Abstract
Background:
Type I bipolar disorder is a chronic mental illness with a recurrent nature.Objectives:
This study was done to identify risk factors for relapse in patients with type I bipolar disorder using Poisson regression.Methods:
In this retrospective cohort study, data were collected from 331 bipolar type I patients admitted to the largest and the only psychiatric hospital in West of Iran, Kermanshah. Poisson regression was used to identify risk factors for the relapse numbers in STATA software.Results:
One hundred sixty six of 331 patients (50.2%) were men. Mean and standard deviation of relapse rates in males and females were 2.93 ± 0.16 and 2.93 ± 0.15, respectively. In multivariate analysis, the results showed that with increasing age of disease onset (RR = 0.98, 95% CI :(0.97 -0.99)) and adherence to medication (RR = 0.86, 95% CI :(0.75-0.98)), the relapse rate ratio decreased, and being divorced or widowed (RR = 1.20,95% CI :( 1.01-1.45)), cigarette smoking (RR = 1.28, 95% CI: (1.52-1.09)), and birth season of winter (RR = 1.18, 95% CI: (1.00-1.41)) increased the rate ratio of relapse.Conclusions:
The results of this study showed that the frequency of relapse was lower in bipolar patients younger at the time of disease onset, cigarette smokers, divorced or widowed patients, and patients with no treatment adherent. It is necessary to prevent or reduce the likelihood of relapse, especially in patients who do not have therapeutic adherence through educational and therapeutic measurements.Keywords
1. Background
Bipolar disorder is a mood disorder and a chronic, severe, and recurrent mental disease. The patients are suffering from severe changes in their mood. Despite the availability of effective drugs, this disorder is still one of the major causes of disability, mortality, and functional decline worldwide, which significantly reduces the quality of life of patients (1, 2). It usually appears at the end of adolescence or early adulthood (3). According to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders Text Revision (DSM-V), this disorder has several types, which the most important types include bipolar I disorder and bipolar II disorder. The difference between the two types is the presence of mania period; this period occurs in type I, but in type II, as a milder type, patients are symptomatic more than half of the time (4). Bipolar I and II disorders affect about 1-4% of the world's population, and the prevalence is almost the same between men and women (3, 5). In 1990, bipolar disorder was the sixth leading cause of disabilities caused by diseases (6).
This disorder has a negative impact on academic and occupational performance, interpersonal conflicts, and legal issues, especially in adolescent patients, with a high risk of suicide and other adverse outcomes (7-11). Severe symptoms of bipolar disorder can lead to hospital admission (12-14). Approximately 50–60% of patients experience an exacerbation of symptoms or hospitalization one year after an episode (15). Given the high relapse rate of patients with bipolar disorder (or another serious psychiatric disease), it is important from a clinical and public health point of view to evaluate the number of relapses in the hospital and to understand the factors affecting it. The number of occurrences of each event in a given period can be described as numerical data (16, 17). Counting regression models are used when the response variable is the counted number of occurrences, and the researcher seeks to understand how the response variable (e.g., relapse) increases with the explanatory variable. These types of data are usually analyzed using Poisson regression (18, 19).
2. Objectives
Since the data on the number of relapses is count data, the main objective of this study was to assess the effects of demographic factors, family, and environment on the relapse number of people with bipolar I disorder using the Poisson regression model.
3. Methods
3.1. The Population and Sample of the Study
The present study was a retrospective cohort study in which all patients with bipolar I disorder admitted to the Kermanshah Farabi teaching-treatment hospital from the beginning of 2015 until the end of 2019 were included in the study. Farabi Hospital is the largest and most specialized neuroscientific center in western Iran.
3.2. Data Collection
Inclusion criteria included bipolar disorder diagnosed by a psychiatrist, according to DSM 5, having at least one relapse leading to hospitalization, as well as the age of 18 to 65 years. Exclusion criteria included patients with comorbidity, a bipolar disorder due to substance abuse, a bipolar disorder due to medication use, and bipolar schizoaffective disorder. The patient's clinical psychological interview form was completed by psychiatrists for patients to collect data through the patient record sheet and recorded in pre-designed forms by the researcher. The investigators also contacted the patient's family in order to correct any inaccuracies in the file information, and the patient was excluded from the study if the co-workers did not answer the phone or did not respond appropriately. Finally, the specification of 331 bipolar I patients was collected out of 733 reviewed cases.
3.3. Variables of the Study
The studied variables included the number of re-hospitalizations (relapse) as the response variable, and age at the onset of disease, gender, marital status, place of residence, the season of birth, employment status, substance abuse, cigarette smoking, alcohol use, bipolar history in the family (grade 1 to 3), history of suicide attempt, and adherence to medication were considered as independent variables. In this study, medication adherence was measured self-reportedly because it was easier, cheaper, and feasible than other adherence measurement methods (20, 21). Having a bipolar patient family (grade one to three) was considered a family history. A history of head trauma is a trauma that caused a skull fracture or coma before the onset of the disease.
3.4. Statistical Analysis
Frequency and percentage were used to analyze qualitative variables and mean and standard deviation were used to analyze quantitative variables. Poisson regression is appropriate when the variance of the response variable is equal to its mean, while in reality, the variance often exceeds the mean in count data (18). The deviance statistics were used to check the validity of using Poisson regression (assumption of mean and variance equality). When the result of this statistic is closer to 1, the assumption of equity of mean and variance of the response variable is established, and the accuracy of using the Poisson regression model is valid (22). In this study, the mean number of relapses was 2.83, and their variance was 4.28, and the mean of deviance statistics was 1.17. Therefore, due to its proximity to number 1, the validity of using Poisson regression was confirmed. Selecting variables firstly was done in a univariate model, and then the variables were included in the multivariate analysis, which rated as P value < 0.05 in the univariate analysis. All analyses were done using Stata software version 14.1 (Stata Corp, College Station, TX, USA).
4. Results
Of the 331 bipolar patients, 166 (50.2%) were male. The total number of relapses for these patients was 915, of which 475 relapses were seen in men, and 440 were in women. The mean age of the patients in men and women was 41.25 ± 0.98 and 40.25 ± 0.96, respectively. The mean age at onset of the disease was 29.78 ± 97.9 in males and 29.32 ± 0.80 years in females. Also, 162 (48.9%) patients were married, 114 (34.4%) were single, and the rest were divorced or widowed, and 147 cases (44.4%) were employed. Only 15 (4.5%) of them had a college education, 66 (19.9%) reported substance abuse, and 90 (27.2%) noted cigarette smoking. The majority of patients (95 patients, 28.7%) were born in spring, 37 patients (11.2%) had a history of bipolar disorder in the family, and 76 (24.2%) patients had a history of a suicide attempt. Also, 181 patients (54.7%) had no medication adherence.
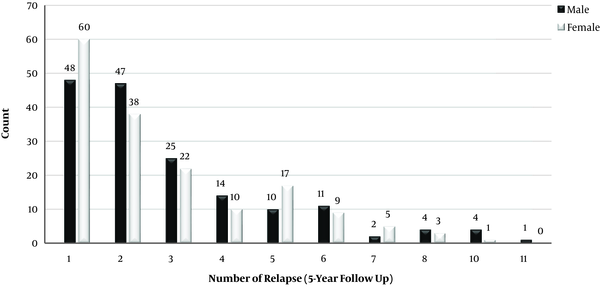
The distribution of relapses showed that 11 men and 9 women experienced more than 7 relapses. Overall, the mean of relapse rates in males and females was 2.93 ± 0.16 and 2.73 ± 0.15, respectively (Figure 1).
Distribution of the relapse numbers in patients with bipolar I disorder
In univariate analysis, the effects of variables of marital status, age at onset of bipolar, the season of birth, cigarette smoking, substance abuse, suicide history, and medication adherence on relapse rates in bipolar patients were significant, and after multivariate analysis, the effects of all variables except the variables of substance abuse and history of attempted suicide were significant (Table 1).
Results of Variables Description and Fitting of the Poisson Regression Model Using Anticipating Variables
| Variable | Frequency (%) | Crude RR (95% CI) | Adjust RR (95% CI) | P Value |
|---|---|---|---|---|
| Age at onset of bipolar, mean ± SE | 29.55 ± 0.63 | 0.96 (0.94 - 0.98) | 0.986 (0.980 - 0.993) | < 0.001 |
| Gender | ||||
| Male | 166 (50.2) | 1.00 | ||
| Female | 165 (49.8) | 0.98 (0.81 - 1.05) | ||
| Marital status | ||||
| Married | 162 (48.9) | 1.00 | ||
| Single | 114 (34.4) | 1.18 (1.03 - 1.37) | 1.07 (0.91 - 1.24) | 0.38 |
| Divorced or widow | 55 (16.6) | 1.23 (1.03 - 1.47) | 1.20 (1.00 - 1.45) | 0.045 |
| Place of residence | ||||
| Urban | 254 (76.7) | 1 | ||
| Rural | 77 (23.3) | 1.10 (0.94 - 1.27) | ||
| Employment status | ||||
| Employed | 147 (44.4) | 1.00 | ||
| Unemployed | 184 (55.6) | 1.05 (0.93 - 1.20) | ||
| Education | ||||
| Illiterate and primary | 164 (49.5) | 1.00 | ||
| High school and diploma | 152 (45.9) | 1.13 (0.99 - 1.29) | ||
| College | 15 (4.5) | 0.97 (0.70 - 1.35) | ||
| Substance abuse | ||||
| Non-addicts | 265 (80.1) | 1.00 | ||
| Addicts | 66 (19.9) | 1.20 (1.03 - 1.40) | ||
| Cigarette smoking | ||||
| Non-smokers | 241 (72.8) | 1.00 | 1.00 | |
| Smokers | 90 (27.2) | 1.29 (1.12 - 1.48) | 1.28 (1.09 - 1.52) | 0.002 |
| Alcohol use | ||||
| No | 310 (93.7) | 1.00 | ||
| Yes | 21 (6.3) | 1.01 (0.77 - 1.31) | ||
| History of prison | ||||
| No | 260 (78.5) | 1 | ||
| Yes | 23 (6.9) | 1.01 (0.78 - 1.30) | ||
| Season of birth | ||||
| Spring | 95 (28.7) | 1.00 | 1.00 | |
| Summer | 78 (23.6) | 1.10 (0.92 - 1.1.32) | 1.14 (0.95 - 1.37) | 0.15 |
| Autumn | 68 (20.5) | 1.03 (0.85 - 1.25) | 1.04 (0.86 - 1.26) | 0.65 |
| Winter | 90 (27.2) | 1.10 (0.92 - 1.32) | 1.18 (1.00 - 1.41) | 0.050 |
| History of head trauma | ||||
| No | 301 (90.9) | 1.00 | ||
| Yes | 30 (9.1) | 1.13 (0.91 - 1.40) | ||
| Family history of bipolar | ||||
| No | 294 (88.8) | 1.00 | ||
| Yes | 37 (11.2) | 1.03 (0.84 - 1.26) | ||
| Suicide attempts | ||||
| No | 251 (75.8) | 1.00 | ||
| Yes | 80 (24.2) | 1.24 (1.08 - 1.43) | ||
| Medication adherence | ||||
| Non-adherence | 181 (54.7) | 1.00 | 1.00 | |
| Adherence | 150 (45.3) | 0.81 (0.71 - 0.93) | 0.86 (0.75 - 0.98) | 0.032 |
As the age at onset of the bipolar increased, the rate ratio of disorder relapse approximately 0.01 decreased (RR = 0.98, 95% CI: (0.97-0.99). Being divorced or widowed increased the rate ratio of relapse by 20% (RR = 1.20, 95% CI: (1.01-1.45)). The rate ratio of the following relapses in patients who smoked was 1.28 times than those who did not smoke (RR = 1.28, 95% CI: (1.09-1.52). In other words, the risk of relapse showed an increase in patients who smoked 28% more than non-smokers. The effect of winter birth on relapse rate was significant (RR = 1.18, 95% CI: (1.00-1.41) so that rate ratio of relapse rates in patients born in winter was 18% higher than those born in spring; however, autumn and summer seasons had no significant effect on subsequent relapses. Also, the effect of medication adherence was significant on relapse rates (RR = 0.86, 95% CI: (75-0.98)) so that the rate ratio of relapse rates was 0.14% lower in patients with medication adherence than patients with no adherence. Overall, sex, occupation, place of residence, education, head trauma history, prison history, history of substance abuse, family bipolar history, and suicide history did not affect the rate of relapse in bipolar patients (Table 1).
5. Discussion
Bipolar I disorder is one of the most important and reversible psychiatric illnesses, and if these patients do not receive proper treatment and follow-up, this disorder will often relapse during their lives. Each attack has an adverse effect on the prognosis of the disease, in addition to causing unpleasant effects on the mental state of the patient and those in contact with him. The costs incurred by the sufferer directly and indirectly on the family and society during the acute period are also high (23). The aim of this study was to identify risk factors for relapse in patients with bipolar disorder using the Poisson regression model.
In this study, the frequency of relapse was higher in men than in women, but gender had no significant effect on relapse. In some studies, gender did not have a significant effect on relapse (24, 25), but in some studies (26) relapse occurred more frequently in men. Given that different variables have been studied, there may be some involving variables that are related to the gender effect in these studies; thus, further studies are needed.
In this study, the marital status variable had an effect on the increase of relapse, so that the widowed or divorced patients were more likely to have a relapse. However, in some studies (25, 27), marital status did not have a significant effect on the relapse of bipolar disorder. In their study, Ghoreishizadeh et al. (28) investigated risk factors for relapse of bipolar I disorder solely on the basis of the frequency of observed factors, but relapse in divorced or widowed individuals was more than married and single ones. Patient care is demanding due to the long treatment process and causes despair, erosion, incidence, or exacerbation of psychosomatic disorders in other family members, especially the patient's parents and spouse (29). The family and its supports play an important role in the treatment and prevention of relapses; thus, given the difficulty of caring for the mentally ill patients, loss of this supportive focus (divorce or death of a spouse) may increase the incidence of relapse in these patients.
The effect of age at onset of the bipolar was significant on the number of relapses so that patients who experienced their first relapse at a younger age were at a higher risk of recurrence than those who were older at the first relapse. However, this was only marginally 1%. In other studies (25, 30) similar results were obtained, and younger patients had more relapse rates. In some adolescents, an emotional crisis or other traumatic events may be the initial cause of the depressive or manic phase. It can also be inferred that because these patients have had a longer period of illness; therefore, they are tired of the disease and treatment process and are less likely to follow the treatment process, which will cause more relapses.
The results of this study showed that bipolar relapses are more common in spring and winter. Winter births caused more relapses than spring births, which was significant, summer and fall births were associated with fewer relapses than spring, but this effect was not significant. In some studies, however, the season of birth (31, 32) had no significant effect on the subsequent relapses in type I bipolar patients. Although genetic components play a major role in the onset of psychiatric and personality disorders, environmental factors may also have significant effects on their incidence of relapses (33). In a study examining personality dimensions (34) and the birth season, no significant effect was seen in none of the NEO Personality Inventory-Revised (NEO PI-R) dimensions, except for the agreeableness dimension. Winter births were associated with lower agreeableness. A review study of more than 250 studies found that bipolar and schizophrenic patients were more likely to be born in winter and spring (35). This hypothesis has been declared in patients with mental disorders, which says that a risk factor specific to these seasons, such as viruses or changes in diet, environment, and temperature variations may affect these disorders (34, 35). Therefore, further studies are needed to understand the effect of the birth season.
In the present study, the cigarette smoking rate among patients with bipolar I disorder was 27.2%. In a study by Ostacher et al. (36), the smoking rate in bipolar patients was reported to be 38.8%, and they found that smoking in these patients exacerbated the symptoms of bipolar disorder and they had poorer functioning. Nicotine increases concentration, decreases tension and feelings of depression, and bipolar disorder patients may increase their concentration with nicotine and treat their distraction as one of the main symptoms of bipolar disorder (37). Therefore, since cigarette metabolism and the metabolism of most mood-regulating and antidepressant drugs occur in the liver, cigarette smoking will decrease drug absorption levels and possibly lead to repeated relapses.
In this study, having a family history of bipolar disorder had no effect on subsequent relapses. In some studies (32, 38), this variable had no significant effect on the increase in subsequent recurrences. However, in studies, (39, 40) having a family history of bipolar disorder increased the risk of relapse. This may be because of a history of having parents or relatives with the disorder, which may increase the risk of disorder in these people than the public population, but it does not necessarily increase the relapse in these patients, and also the incidences, such as the death of loved ones, severe stress, physical illness, etc. may increase the relapse in these patients.
One of the biggest problems of physicians facing chronic and mental illnesses is the lack of patient adherence to treatment (41). Although the rate of non-adherence to treatment varies in mental illnesses, it is approximately 50% in bipolar disorder (42, 43). In this study, this rate was 54.7%. In one study from eight European countries, it was estimated that approximately 57% of patients with bipolar had no medication adherence or were partially adherent to treatment (44). In a similar study (30), the rate of non-adherence in type I bipolar patients was reported to be 56.5%. Failure to medication non-adherence increases the risk of relapse and suicide (45, 46). Various studies have cited reasons, such as side effects of medications, other chronic illnesses, stressful life events, and inappropriate economic status for psychiatric patients' failure to medication non-adherence (47, 48).
One of the limitations of this study was its retrospective design; thus, we were unable to assess other possible relapsing factors, such as the disease stigma, bad events of life, social support, and family support due to the lack of information needed in the patient's file or the lack of cooperation in telephone calls. Another limitation was the use of the self-report tool to measure adherence in patients. This method, although is associated with high specificity and low sensitivity, may also overestimate adherence. Therefore, it is recommended to design a prospective study, in which all possible factors related to the relapse of bipolar patients are measured.
5.1. Conclusion
Bipolar I disorder, as a mental disorder with a relapsing nature, affects not only the patient's performance but also his or her family. This study, using Poisson regression analysis, showed that early age at the onset of illness, being divorced or widowed, cigarette smoking, winter birth, and the lack of therapeutic adherence were risk factors for subsequent relapses in bipolar patients. Consequently, since the changing role of cigarette smoking and medication adherence are more controllable than other variables; therefore, preventive and therapeutic measures to reduce or stop smoking and to establish psychological and educational counseling programs seem to be necessary and helpful for increasing medication adherence.
Acknowledgements
References
-
1.
Sadock BJ, Sadock VA, Williams L, Ott CA. Book Review: Kaplan & Sadock's Pocket Handbook of Clinical Psychiatry, 5th Edition. Annals of Pharmacotherapy. 2010;44(10):1684. https://doi.org/10.1345/aph.1P356.
-
2.
Wang M, Alexanderson K, Runeson B, Mittendorfer-Rutz E. Sick-leave measures, socio-demographic factors and health care as risk indicators for suicidal behavior in patients with depressive disorders--a nationwide prospective cohort study in Sweden. J Affect Disord. 2015;173:201-10. [PubMed ID: 25462417]. https://doi.org/10.1016/j.jad.2014.10.069.
-
3.
Merikangas KR, Jin R, He JP, Kessler RC, Lee S, Sampson NA, et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry. 2011;68(3):241-51. [PubMed ID: 21383262]. [PubMed Central ID: PMC3486639]. https://doi.org/10.1001/archgenpsychiatry.2011.12.
-
4.
American Psychiatrie Association. Diagnostic and statistical manu al of mental disorders. Washington, DC: American Psychiatrie Publishing; 2007.
-
5.
Francisco M, van den Bruinhorst A, Kroon MC. Low-transition-temperature mixtures (LTTMs): a new generation of designer solvents. Angew Chem Int Ed Engl. 2013;52(11):3074-85. [PubMed ID: 23401138]. https://doi.org/10.1002/anie.201207548.
-
6.
Morris CD, Miklowitz DJ, Wisniewski SR, Giese AA, Thomas MR, Allen MH. Care satisfaction, hope, and life functioning among adults with bipolar disorder: data from the first 1000 participants in the Systematic Treatment Enhancement Program. Compr Psychiatry. 2005;46(2):98-104. [PubMed ID: 15723025]. https://doi.org/10.1016/j.comppsych.2004.07.026.
-
7.
Birmaher B, Axelson D, Goldstein B, Strober M, Gill MK, Hunt J, et al. Four-year longitudinal course of children and adolescents with bipolar spectrum disorders: the Course and Outcome of Bipolar Youth (COBY) study. Am J Psychiatry. 2009;166(7):795-804. [PubMed ID: 19448190]. [PubMed Central ID: PMC2828047]. https://doi.org/10.1176/appi.ajp.2009.08101569.
-
8.
Carlson GA, Kotov R, Chang SW, Ruggero C, Bromet EJ. Early determinants of four-year clinical outcomes in bipolar disorder with psychosis. Bipolar Disord. 2012;14(1):19-30. [PubMed ID: 22329469]. [PubMed Central ID: PMC3281503]. https://doi.org/10.1111/j.1399-5618.2012.00982.x.
-
9.
Goldstein TR, Ha W, Axelson DA, Goldstein BI, Liao F, Gill MK, et al. Predictors of prospectively examined suicide attempts among youth with bipolar disorder. Arch Gen Psychiatry. 2012;69(11):1113-22. [PubMed ID: 22752079]. [PubMed Central ID: PMC3600896]. https://doi.org/10.1001/archgenpsychiatry.2012.650.
-
10.
Pavuluri MN, O'Connor MM, Harral EM, Moss M, Sweeney JA. Impact of neurocognitive function on academic difficulties in pediatric bipolar disorder: A clinical translation. Biol Psychiatry. 2006;60(9):951-6. [PubMed ID: 16730333]. https://doi.org/10.1016/j.biopsych.2006.03.027.
-
11.
Wilens TE, Martelon M, Anderson JP, Shelley-Abrahamson R, Biederman J. Difficulties in emotional regulation and substance use disorders: a controlled family study of bipolar adolescents. Drug Alcohol Depend. 2013;132(1-2):114-21. [PubMed ID: 23422834]. [PubMed Central ID: PMC3683118]. https://doi.org/10.1016/j.drugalcdep.2013.01.015.
-
12.
Hirschfeld RM, Calabrese JR, Weissman MM, Reed M, Davies MA, Frye MA, et al. Screening for bipolar disorder in the community. J Clin Psychiatry. 2003;64(1):53-9. [PubMed ID: 12590624]. https://doi.org/10.4088/jcp.v64n0111.
-
13.
Murray CJ, Lopez AD; World Health Organization. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020: summary. Harvard School of Public Health; 1996.
-
14.
Pallaskorpi S, Suominen K, Ketokivi M, Mantere O, Arvilommi P, Valtonen H, et al. Five-year outcome of bipolar I and II disorders: findings of the Jorvi Bipolar Study. Bipolar Disord. 2015;17(4):363-74. [PubMed ID: 25726951]. https://doi.org/10.1111/bdi.12291.
-
15.
Kessing LV, Hansen MG, Andersen PK, Angst J. The predictive effect of episodes on the risk of recurrence in depressive and bipolar disorders - a life-long perspective. Acta Psychiatr Scand. 2004;109(5):339-44. [PubMed ID: 15049770]. https://doi.org/10.1046/j.1600-0447.2003.00266.x.
-
16.
Johnson NL, Kemp AW, Kotz S. Univariate discrete distributions. John Wiley & Sons; 2005. https://doi.org/10.1002/0471715816.
-
17.
Races P. Poisson distribution. 1988.
-
18.
Agresti A. Categorical data analysis. John Wiley & Sons; 2002. https://doi.org/10.1002/0471249688.
-
19.
Long JS. Regression models for categorical and limited dependent variables. Thousand Oaks, California: SAGE Publications; 1997.
-
20.
Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich). 2008;10(5):348-54. [PubMed ID: 18453793]. [PubMed Central ID: PMC2562622]. https://doi.org/10.1111/j.1751-7176.2008.07572.x.
-
21.
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67-74. [PubMed ID: 3945130]. https://doi.org/10.1097/00005650-198601000-00007.
-
22.
McCullagh P, Nelder JA. Generalized linear models. Standard book on generalized linear models. 2nd ed ed. London: Chapman and Hall; 1989. https://doi.org/10.1007/978-1-4899-3242-6.
-
23.
Cakir S, Ozerdem A. [Psychotherapeutic and psychosocial approaches in bipolar disorder: a systematic literature review]. Turk Psikiyatri Derg. 2010;21(2):143-54. [PubMed ID: 20514565].
-
24.
Angst J, Gamma A, Sellaro R, Lavori PW, Zhang H. Recurrence of bipolar disorders and major depression. A life-long perspective. Eur Arch Psychiatry Clin Neurosci. 2003;253(5):236-40. [PubMed ID: 14504992]. https://doi.org/10.1007/s00406-003-0437-2.
-
25.
TAHERI SS, KHODAYIE AMR, karimlou M, Rahgozar M. Identifying risk factors of time to releases in patients with bipolar disorder using penalized likelihood model with shared gamma frailty compared with with-out frailty model. RAZI JOURNAL OF MEDICAL SCIENCES. 2016;23(142):42-9.
-
26.
Gholizadeh A, Kheiri S, Sedehi M, Esmaily H, Arab Borzou Z. Identification of some individual and social factors on relapse intervals in bipolar disorder: Bayesian analysis of log-skew-normal accelerated failure time model. Koomesh. 2018;20(2):384-90.
-
27.
Sajatovic M, Valenstein M, Blow FC, Ganoczy D, Ignacio RV. Treatment adherence with antipsychotic medications in bipolar disorder. Bipolar Disord. 2006;8(3):232-41. [PubMed ID: 16696824]. https://doi.org/10.1111/j.1399-5618.2006.00314.x.
-
28.
Ghoreishizadeh MA, Ranjbar F, Pezeshki MZ. Risk factors in relapse bipolar I mood disorder and its relationship with demographic characteristics. Medical Journal of Tabriz University of Medical Science & Health Service. 2009;(2):6.
-
29.
Pickett-Schenk SA, Cook JA, Laris A. Journey of Hope program outcomes. Community Ment Health J. 2000;36(4):413-24. [PubMed ID: 10917275]. https://doi.org/10.1023/a:1001913013197.
-
30.
Rosca P, Bauer A, Grinshpoon A, Khawaled R, Mester R, Ponizovsky AM. Rehospitalizations among psychiatric patients whose first admission was involuntary: a 10-year follow-up. Israel Journal of Psychiatry and Related Sciences. 2006;43(1):57.
-
31.
Najafi Vosough R, Ghaleiha A, Faradmal J, Mahjub H. Factors Affecting the Risk of Mental Disorders in Patients With Bipolar Disorder in the West of Iran. Avicenna Journal of Neuro Psych Physiology. 2016;3(1). https://doi.org/10.17795/ajnpp-37911.
-
32.
Vejdani-aram S, Fardmal J, Roshanaei G, Najafi-Vosough R, Mahjub H, Ghaleiha A. Identifying the Factors Influencing the Recurrence Time of Bipolar I Disorder Using Frailty Model. Journal of Mazandaran University of Medical Sciences. 2017;27(148):56-67.
-
33.
Kato C, Petronis A, Okazaki Y, Tochigi M, Umekage T, Sasaki T. Molecular genetic studies of schizophrenia: challenges and insights. Neuroscience Research. 2002;43(4):295-304. https://doi.org/10.1016/s0168-0102(02)00064-0.
-
34.
Tochigi M, Marumo K, Hibino H, Otowa T, Kato C, Marui T, et al. Season of birth effect on personality in a general population. Neurosci Lett. 2004;365(2):120-3. [PubMed ID: 15245791]. https://doi.org/10.1016/j.neulet.2004.04.064.
-
35.
Torrey E, Miller J, Rawlings R, Yolken RH. Seasonality of births in schizophrenia and bipolar disorder: a review of the literature. Schizophrenia Research. 1997;28(1):1-38. https://doi.org/10.1016/s0920-9964(97)00092-3.
-
36.
Ostacher MJ, Nierenberg AA, Perlis RH, Eidelman P, Borrelli DJ, Tran TB, et al. The relationship between smoking and suicidal behavior, comorbidity, and course of illness in bipolar disorder. J Clin Psychiatry. 2006;67(12):1907-11. [PubMed ID: 17194268]. https://doi.org/10.4088/jcp.v67n1210.
-
37.
Sadock BJ, Sadock VA. Kaplan and Sadock's synopsis of psychiatry: Behavioral sciences/clinical psychiatry. Lippincott Williams & Wilkins; 2011.
-
38.
Lin CH, Chen MC, Chou LS, Lin CH, Chen CC, Lane HY. Time to rehospitalization in patients with major depression vs. those with schizophrenia or bipolar I disorder in a public psychiatric hospital. Psychiatry Res. 2010;180(2-3):74-9. [PubMed ID: 20494450]. https://doi.org/10.1016/j.psychres.2009.12.003.
-
39.
Ostergaard SD, Waltoft BL, Mortensen PB, Mors O. Environmental and familial risk factors for psychotic and non-psychotic severe depression. J Affect Disord. 2013;147(1-3):232-40. [PubMed ID: 23228568]. https://doi.org/10.1016/j.jad.2012.11.009.
-
40.
Yazdani-Charati J, Zarghami M, Saadat S. Determining the factors affecting recurrence in bipolar I disorder using Andersen-Gill counting process model. Journal of Mazandaran University of Medical Sciences. 2014;23(108):83-9.
-
41.
Lindenmayer JP, Liu-Seifert H, Kulkarni PM, Kinon BJ, Stauffer V, Edwards SE, et al. Medication nonadherence and treatment outcome in patients with schizophrenia or schizoaffective disorder with suboptimal prior response. J Clin Psychiatry. 2009;70(7):990-6. [PubMed ID: 19497244]. https://doi.org/10.4088/JCP.08m04221.
-
42.
Miasso AI, do Carmo BP, Tirapelli CR. [Bipolar affective disorder: pharmacotherapeutic profile and adherence to medication]. Rev Esc Enferm USP. 2012;46(3):689-95. [PubMed ID: 22773491]. https://doi.org/10.1590/s0080-62342012000300022.
-
43.
Sajatovic M, Elhaj O, Youngstrom EA, Bilali SR, Rapport DJ, Ganocy SJ, et al. Treatment adherence in individuals with rapid cycling bipolar disorder: results from a clinical-trial setting. J Clin Psychopharmacol. 2007;27(4):412-4. [PubMed ID: 17632236]. https://doi.org/10.1097/01.jcp.0000280310.50871.ff.
-
44.
Vieta E, Azorin JM, Bauer M, Frangou S, Perugi G, Martinez G, et al. Psychiatrists' perceptions of potential reasons for non- and partial adherence to medication: results of a survey in bipolar disorder from eight European countries. J Affect Disord. 2012;143(1-3):125-30. [PubMed ID: 22840608]. https://doi.org/10.1016/j.jad.2012.05.041.
-
45.
Gigante AD, Lafer B, Yatham LN. Long-acting injectable antipsychotics for the maintenance treatment of bipolar disorder. CNS Drugs. 2012;26(5):403-20. [PubMed ID: 22494448]. https://doi.org/10.2165/11631310-000000000-00000.
-
46.
Samalin L, Nourry A, Charpeaud T, Llorca PM. What is the evidence for the use of second-generation antipsychotic long-acting injectables as maintenance treatment in bipolar disorder? Nord J Psychiatry. 2014;68(4):227-35. [PubMed ID: 23795859]. https://doi.org/10.3109/08039488.2013.801078.
-
47.
Lingam R, Scott J. Treatment non-adherence in affective disorders. Acta Psychiatr Scand. 2002;105(3):164-72. [PubMed ID: 11939969]. https://doi.org/10.1034/j.1600-0447.2002.1r084.x.
-
48.
Novick D, Haro JM, Suarez D, Perez V, Dittmann RW, Haddad PM. Predictors and clinical consequences of non-adherence with antipsychotic medication in the outpatient treatment of schizophrenia. Psychiatry Res. 2010;176(2-3):109-13. [PubMed ID: 20185182]. https://doi.org/10.1016/j.psychres.2009.05.004.