis. BMC Urol. 2019;19(1):57. [PubMed ID: 31262284]. [PubMed Central ID: PMC6604199]. https://doi.org/10.1186/s12894-019-0488-y.
-
20.
Keskin SK, Danacioglu YO, Turan T, Atis RG, Canakci C, Caskurlu T, et al. Reasons for early readmission after percutaneous nephrolithotomy and retrograde intrarenal surgery. Wideochir Inne Tech Maloinwazyjne. 2019;14(2):271-7. [PubMed ID: 31118994]. [PubMed Central ID: PMC6528118]. https://doi.org/10.5114/wiitm.2018.77705.