Abstract
Background:
Dihydropyrimidine dehydrogenase (DPD) is the initial enzyme in the catabolism of 5-fluorouracil (5-fu). Deficiency of this enzyme can lead to severe and lethal toxicity following the administration of 5FU or capecitabine. The aim of this study was to demonstrate the prevalence of the IVS14 + 1G > A mutation of the dihydropyrimidine dehydrogenase gene (DPYD) and important side effects of the adjuvant chemotherapy regimens in an ethnic Iranian group of colorectal cancer (CRC) patients.Methods:
The research population included patients with colorectal cancer during the period of October 2011 to January 2013. Genomic DNA was isolated from blood cells of 109 patients. Polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP) technique was carried out to identify the frequency of the IVS14 + 1G > A mutation. The side effects of chemotherapy regimens containing 5-FU or capecitabine were recorded during 1-6 courses of chemotherapy.Results:
The IVS14 + 1G > A mutation was not found in the population studied. Overall 28.4% of patients reported to have at least 1 grade 3 or 4 toxicity.Conclusions:
We concluded that IVS14 + 1G > A mutation was rare in the population studied; however, a larger sample size may be required to determine the precise mutation frequency in this region.Keywords
Colorectal Cancer Dihydropyrimidine Dehydrogenase 5-fu Toxicity Iran
1. Background
Colorectal cancer (CRC) is the 3rd most common prevalent cancer and a significant cause of cancer-dependent mortalities worldwide (1). It is believed that Iran is a known zone of gastrointestinal cancer with a high incidence of especially colorectal cancers and it has been reported to be among the 5 most common cancers in Iran (2).
5- Fluorouracil (5-FU) has been used as a chemotherapy agent for about 50 years (1, 3). The cytotoxic effects of 5-FU are known to be caused by its metabolites. Thymedylate synthase inhibition by 5-fluoro-deoxy-uridine monophosphate, ametabolite of 5-FU can lead to impaired DNA synthesis. In addition, 5-FU metabolites intervene with nucleoside metabolism, which can also be interpolated into RNA and DNA, and ultimately help to cytotoxicity 5-FU and cell death. An oral pro-drug of 5-fluorourarcil is capecitabine, which is converted to the active drug 5-FU in the tumor and also normal tissues by a 3step enzymatic activation process. Indeed, capecitabine becomes active after the conversion to 5-FU (4). 5-FU is catabolized to 2-fluoro-β-alanine by 3 enzymes. The first and rate-limiting enzyme in the process is dihydropyrimidine dehydrogenase (DPD) (4). DPD has activity been widely detected in various organs. However, up to 80% of administered 5-FU is catabolized by DPD in hepatic cells or peripheral blood mononuclear cells (5, 6). Accordingly, DPD activity is very important in predicting the toxicity and efficacy of flourouracils. Life-threatening toxicity secondary to treatment with 5-FU is seen in DPD-deficient cancer patients. It has been shown that cancer patients with even a 50% of the normal level of DPD activity suffer from severe toxicity following treatment of flourouracils (6-9).
So far 39 different mutations have been identified in the DPD gene, some of them resulting in decreased DPD activity. One of these polymorphisms in the DPD gene, resulting in decreased enzyme activity, is a splice-site IVS14 + 1G/A mutation, which is the result of a G to A transition in the GT5’-splice recognition site of intron14 (7-9). Random screening for the IVS14 + 1G > A DPD variant in different normal populations has shown that frequencies of homozygotes and heterozygotes alleles are approximately between 0 to 1.2% (7, 9).
The purpose of this research was to find the prevalence rate of the IVS14 + 1G > A mutation of DPD gene in a group of Iranian CRC patients and to investigate the prevalence of severe toxicities of adjuvant chemotherapy maybe relevant to this mutation.
2. Methods
This prospective study was approved by the ethics committee of Mashhad University of Medical Sciences (MUMS). A written informed consent from each patient was also obtained. The research population included patients with colorectal cancer consecutively that referred to the department of oncology of Omid and Imam Reza hospitals, MUMS during the period of October 2011 to January 2013.
The laboratory routine tests included: CBC (diff), liver function test, kidney function test, alkaline phosphatase, and lactate dehydrogenase, which were done for patients during their first visit.
Patients older than 75 years and also those patients who were considered inappropriate for chemotherapy as a result of a poor performance status score (Karnofsky scale) of fewer than 60 or functional disorder of kidney or liver were excluded from the study. Patients who were eligible for chemotherapy with different chemotherapy regimens containing 5-FU or capecitabine were included in the study. The side effects related more to the administration of these drugs were recorded through a period of at least 1 to maximum of 6 courses. Patients were visited weekly, biweekly, or whenever a complaint presented by patients. CBC and routine examinations were done at the same interval. The side effects were recorded based on the WHO common toxicity criteria (10). Genomic DNA was extracted from blood cells (1000 µL of whole blood) by using a standard DNA isolation Kit (Biogene, Mashhad, Iran). DNA obtained was quantified by measuring absorption of 260 / 280 nm (Nanodrop ND-1000, USA). PCR-RFLP technique was performed on the isolated DNA by amplification of the region expected to contain the IVS14 + 1G > A mutation of exon 14 of DPD. The following primer pair was used for PCR reactions: 5’-ATCAGGACATTGTGACATATGTTTC-3’ as a sense primer and 5’ -CTTGTTTTAGATGTTAAATCACACATA-3’ as an anti-sense primer. PCR was carried out in a volume of 20 µL containing 40 ng of the template DNA, MgCl2 (50 mM), PCR buffer 10× (2 µL), dNTPs (200 µM), Taq DNA polymerase (0.5 IU, Genet Bio, Korea), and 4pMof each primer. The PCR was performed in gradient thermal cycler (Astec, Japan) consisting: initial strand separation (5 minutes) at 94°C, 36 cycles of initial denaturation 20 seconds at 94°C, 40 seconds at 56°C for annealing , 40 seconds at 72°C for extension, and then 8 minutes at 72°C for final extension. The reaction product (5 µL) was visualized with electrophoresis in 1.5% agarose gel with ethidium bromide staining.
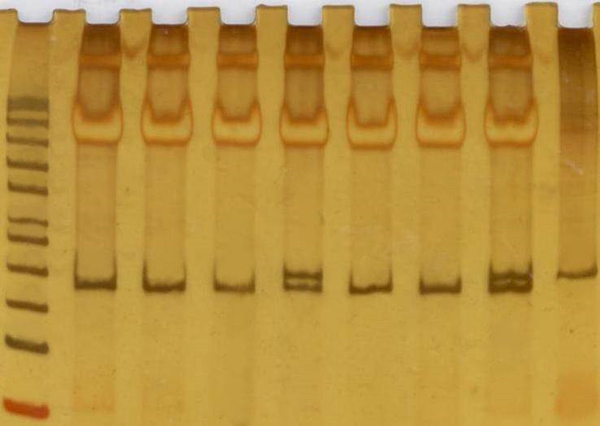
For the RFLP assay, 7 µL of PCR product was digested with 3U of NdeI restriction endonuclease (Thermoscientific, Canada) overnight at 37°C. The digested fragments were separated by electrophoresis on 3% (W/V) agarose gel for 2 hours at 120 V. The wild-type allele (IVS14 + 1G) was expected to yield 2 bands of 181 and 17 bp fragments, while the mutant allele (IVS14 + 1A) was expected to produce 3 fragments of 154 bp, 27 bp, and 17 bp after a digestions with NdeI (Figure 1). Some specimens were reassessed randomly in a referral hospital lab to ensure the accuracy of the tests.
PCR-RFLP Production
3. Results
A group of 109 patients who met our inclusion criteria were included in the study. Table 1 shows the demographic characteristics of patients that participated in the study. After prescription of 468 cycles of chemotherapy and recording the side effects occurring during the 1st 6 cycles of chemotherapy for every patient, a total of 55 episodes of grade 3 and 4 side effects were recorded as 11.6% of all cycles. Overall 31 patients (28.4%) have been confronted with at least 1 important side effect during chemotherapy at a time. The most common grade 3 and 4 side effects were neutropenia in 20.2% and after that nausea (7.3%) and diarrhea (6.4%). One patient died with signs and symptoms of neutropenic fever and grade 3 diarrhea (Table 2).
Patients’ Characteristics
| Variables | Value |
|---|---|
| Patients | 109 |
| Age, y | |
| Range | 23 - 75 |
| Median | 56 |
| Gender | |
| Male | 64 |
| Female | 45 |
| Anatomical tumor site | |
| Colon | 56 |
| Rectum | 53 |
| Stage | |
| II | 13 |
| III | 31 |
| IV | 35 |
| Undetermined | 30 |
| Performance status (Karnofsky scale) | |
| 90 | 82 |
| 80 | 19 |
| 70 | 4 |
| 60 | 4 |
| Toxicities | Frequency |
|---|---|
| Anemia | 2 (0.4) |
| Leukopenia | 8 (1.7) |
| Neutropenia | 25 (5.3) |
| Thrombocytopenia | 2 (0.4) |
| Hand and foot syndrome | 1 (0.2) |
| Nail changes | 1 (0.2) |
| Diarrhea | 6 (1.3) |
| Emesis | 7 (1.5) |
| Vomiting | 1 (0.2) |
| Stomatitis | 3 (0.6) |
| Total | 55 (11.6) |
No individuals as the heterozygote or homozygote for IVS14 + 1G > A DPYD mutation was found among all cases of CRC patients in this study.
4. Discussion
To the best of our knowledge, this is the first study on DPD mutation from the Iranian population. However the prevalence of the IVS14 + 1G > A mutation has been reported from different countries before. In one of the largest studies thus far, it was found that the frequency of this mutation was 0.94% among the German population. There were 2 IVS14 + 1G > A mutation heterozygotes in 228 colorectal tumor patients (0.88%). Also 5 heterozygotes and 1 hemozygote of IVS14 + 1G > A mutation were found among 25 patients with severe 5-FU related toxicity (11). A study in France reported only 2 IVS14 + 1G > A mutation heterozygotes among 93 patients experiencing severe 5-FU related toxicity (12). At a large screening study among the white healthy population in Deutschland, the prevalence of this mutation reported to be 1.8% (13).
In another Dutch study, the researchers reported a very close relation between grade 4 neutropenia and DPD IVS14 + 1G > A mutation. As much as 50% of the patients registered in this study had the mutation (14). In a study from Turkey among 250 healthy volunteers, no mutation was identified in the DPD allele (9). Another study from Turkey, however, among the cancer patients population, 3 out of 200 patients were found to represent the heterozygote IVS14 + 1G > A mutation for DPD (15). In a cohort study from Poland, including 252 CRC patients, 1 heterozygote for this mutation was identified (0.44%). This was 1 of 4 CRC patients suffering from severe myelotoxicity (7).
From Egypt, a study comprised of 247 healthy individuals reported no referred DPD IVS14 + 1G > A mutation (16). In an analysis of DPD mutations, among 300 Taiwanese healthy subjects the researchers found no mutation of IVS14 + 1G > A. In addition, there was no association between any of other mutations with DPD protein levels (17). In other studies no IVS14 + 1G > A mutation was detected among Japanese, Korean, and African-Americans as well (8, 18, 19). It seems that the mutation frequency is less reported in Asian and African ancestries. Based on some estimations, 1% - 3% of the normal Caucasian population could be heterozygotes for the mutant DPD alleles (6, 11).
4.1. Conclusion
We could not find any DPD IVS14 + 1G > A mutation in our study. We are aware that-our sample size was not large enough to estimate the real frequency of this mutation among our population, therefore, the study will continue to find at least 1 mutation. Although, the sever grade 3 and 4 complications, after receiving 5-FU and capeciatbine based chemotherapy, was not infrequent, however, among these patients, we could not find a mutation as well. It is possible that a different mutation other than DPD IVS14 + 1G > A mutation was responsible for the observed toxicity or maybe the toxicities were due to other unknown mechanisms in our population. These alternative possibilities could be subject of larger and more comprehensive studies.
4.2. Clinical Practice Points
IVS14 + 1G/A mutation is a known cause of chemotherapy related toxicities of CRC patients. There have been some reports about the prevalence rate of this mutation from different countries before. According to this study, frequency of this mutation was between 0% - 1.8%.
This article was the only study on CRC patients in Iran that couldn’t find any mutations, therefore, we estimate that the prevalence of this mutation shouldn’t be more than 1% in this population.
We’ll continue this study on more patients. If we would make sure of aforementioned prevalence of DPD mutation in the studied population, we won’t need to perform screening test for DPD deficiency before prescription of 5-fu or capecitabine to our patients.
Acknowledgements
References
-
1.
Jemal A, Center MM, DeSantis C, Ward EM. Global patterns of cancer incidence and mortality rates and trends. Cancer Epidemiol Biomarkers Prev. 2010;19(8):1893-907. [PubMed ID: 20647400]. https://doi.org/10.1158/1055-9965.EPI-10-0437.
-
2.
Islamic Republic of Iran. Ministry of health and medical education: Iranian annual of national cancer registration report. 2004.
-
3.
Potter JD. Colorectal cancer: molecules and populations. J Natl Cancer Inst. 1999;91(11):916-32. [PubMed ID: 10359544]. https://doi.org/10.1093/jnci/91.11.916.
-
4.
Koopman M, Venderbosch S, Nagtegaal ID, van Krieken JH, Punt CJ. A review on the use of molecular markers of cytotoxic therapy for colorectal cancer, what have we learned? Eur J Cancer. 2009;45(11):1935-49. [PubMed ID: 19473832]. https://doi.org/10.1016/j.ejca.2009.04.023.
-
5.
Lu Z, Zhang R, Carpenter JT, Diasio RB. Decreased dihydropyrimidine dehydrogenase activity in a population of patients with breast cancer: implication for 5-fluorouracil-based chemotherapy. Clin Cancer Res. 1998;4(2):325-9. [PubMed ID: 9516918].
-
6.
Wei X, McLeod HL, McMurrough J, Gonzalez FJ, Fernandez-Salguero P. Molecular basis of the human dihydropyrimidine dehydrogenase deficiency and 5-fluorouracil toxicity. J Clin Invest. 1996;98(3):610-5. [PubMed ID: 8698850]. https://doi.org/10.1172/JCI118830.
-
7.
Sulzyc-Bielicka V, Binczak-Kuleta A, Pioch W, Kladny J, Gziut K, Bielicki D, et al. 5-Fluorouracil toxicity-attributable IVS14 + 1G > A mutation of the dihydropyrimidine dehydrogenase gene in Polish colorectal cancer patients. Pharmacol Rep. 2008;60(2):238-42. [PubMed ID: 18443386].
-
8.
Tanaka D, Hishida A, Matsuo K, Iwata H, Shinoda M, Yamamura Y, et al. Polymorphism of dihydropyrimidine dehydrogenase (DPYD) Cys29Arg and risk of six malignancies in Japanese. Nagoya J Med Sci. 2005;67(3-4):117-24. [PubMed ID: 17375478].
-
9.
Suzen HS, Yuce N, Guvenc G, Duydu Y, Erke T. TYMS and DPYD polymorphisms in a Turkish population. Eur J Clin Pharmacol. 2005;61(12):881-5. [PubMed ID: 16328315]. https://doi.org/10.1007/s00228-005-0054-2.
-
10.
Trotti A, Byhardt R, Stetz J, Gwede C, Corn B, Fu K, et al. Common toxicity criteria: version 2.0. an improved reference for grading the acute effects of cancer treatment: impact on radiotherapy. Int J Radiat Oncol Biol Phys. 2000;47(1):13-47. [PubMed ID: 10758303]. https://doi.org/10.1016/S0360-3016(99)00559-3.
-
11.
Raida M, Schwabe W, Hausler P, Van Kuilenburg AB, Van Gennip AH, Behnke D, et al. Prevalence of a common point mutation in the dihydropyrimidine dehydrogenase (DPD) gene within the 5'-splice donor site of intron 14 in patients with severe 5-fluorouracil (5-FU)- related toxicity compared with controls. Clin Cancer Res. 2001;7(9):2832-9. [PubMed ID: 11555601].
-
12.
Magné N, Renée N, Formento JL, Etienne-Grimaldi MC, Francoual M, Milano G. Prospective study of dihydropyrimidine dehydrogenase (DPD) activity and DPYD IVS14+1G>A mutation in patients developing FU-related toxicities: An updated analysis based on a ten-year recruitment across multiple French institutions. J Clin Oncol. 2005;23(16_suppl):2003. https://doi.org/10.1200/jco.2005.23.16_suppl.2003.
-
13.
van Kuilenburg AB, Muller EW, Haasjes J, Meinsma R, Zoetekouw L, Waterham HR, et al. Lethal outcome of a patient with a complete dihydropyrimidine dehydrogenase (DPD) deficiency after administration of 5-fluorouracil: frequency of the common IVS14+1G>A mutation causing DPD deficiency. Clin Cancer Res. 2001;7(5):1149-53. [PubMed ID: 11350878].
-
14.
Van Kuilenburg AB, Meinsma R, Zoetekouw L, Van Gennip AH. Increased risk of grade IV neutropenia after administration of 5-fluorouracil due to a dihydropyrimidine dehydrogenase deficiency: high prevalence of the IVS14+1g>a mutation. Int J Cancer. 2002;101(3):253-8. [PubMed ID: 12209976]. https://doi.org/10.1002/ijc.10599.
-
15.
Celik I, Kars A, Guc D, Tekuzman G, Ruacan S. Dihydropyrimidine dehydrogenase enzyme deficiency: clinical and genetic assessment of prevalence in Turkish cancer patients. Cancer Invest. 2002;20(3):333-9. [PubMed ID: 12025228]. https://doi.org/10.1081/CNV-120001178.
-
16.
Hamdy SI, Hiratsuka M, Narahara K, El-Enany M, Moursi N, Ahmed MS, et al. Allele and genotype frequencies of polymorphic cytochromes P450 (CYP2C9, CYP2C19, CYP2E1) and dihydropyrimidine dehydrogenase (DPYD) in the Egyptian population. Br J Clin Pharmacol. 2002;53(6):596-603. [PubMed ID: 12047484].
-
17.
Hsiao HH, Yang MY, Chang JG, Liu YC, Liu TC, Chang CS, et al. Dihydropyrimidine dehydrogenase pharmacogenetics in the Taiwanese population. Cancer Chemother Pharmacol. 2004;53(5):445-51. [PubMed ID: 15132136]. https://doi.org/10.1007/s00280-003-0749-y.
-
18.
Cho HJ, Park YS, Kang WK, Kim JW, Lee SY. Thymidylate synthase (TYMS) and dihydropyrimidine dehydrogenase (DPYD) polymorphisms in the Korean population for prediction of 5-fluorouracil-associated toxicity. Ther Drug Monit. 2007;29(2):190-6. [PubMed ID: 17417073]. https://doi.org/10.1097/FTD.0b013e318040b1fe.
-
19.
Ahluwalia R, Freimuth R, McLeod HL, Marsh S. Use of pyrosequencing to detect clinically relevant polymorphisms in dihydropyrimidine dehydrogenase. Clin Chem. 2003;49(10):1661-4. [PubMed ID: 14500593]. https://doi.org/10.1373/49.10.1661.
