Abstract
Context:
This study was done to extract the evaluation criteria to assess the effects of decision support systems integrated with computerized provider order entry (CPOE) systems.Methods:
A Scoping review search was carried out on papers published in nine electronic databases, including PubMed, Embase, ProQuest, Scopus, Web of Science, Cochrane, Science Direct, ACM digital library, and IEEE Xplore Digital Library up to February 2019. This study was conducted based on the PRISMA flow diagram. Two investigators independently worked on identifying papers published in English electronic clinical decision supports physicians used that to help decision-making during medical orders. Finally, the criteria for effects of clinical decision support systems (CDSSs) in CPOE were extracted from the selected papers.Results:
Eighty-seven studies were identified matching the inclusion criteria. The most significant number of effects belonged to the medication order decision support system. Medication order decision support system studies were classified into five categories by effects: clinical effects (8 dimensions), the process of care effects (3 dimensions), user workload effects (8 dimensions), economic effects (2 dimensions), and implementation effects (5 dimensions).Conclusions:
It can be concluded that the most substantial effect is related to medication decision supports within the CPOE system. These studies provide wide-ranging criteria to evaluate CDSS integrated into CPOE. It helps identify weaknesses and strengths of CDSSs within CPOE systems.Keywords
Medical Order Entry Systems Computerized Provider Order Entry CPOE Clinical Decision Support Systems CDSS Criteria Outcome Evaluation.
1. Context
Health care organizations use information technology for improving patient care (1). Computerized provider order entry (CPOE) combined with a clinical decision support system (CDSS) is a complex component of the electronic medical record. CPOE is an electronic application the physician or care provider uses to enter order medication, laboratory tests, request imaging, blood bank, and request a consultation. The primary purposes of CPOE include assurance of legibility and completeness of provider orders (2, 3). Much of the potential value of CPOE come from clinical decision support tools that can help a physician improve clinical decision-making at the point of care (4).
CDSS in provider order entry system includes drug-drug interaction checking, drug-allergy checking, drug-age checking, drug dose calculating, restricting transfusion orders, and detecting unnecessary diagnostic tests (5). The CDSS is embedded in medication orders, transfusion orders, requests for medical images, and laboratory test order. CDSS embedded in CPOE contributes to improving patient safety, preventing waste of the cost of care, and promoting health care services (4).
Evaluation of CDSS is required to ensure long-term CDSS integrated into CPOE sustainability, improve care quality (process, structures, and patient outcome). Also, evaluation is essential to ensure the appropriateness of the CDSS. Feedback obtained from the assessment of CDSS performance help to improve the suitability of CDSS.
Despite the increasing use of CPOE combined with CDSS for improving patient safety and reducing the use of services, the effects of CPOE combined with CDSS are unclear. Several studies have examined the impact of clinical decisions integrated into the CPOE system (6-12).
2. Objectives
One study specifically explored the effects of CDSS (13); however, many questions have remained unanswered about CPOE combined with CDSS impact. Then, having the criteria for evaluating the impact of CPOE combined with CDSS is necessary. Accordingly, the present study was conducted as a scoping review to identify the criteria for assessing the effects of CDSS integrated with CPOE.
3. Methods
This scoping review investigated the effects of CDSS integrated into CPOE. Any types of clinical decision support (alert, reminder, info button, and relevant information) presented to physicians during medical order entry (from initial order to submit the order) and published until February 2019 in English were included in the present study. However, thesis/dissertation, proceeding papers, conference papers, letters to the editor, short communications, unpublished articles, and non-English language papers were excluded in the final stage of screening.
To collect relevant studies, a systematic search was carried out using databases from inception to February 2019. To make sure that there were no other similar systematic reviews, a rapid search was conducted on Cochrane library databases to find a possible systematic article related to the metrics evaluating the effects of intervention (medical order entry system with decision support). Then, nine information databases, including PubMed, Embase, ProQuest, Scopus, Web of Science, Cochrane, Science Direct, ACM digital library, IEEE Xplore Digital Library, were searched. In all search stages, the results were reviewed by other individuals and approved.
The search was conducted with relatively common terms using synonymous words and "OR" operators. To achieve more specificity, the search was implemented with synonymous words and the "AND" operator. The "MeSH terminology" keyword in the PubMed database and the "Emtree terminology" keyword in the Embase database were also used to find terms related to articles (Table 1). The search strategy was approved by a senior medical librarian.
Search Strategy to Investigate the Effects of Computerized Provider Order Entry Combined with Decision Support Systems
| Database | PubMed, Embase, ProQuest, Scopus, Web of Science, Cochrane, Science Direct, ACM digital library, IEEE Xplore Digital Library |
|---|---|
| Search strategy | #1 AND #2 AND #3 |
| #1 | "Medical Order Entry Systems" OR "CPOE" OR "Computerized Order Entry" OR "Computerized Prescriber Order Entry" OR "Computerized Provider Order Entry" OR "Electronic Order" OR "Electronic Prescribing" OR "Electronic Physician Order Entry" OR "Computerized Physician Order Entry" |
| #2 | "Clinical Decision Support Systems" OR "Clinical Computerized Decision Support Systems" OR "Decision-Support Systems" OR "Reminder Systems" OR "Computer-Assisted Decision-Making" OR " Computer-Assisted Therapy " OR "Expert Systems" OR "Alert System" OR "Clinical Decision Support Alert" OR "Formulary Decision Support" |
| #3 | "Impact" OR "Effect" OR "Mortality" OR "Length Of Stay" OR "Medication Errors" OR "Drug Side Effects" OR "Adverse Reactions" OR "Readmission" OR "Hospitalization Cost" OR "Treatment Cost" OR "Hospital Acquired Infection" OR "Nosocomial Infection" OR "Patient Outcome" OR "Clinician Performance" OR "Satisfaction" |
The required information was extracted using a collection form. This form included the journal name, article title, study design, study date, research sample, data collection tools, intervention (medical order entry with decision support), intervention effects, and conclusion. All forms were developed item by item. In the extraction stage, one of the authors inserted the data into the form, and other authors reassurance them. In case of disagreements between the two authors, a third author resolved the issue.
Two authors screened the titles and abstracts. Data abstracted were categorized according to the medical order type (medication order, radiology orders, laboratory order, and blood bank order). The effects of CPOE combined with CDSS were captured using a narrative review. Effects of electronic medication orders with CDSS were classified using the taxonomy described by Bright et al. (13).
4. Results
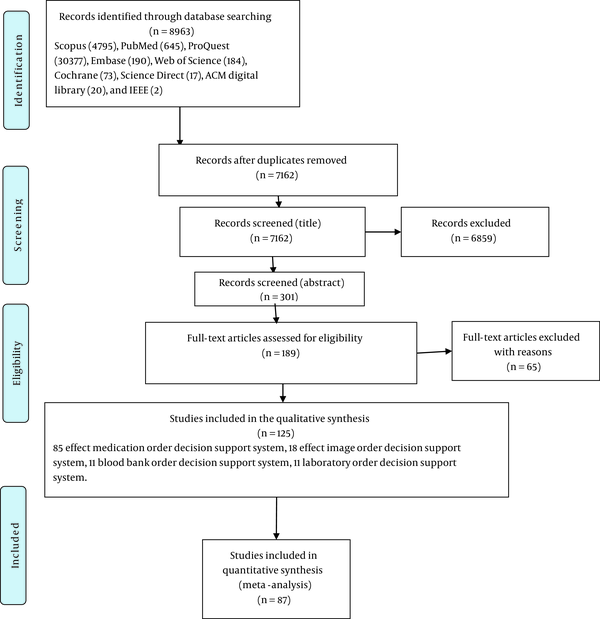
The literature search was conducted in February 2019 initially and identified a total of 8963 possible articles, and after removing duplicates, 7162 records remained. A three-stage review process was employed (title, abstract, and full text). In the first and second stages, two reviewers screened all titles and abstracts for relevancy and eliminated articles that did not meet the inclusion criteria. Following the first-stage screening, 301 articles were retrieved and reviewed, and one reviewer conducted the third-stage screening process. Further 125 eligible studies were included. The flow diagram of study selection is shown in Figure 1. Then, 38 studies were eliminated because their publication date was before 2013, and there were similar studies published after 2013. However, the publication date of four studies was before 2013, and there was not similar study after 2013. Finally, 87 studies were included.
PRISMA flow diagram
The effect of decision support combined with the CPOE was classified by the order type. The largest effects item of decision support with the medical order entry system belonged to medication orders. Most of the studies had evaluated the effectiveness of decision support during medication order on medication errors, length of stay in the ward and hospital, mortality in the ward and hospital, compliance with standardizing therapy, and physician response to alerts. However, very few publications had evaluated the impact of decision support during a medication order on re-admission, mechanical ventilation duration, antimicrobial resistance, user workload, and efficiency time. Twenty-six effects related to the decision support integrated into the medication order entry system are reported in Table 2.
Effects of Decision Support Integrated into Medication Order Entry System
| Number | Categoriy | Reference Count | Reference |
|---|---|---|---|
| Clinical effects | |||
| 1 | Medication errors | 17 | (6, 9-11, 14-28) |
| 2 | Hospital mortality | 5 | (11, 17, 25, 29-31) |
| 3 | Length of stay | 7 | (11, 17, 19, 25, 30, 32, 33) |
| 4 | Adverse drug event | 3 | (25, 29, 34) |
| 5 | Re-admission | 1 | (17) |
| 6 | Mechanical ventilation duration | 1 | (35) |
| 7 | Patient safety/falling rate | 4 | (21, 22, 36-38) |
| 8 | Antimicrobial resistance | 1 | (30) |
| Process of care effects | |||
| 9 | Adherence to standardized care | 13 | (16, 19, 23, 30, 36, 39-49) |
| 10 | Medication discontinuation | 3 | (21, 31, 50) |
| 11 | The time of the chemotherapy process | 1 | (6) |
| User workload and efficiency effects | |||
| 12 | Clinician and clinical pharmacy Workload | 4 | (14, 23, 36, 51) |
| 13 | Time required to enter medication order | 2 | (19, 52) |
| 14 | Workflow (changes in work practices) | 1 | (19) |
| 15 | Staff time efficiency | 1 | (19) |
| 16 | Reduction in team-wide discussions | 1 | (19) |
| 17 | Education | 1 | (53) |
| 18 | Pharmacist–physician communication | 1 | (54) |
| 19 | Alert burden on users | 2 | (19, 55) |
| Economic effects | |||
| 20 | Drug costs | 5 | (17, 29, 30, 56, 57) |
| 21 | Usage of medication | 3 | (19, 30, 58) |
| Use and implementation effects | |||
| 22 | Frequency of alerts | 7 | (19, 32, 50, 55, 59-62) |
| 23 | Physician response to an alert | 3 | (31, 59, 62) |
| 24 | Number of orders canceled | 1 | (63) |
| 25 | Usability | 2 | (9, 19) |
| 26 | Rate of order set use | 1 | (64) |
The majority of studies had evacuated the effectiveness of decision support during a medical image order entry on medical image appropriate order and medical image utilization. On the other hand, fewer studies had evaluated the impact of decision support during image requests on turnaround time, repeated tests, and user compliance to the regulations. Six effects related to decision support during medical image requests are shown in Table 3.
Effects of Decision Support During Medical Image Request
Most studies had explored the effectiveness of decision support integrated into laboratory test order entry on usage of laboratory resources, unnecessary and duplicate orders, costs, and user satisfaction. However, only a few studies had evaluated the impact of decision support into laboratory test order entry on workflow, user compliance with guidelines, mortality, and length of stay. Eleven effects related to decision support integrated into laboratory test order entry are outlined in Table 4.
Effects of Decision Support Integrated into Laboratory Test Order Entry
| Number | Effects | Reference Count | Reference |
|---|---|---|---|
| 1 | Usage of laboratory resource | 5 | (77-81) |
| 2 | Mortality (secondary outcome) | 1 | (80) |
| 3 | Length of stay | 1 | (80) |
| 4 | Cost | 4 | (77, 80, 82, 83) |
| 5 | User satisfaction | 2 | (79, 83) |
| 6 | Compliance with guideline | 1 | (12) |
| 7 | Unnecessary and duplicate ordering | 3 | (82, 84, 85) |
| 9 | Effective patient care | 1 | (86) |
| 10 | Change physician test-ordering behavior | 1 | (83) |
| 11 | Impact on workflow | 1 | (83) |
Many studies had assessed the effectiveness of decision support integrated into blood products orders entry on the usage of blood products, compliance with guidelines, and reducing the use of unnecessary blood products. However, sparse research had tested the impact of decision support integrated into blood products order entry on blood product costs, mortality, and length of stay. Six effects related to decision support integrated into blood products order entry are summarized in Table 5.
Effects of Decision Support Integrated into Blood Products Order Entry
5. Discussion
This study showed that the main category evaluation criteria for CDSS integrated into CPOE included four categories of evaluation criteria for decision support integrated into medication order entry system, decision support during medical image order entry, decision support integrated into laboratory test order entry, and decision support integrated into blood products order entry. The main evaluation criteria can be regarded as the process of care, structure, and patient outcome. To the best of our knowledge, this is the first scoping review determining the criteria for evaluating the effects of implementation CDSS integrated into the CPOE in the clinical setting. These types of studies are carried out for preliminary evaluation of the scope of available research literature on the effects of CPOE combined with CDSS.
CPOE combined with CDSS can help physicians in decision-making at the point of care. CDSS integrated into CPOE is employed to prevent medication error, improve patient care, enhance patient safety, reduce costs, and increase physician adherence to standardized care. Decision support can be embedded into all types of medical order, including medication order, laboratory test order, medical image order, and blood product requests. According to this review, most studies had dealt with the decision support embedded within the medication order entry system on medication error (drug-drug interaction, drug-allergy interaction, drug-lab interaction, dose error, and drug-condition interaction). Clinical decision support embedded within medication order reduces medication error. Ranji et al. found that CDSS integrated into CPOE dramatically reduced medication error (18). The primary objective of CPOE combined with CDSS is to reduce medication error. Then, CPOE with CDSS prevents medication error. On the other hand, some studies have found that CPOE facilitated medication error (97).
According to this study results, the effects of the implementation of clinical decision support integrated into medication order entry system should be examined on adverse drug events since it is unclear (98) and there is not a uniform way to collect adverse drug event data.
Some studies had evaluated the effects of implementing the clinical decision support embedded within medication order on hospital mortality and length of stay in a clinical setting. Prgomet et al. found that computerized decision support embedded within CPOE reduced hospital mortality rate and length of stay (11). Most studies assessing the effect of CPOE with CDSS on hospital mortality and length of stay did not apply a high-quality method, such as randomized control trial.
Many studies had evaluated the effects of implementation of CDSS integrated into a CPOE on adherence to standardize care. Many studies had demonstrated that E-prescribing with decision support could enhance adherence to standardize care (44, 46). One of the best strategies to conduct health care policy is implementing policy on CPOE.
Decision support embedded within medication orders affects the rate of medication discontinuation. On the other hand, few studies had evaluated the effects of decision support integrated into CPOE on this rate (21). Close loop workflow integrated with CDS embedded within CPOE can reduce the rate of medication discontinuation and help in tracking orders.
The effects of implementation of decision support embedded within medication order on clinician and clinical pharmacy workload are controversial. Sparse studies have been carried out on the effect of medication order with decision support (36, 51). Clinical decision support embedded within CPOE can increase workload because of the need to taking more steps for the entry of information.
Regarding the impact of decision support embedded within medication order on drug cost and drug usage, Fischer et al. found that CPOE with a CDSS would reduce the drug cost and drug usage (99) because drug cost affects clinician decision-making regarding care and clinical decision support can restrict inappropriate prescription.
Many studies, such as a study conducted by McCoy et al. (100) had evaluated physician response to decision support embedded within the medication order entry system. Nevertheless, a few studies have been conducted on the usability and functionality of clinical decision support embedded within the CPOE. Usability evaluation is imperative for assurance of learnability, ease of use, memorizing, and user satisfaction with the information system.
The majority of studies had evaluated the effects of decision support integrated into medical image order entry system on inappropriateness order. These results are similar to those reported by Goldzweig et al. (70). Unnecessary medical image order is common. Furthermore, unnecessary medical image order increases health care service costs. As a result, the rate of the unsatisfied user from healthcare centers increases. CDSS integrated into CPOE can decrease inappropriate medical image orders.
According to our findings, most studies had been performed on decision support systems in the laboratory order context, and evaluated the effect of decision support integrated into laboratory test order entry system on laboratory resource usage and laboratory test cost. Eaton et al. observed that laboratory test order entry with decision support can reduce laboratory resource usage and laboratory test cost (78). Approximately half of the orders in health care centers are unnecessary. Clinical decision support integrated into CPOE may restrict laboratory tests, identify redundant order, and display past laboratory results.
Most studies had evaluated the impact of decision support integrated into the blood products order entry system on blood products usage and provider compliance with the guideline. Hibbs et al. found that decision support applied to transfusion order enhanced transfusion practice (89). The rule-based decision supports transfusion order and limits blood bank order, and consequently, clinician practice compliances with standard care.
This study introduced a list of criteria for evaluating the implementation of CDSS combined with CPOE. It helps identify weaknesses and strengths of CDSS combined with CPOE.
There is little evidence on the effect of CDSS combined with CPOE on user workload and efficiency. Further studies for evaluating the effects of decision support integrated into CPOE are essential. Gray literature and conference papers were excluded, which was a limitation. Also, only papers published in the English language were included.
There is evidence that there are logical scientific implications for evaluating successful implementation and effects of CDSS integrated into CPOE in the clinical setting. The findings of the present study offered the key metrics for evaluating the effectiveness of implemented decision support embedded within each medical order type. These studies provide extensive criteria to evaluate CDSS integrated into CPOE. These evaluation criteria can be used to evaluate CDSS integrated into CDSS in practice. Future studies on business intelligence development to present the effects of implementing CDSS integrated into CPOE will help policymakers to assure successful implementation of CDSS integrated into the CPOE. Representing the effects of CDSS integrated into CPOE using visual tools is effective for the management of decision-making.
References
-
1.
Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144(10):742-52. [PubMed ID: 16702590]. https://doi.org/10.7326/0003-4819-144-10-200605160-00125.
-
2.
Kuperman GJ, Teich JM, Gandhi TK, Bates DW. Patient Safety and Computerized Medication Ordering at Brigham and Women’s Hospital. Jt Comm J Qual Improv. 2001;27(10):509-21. https://doi.org/10.1016/s1070-3241(01)27045-x.
-
3.
Khammarnia M, Sharifian R, Zand F, Barati O, Keshtkaran A, Sabetian G, et al. The impact of computerized physician order entry on prescription orders: A quasi-experimental study in Iran. Med J Islam Repub Iran. 2017;31:69. [PubMed ID: 29445698]. [PubMed Central ID: PMC5804463]. https://doi.org/10.14196/mjiri.31.69.
-
4.
Sittig DF, Stead WW. Computer-based physician order entry: the state of the art. J Am Med Inform Assoc. 1994;1(2):108-23. [PubMed ID: 7719793]. [PubMed Central ID: PMC116190]. https://doi.org/10.1136/jamia.1994.95236142.
-
5.
Schiff G, Mirica MM, Dhavle AA, Galanter WL, Lambert B, Wright A. A Prescription For Enhancing Electronic Prescribing Safety. Health Aff (Millwood). 2018;37(11):1877-83. [PubMed ID: 30395495]. https://doi.org/10.1377/hlthaff.2018.0725.
-
6.
Rahimi R, Moghaddasi H, Rafsanjani KA, Bahoush G, Kazemi A. Effects of chemotherapy prescription clinical decision-support systems on the chemotherapy process: A systematic review. Int J Med Inform. 2019;122:20-6. [PubMed ID: 30623780]. https://doi.org/10.1016/j.ijmedinf.2018.11.004.
-
7.
Varghese J, Kleine M, Gessner SI, Sandmann S, Dugas M. Effects of computerized decision support system implementations on patient outcomes in inpatient care: a systematic review. J Am Med Inform Assoc. 2018;25(5):593-602. [PubMed ID: 29036406]. [PubMed Central ID: PMC7646949]. https://doi.org/10.1093/jamia/ocx100.
-
8.
Shanbhag D, Graham ID, Harlos K, Haynes RB, Gabizon I, Connolly SJ, et al. Effectiveness of implementation interventions in improving physician adherence to guideline recommendations in heart failure: A systematic review. BMJ Open. 2018;8(3). e017765. [PubMed ID: 29511005]. [PubMed Central ID: PMC5855256]. https://doi.org/10.1136/bmjopen-2017-017765.
-
9.
Powers EM, Shiffman RN, Melnick ER, Hickner A, Sharifi M. Efficacy and unintended consequences of hard-stop alerts in electronic health record systems: a systematic review. J Am Med Inform Assoc. 2018;25(11):1556-66. [PubMed ID: 30239810]. [PubMed Central ID: PMC6915824]. https://doi.org/10.1093/jamia/ocy112.
-
10.
Reis WC, Bonetti AF, Bottacin WE, Reis AJ, Souza TT, Pontarolo R, et al. Impact on process results of clinical decision support systems (CDSSs) applied to medication use: overview of systematic reviews. Pharm Pract (Granada). 2017;15(4):1036. [PubMed ID: 29317919]. [PubMed Central ID: PMC5741996]. https://doi.org/10.18549/PharmPract.2017.04.1036.
-
11.
Prgomet M, Li L, Niazkhani Z, Georgiou A, Westbrook JI. Impact of commercial computerized provider order entry (CPOE) and clinical decision support systems (CDSSs) on medication errors, length of stay, and mortality in intensive care units: A systematic review and meta-analysis. J Am Med Inform Assoc. 2017;24(2):413-22. [PubMed ID: 28395016]. [PubMed Central ID: PMC7651905]. https://doi.org/10.1093/jamia/ocw145.
-
12.
Delvaux N, Van Thienen K, Heselmans A, de Velde SV, Ramaekers D, Aertgeerts B. The Effects of Computerized Clinical Decision Support Systems on Laboratory Test Ordering: A Systematic Review. Arch Pathol Lab Med. 2017;141(4):585-95. [PubMed ID: 28353386]. https://doi.org/10.5858/arpa.2016-0115-RA.
-
13.
Bright TJ, Wong A, Dhurjati R, Bristow E, Bastian L, Coeytaux RR, et al. Effect of clinical decision-support systems: a systematic review. Ann Intern Med. 2012;157(1):29-43. [PubMed ID: 22751758]. https://doi.org/10.7326/0003-4819-157-1-201207030-00450.
-
14.
Lyell D, Magrabi F, Coiera E. Reduced Verification of Medication Alerts Increases Prescribing Errors. Appl Clin Inform. 2019;10(1):66-76. [PubMed ID: 30699458]. [PubMed Central ID: PMC6353646]. https://doi.org/10.1055/s-0038-1677009.
-
15.
Pontefract SK, Hodson J, Slee A, Shah S, Girling AJ, Williams R, et al. Impact of a commercial order entry system on prescribing errors amenable to computerised decision support in the hospital setting: a prospective pre-post study. BMJ Qual Saf. 2018;27(9):725-36. [PubMed ID: 29572298]. [PubMed Central ID: PMC6109251]. https://doi.org/10.1136/bmjqs-2017-007135.
-
16.
Jia P, Zhang L, Chen J, Zhao P, Zhang M. The Effects of Clinical Decision Support Systems on Medication Safety: An Overview. PLoS One. 2016;11(12). e0167683. [PubMed ID: 27977697]. [PubMed Central ID: PMC5157990]. https://doi.org/10.1371/journal.pone.0167683.
-
17.
Aziz MT, Ur-Rehman T, Qureshi S, Bukhari NI. Reduction in chemotherapy order errors with computerised physician order entry and clinical decision support systems. Health Inf Manag. 2015;44(3):13-22. [PubMed ID: 26464298]. https://doi.org/10.1177/183335831504400303.
-
18.
Ranji SR, Rennke S, Wachter RM. Computerised provider order entry combined with clinical decision support systems to improve medication safety: A narrative review. BMJ Qual Saf. 2014;23(9):773-80. [PubMed ID: 24728888]. https://doi.org/10.1136/bmjqs-2013-002165.
-
19.
Cresswell KM, Bates DW, Williams R, Morrison Z, Slee A, Coleman J, et al. Evaluation of medium-term consequences of implementing commercial computerized physician order entry and clinical decision support prescribing systems in two 'early adopter' hospitals. J Am Med Inform Assoc. 2014;21(e2):e194-202. [PubMed ID: 24431334]. [PubMed Central ID: PMC4173168]. https://doi.org/10.1136/amiajnl-2013-002252.
-
20.
Malte CA, Berger D, Saxon AJ, Hagedorn HJ, Achtmeyer CE, Mariano AJ, et al. Electronic Medical Record Alert Associated With Reduced Opioid and Benzodiazepine Coprescribing in High-risk Veteran Patients. Med Care. 2018;56(2):171-8. [PubMed ID: 29287034]. https://doi.org/10.1097/MLR.0000000000000861.
-
21.
Scott IA, Pillans PI, Barras M, Morris C. Using EMR-enabled computerized decision support systems to reduce prescribing of potentially inappropriate medications: a narrative review. Ther Adv Drug Saf. 2018;9(9):559-73. [PubMed ID: 30181862]. [PubMed Central ID: PMC6116772]. https://doi.org/10.1177/2042098618784809.
-
22.
Vanderman AJ, Moss JM, Bryan W3, Sloane R, Jackson GL, Hastings SN. Evaluating the Impact of Medication Safety Alerts on Prescribing of Potentially Inappropriate Medications for Older Veterans in an Ambulatory Care Setting. J Pharm Pract. 2017;30(1):82-8. [PubMed ID: 26702027]. https://doi.org/10.1177/0897190015621803.
-
23.
Desmedt S, Spinewine A, Jadoul M, Henrard S, Wouters D, Dalleur O. Impact of a clinical decision support system for drug dosage in patients with renal failure. Int J Clin Pharm. 2018;40(5):1225-33. [PubMed ID: 29785684]. https://doi.org/10.1007/s11096-018-0612-1.
-
24.
Hamad A, Cavell G, Hinton J, Wade P, Whittlesea C. A pre-postintervention study to evaluate the impact of dose calculators on the accuracy of gentamicin and vancomycin initial doses. BMJ Open. 2015;5(6). e006610. [PubMed ID: 26044758]. [PubMed Central ID: PMC4458600]. https://doi.org/10.1136/bmjopen-2014-006610.
-
25.
Gillaizeau F, Chan E, Trinquart L, Colombet I, Walton RT, Rege-Walther M, et al. Computerized advice on drug dosage to improve prescribing practice. Cochrane Database Syst Rev. 2013;(11). CD002894. [PubMed ID: 24218045]. https://doi.org/10.1002/14651858.CD002894.pub3.
-
26.
McKibben S, De Simoni A, Bush A, Thomas M, Griffiths C. The use of electronic alerts in primary care computer systems to identify the excessive prescription of short-acting beta2-agonists for people with asthma: a systematic review. NPJ Prim Care Respir Med. 2018;28(1):14. [PubMed ID: 29662064]. [PubMed Central ID: PMC5902442]. https://doi.org/10.1038/s41533-018-0080-z.
-
27.
Hou J, Cheng K, Bai K, Chen H, Wu W, Lin Y, et al. The effect of a computerized pediatric dosing decision support system on pediatric dosing errors. J Food Drug Anal. 2013;21(3):286-91. https://doi.org/10.1016/j.jfda.2013.07.006.
-
28.
Lee J, Han H, Ock M, Lee SI, Lee S, Jo MW. Impact of a clinical decision support system for high-alert medications on the prevention of prescription errors. Int J Med Inform. 2014;83(12):929-40. [PubMed ID: 25256067]. https://doi.org/10.1016/j.ijmedinf.2014.08.006.
-
29.
Prasert V, Shono A, Chanjaruporn F, Ploylearmsang C, Boonnan K, Khampetdee A, et al. Effect of a computerized decision support system on potentially inappropriate medication prescriptions for elderly patients in Thailand. J Eval Clin Pract. 2019;25(3):514-20. [PubMed ID: 30484935]. https://doi.org/10.1111/jep.13065.
-
30.
Curtis CE, Al Bahar F, Marriott JF. The effectiveness of computerised decision support on antibiotic use in hospitals: A systematic review. PLoS One. 2017;12(8). e0183062. [PubMed ID: 28837665]. [PubMed Central ID: PMC5570266]. https://doi.org/10.1371/journal.pone.0183062.
-
31.
Lachance P, Villeneuve PM, Rewa OG, Wilson FP, Selby NM, Featherstone RM, et al. Association between e-alert implementation for detection of acute kidney injury and outcomes: a systematic review. Nephrol Dial Transplant. 2017;32(2):265-72. [PubMed ID: 28088774]. [PubMed Central ID: PMC6251638]. https://doi.org/10.1093/ndt/gfw424.
-
32.
Bayoumi I, Al Balas M, Handler SM, Dolovich L, Hutchison B, Holbrook A. The effectiveness of computerized drug-lab alerts: a systematic review and meta-analysis. Int J Med Inform. 2014;83(6):406-15. [PubMed ID: 24793784]. https://doi.org/10.1016/j.ijmedinf.2014.03.003.
-
33.
Pendharkar SR, Ospina MB, Southern DA, Hirani N, Graham J, Faris P, et al. Effectiveness of a standardized electronic admission order set for acute exacerbation of chronic obstructive pulmonary disease. BMC Pulm Med. 2018;18(1):93. [PubMed ID: 29843772]. [PubMed Central ID: PMC5975274]. https://doi.org/10.1186/s12890-018-0657-x.
-
34.
Durieux P, Trinquart L, Colombet I, Niès J, Walton RT, Rajeswaran A, et al. Computerized advice on drug dosage to improve prescribing practice. Cochrane Database of Systematic Reviews. Cochrane Database Syst Rev; 2008. https://doi.org/10.1002/14651858.CD002894.pub2.
-
35.
Al-Dorzi HM, Tamim HM, Cherfan A, Hassan MA, Taher S, Arabi YM. Impact of computerized physician order entry (CPOE) system on the outcome of critically ill adult patients: a before-after study. BMC Med Inform Decis Mak. 2011;11:71. [PubMed ID: 22098683]. [PubMed Central ID: PMC3248372]. https://doi.org/10.1186/1472-6947-11-71.
-
36.
Wolf M, Miller S, DeJong D, House JA, Dirks C, Beasley B. The process of development of a prioritization tool for a clinical decision support build within a computerized provider order entry system: Experiences from St Luke's Health System. Health Informatics J. 2016;22(3):579-93. [PubMed ID: 25814483]. https://doi.org/10.1177/1460458215571769.
-
37.
Marasinghe KM. Computerised clinical decision support systems to improve medication safety in long-term care homes: a systematic review. BMJ Open. 2015;5(5). e006539. [PubMed ID: 25967986]. [PubMed Central ID: PMC4431065]. https://doi.org/10.1136/bmjopen-2014-006539.
-
38.
Weersink RA, Bouma M, Burger DM, Drenth JPH, Harkes-Idzinga SF, Hunfeld NGM, et al. Evidence-Based Recommendations to Improve the Safe Use of Drugs in Patients with Liver Cirrhosis. Drug Saf. 2018;41(6):603-13. [PubMed ID: 29330714]. [PubMed Central ID: PMC5966501]. https://doi.org/10.1007/s40264-017-0635-x.
-
39.
Yoon CH, Ritchie SR, Duffy EJ, Thomas MG, McBride S, Read K, et al. Impact of a smartphone app on prescriber adherence to antibiotic guidelines in adult patients with community acquired pneumonia or urinary tract infections. PLoS One. 2019;14(1). e0211157. [PubMed ID: 30695078]. [PubMed Central ID: PMC6350960]. https://doi.org/10.1371/journal.pone.0211157.
-
40.
Arias Pou P, Aquerreta Gonzalez I, Idoate Garcia A, Garcia-Fernandez N. Improvement of drug prescribing in acute kidney injury with a nephrotoxic drug alert system. Eur J Hosp Pharm. 2019;26(1):33-8. [PubMed ID: 31157093]. [PubMed Central ID: PMC6362774]. https://doi.org/10.1136/ejhpharm-2017-001300.
-
41.
Pereboom M, Mulder IJ, Verweij SL, van der Hoeven RTM, Becker ML. A clinical decision support system to improve adequate dosing of gentamicin and vancomycin. Int J Med Inform. 2019;124:1-5. [PubMed ID: 30784421]. https://doi.org/10.1016/j.ijmedinf.2019.01.002.
-
42.
Gunn LR, Tunney R, Kelly K. Nonmodal Clinical Decision Support and Antimicrobial Restriction Effects on Rates of Fluoroquinolone Use in Uncomplicated Infections. Appl Clin Inform. 2018;9(1):149-55. [PubMed ID: 29490408]. [PubMed Central ID: PMC5830158]. https://doi.org/10.1055/s-0038-1626726.
-
43.
Lilih S, Pereboom M, van der Hoeven RT, Mantel-Teeuwisse AK, Becker ML. Improving the effectiveness of drug safety alerts to increase adherence to the guideline for gastrointestinal prophylaxis. Int J Med Inform. 2017;97:139-44. [PubMed ID: 27919373]. https://doi.org/10.1016/j.ijmedinf.2016.10.002.
-
44.
Joseph SB, Sow M. E-Prescribing With Decision Support Is Associated With Improvements in Medication Adherence. Am J Pharm. 2016;8(4):133-40.
-
45.
Jajosky J, Howell SM, Honaker J, Moriarty A, Shea JM. Improving Adherence to Practice Guidelines for Anticoagulation in Patients Receiving Neuraxial Anesthesia Using an Electronic Order Entry Alert System. J Patient Saf. 2015;15(3):218-23. [PubMed ID: 26076079]. [PubMed Central ID: PMC7392164]. https://doi.org/10.1097/PTS.0000000000000219.
-
46.
Helmons PJ, Coates CR, Kosterink JG, Daniels CE. Decision support at the point of prescribing to increase formulary adherence. Am J Health Syst Pharm. 2015;72(5):408-13. [PubMed ID: 25694416]. https://doi.org/10.2146/ajhp140388.
-
47.
Netherton SJ, Lonergan K, Wang D, McRae A, Lang E. Computerized physician order entry and decision support improves ED analgesic ordering for renal colic. Am J Emerg Med. 2014;32(9):958-61. [PubMed ID: 24997107]. https://doi.org/10.1016/j.ajem.2014.05.002.
-
48.
Caraballo PJ, Naessens JM, Klarich MJ, Leutink DJ, Peterson JA, Wagie AE, et al. Decline in ACEI/ARB Prescribing as Heart Failure Core Metrics Improve During Computer-Based Clinical Decision Support. Am J Med Qual. 2014;29(4):300-7. [PubMed ID: 24249835]. https://doi.org/10.1177/1062860613509265.
-
49.
Kohler MJ, Amezaga M, Drozd J, Crowley ST, Gulanski B, Anderson DR, et al. Use of a computerized order set to increase prescription of calcium and vitamin D supplementation in patients receiving glucocorticoids. J Gen Intern Med. 2013;28(6):825-9. [PubMed ID: 23404201]. [PubMed Central ID: PMC3663954]. https://doi.org/10.1007/s11606-013-2360-1.
-
50.
Awdishu L, Coates CR, Lyddane A, Tran K, Daniels CE, Lee J, et al. The impact of real-time alerting on appropriate prescribing in kidney disease: a cluster randomized controlled trial. J Am Med Inform Assoc. 2016;23(3):609-16. [PubMed ID: 26615182]. https://doi.org/10.1093/jamia/ocv159.
-
51.
Claus BO, Colpaert K, Steurbaut K, De Turck F, Vogelaers DP, Robays H, et al. Role of an electronic antimicrobial alert system in intensive care in dosing errors and pharmacist workload. Int J Clin Pharm. 2015;37(2):387-94. [PubMed ID: 25666942]. https://doi.org/10.1007/s11096-015-0075-6.
-
52.
Coleman JJ, Hodson J, Thomas SK, Brooks HL, Ferner RE. Temporal and other factors that influence the time doctors take to prescribe using an electronic prescribing system. J Am Med Inform Assoc. 2015;22(1):206-12. [PubMed ID: 25074989]. [PubMed Central ID: PMC4433371]. https://doi.org/10.1136/amiajnl-2014-002822.
-
53.
Yu CH, Stephenson AL, Gupta S. The effect of patient care order sets on medical resident education: a prospective before-after study. BMC Med Educ. 2013;13:146. [PubMed ID: 24195667]. [PubMed Central ID: PMC3829666]. https://doi.org/10.1186/1472-6920-13-146.
-
54.
Thomas SK, Coleman JJ. The impact of computerised physician order entry with integrated clinical decision support on pharmacist–physician communication in the hospital setting: a systematic review of the literature. Eur J Hosp Pharm. 2012;19(4):349-54. https://doi.org/10.1136/ejhpharm-2012-000110.
-
55.
Wright A, Aaron S, Seger DL, Samal L, Schiff GD, Bates DW. Reduced Effectiveness of Interruptive Drug-Drug Interaction Alerts after Conversion to a Commercial Electronic Health Record. J Gen Intern Med. 2018;33(11):1868-76. [PubMed ID: 29766382]. [PubMed Central ID: PMC6206354]. https://doi.org/10.1007/s11606-018-4415-9.
-
56.
Tseng CW, Lin GA, Davis J, Taira DA, Yazdany J, He Q, et al. Giving formulary and drug cost information to providers and impact on medication cost and use: a longitudinal non-randomized study. BMC Health Serv Res. 2016;16(1):499. [PubMed ID: 27654857]. [PubMed Central ID: PMC5031286]. https://doi.org/10.1186/s12913-016-1752-4.
-
57.
McGregor JC, Weekes E, Forrest GN, Standiford HC, Perencevich EN, Furuno JP, et al. Impact of a computerized clinical decision support system on reducing inappropriate antimicrobial use: a randomized controlled trial. J Am Med Inform Assoc. 2006;13(4):378-84. [PubMed ID: 16622162]. [PubMed Central ID: PMC1513678]. https://doi.org/10.1197/jamia.M2049.
-
58.
Okumura LM, Veroneze I, Burgardt CI, Fragoso MF. Effects of a computerized provider order entry and a clinical decision support system to improve cefazolin use in surgical prophylaxis: a cost saving analysis. Pharm Pract (Granada). 2016;14(3):717. [PubMed ID: 27785159]. [PubMed Central ID: PMC5061515]. https://doi.org/10.18549/PharmPract.2016.03.717.
-
59.
Weingart SN, Zhu J, Young-Hong J, Vermilya HB, Hassett M. Do drug interaction alerts between a chemotherapy order-entry system and an electronic medical record affect clinician behavior? J Oncol Pharm Pract. 2014;20(3):163-71. [PubMed ID: 23804625]. https://doi.org/10.1177/1078155213487395.
-
60.
Dexheimer JW, Kirkendall ES, Kouril M, Hagedorn PA, Minich T, Duan LL, et al. The Effects of Medication Alerts on Prescriber Response in a Pediatric Hospital. Appl Clin Inform. 2017;8(2):491-501. [PubMed ID: 28487930]. [PubMed Central ID: PMC6241745]. https://doi.org/10.4338/ACI-2016-10-RA-0168.
-
61.
Page N, Baysari MT, Westbrook JI. A systematic review of the effectiveness of interruptive medication prescribing alerts in hospital CPOE systems to change prescriber behavior and improve patient safety. Int J Med Inform. 2017;105:22-30. [PubMed ID: 28750908]. https://doi.org/10.1016/j.ijmedinf.2017.05.011.
-
62.
Wong A, Amato MG, Seger DL, Rehr C, Wright A, Slight SP, et al. Prospective evaluation of medication-related clinical decision support over-rides in the intensive care unit. BMJ Qual Saf. 2018;27(9):718-24. [PubMed ID: 29440481]. https://doi.org/10.1136/bmjqs-2017-007531.
-
63.
Balasuriya L, Vyles D, Bakerman P, Holton V, Vaidya V, Garcia-Filion P, et al. Computerized Dose Range Checking Using Hard and Soft Stop Alerts Reduces Prescribing Errors in a Pediatric Intensive Care Unit. J Patient Saf. 2017;13(3):144-8. [PubMed ID: 25370855]. https://doi.org/10.1097/PTS.0000000000000132.
-
64.
Fargo EL, D'Amico F, Pickering A, Fowler K, Campbell R, Baumgartner M. Impact of Electronic Physician Order-Set on Antibiotic Ordering Time in Septic Patients in the Emergency Department. Appl Clin Inform. 2018;9(4):869-74. [PubMed ID: 30517970]. [PubMed Central ID: PMC6281440]. https://doi.org/10.1055/s-0038-1676040.
-
65.
Huber TC, Krishnaraj A, Patrie J, Gaskin CM. Impact of a Commercially Available Clinical Decision Support Program on Provider Ordering Habits. J Am Coll Radiol. 2018;15(7):951-7. [PubMed ID: 29807818]. https://doi.org/10.1016/j.jacr.2018.03.045.
-
66.
Min A, Chan VWY, Aristizabal R, Peramaki ER, Agulnik DB, Strydom N, et al. Clinical Decision Support Decreases Volume of Imaging for Low Back Pain in an Urban Emergency Department. J Am Coll Radiol. 2017;14(7):889-99. [PubMed ID: 28483544]. https://doi.org/10.1016/j.jacr.2017.03.005.
-
67.
Sistrom CL, Weilburg JB, Dreyer KJ, Ferris TG. Provider Feedback about Imaging Appropriateness by Using Scores from Order Entry Decision Support: Raw Rates Misclassify Outliers. Radiology. 2015;275(2):469-79. [PubMed ID: 25423147]. https://doi.org/10.1148/radiol.14141092.
-
68.
Schneider E, Zelenka S, Grooff P, Alexa D, Bullen J, Obuchowski NA. Radiology order decision support: examination-indication appropriateness assessed using 2 electronic systems. J Am Coll Radiol. 2015;12(4):349-57. [PubMed ID: 25842015]. https://doi.org/10.1016/j.jacr.2014.12.005.
-
69.
Moriarity AK, Klochko C, O'Brien M, Halabi S. The effect of clinical decision support for advanced inpatient imaging. J Am Coll Radiol. 2015;12(4):358-63. [PubMed ID: 25622766]. https://doi.org/10.1016/j.jacr.2014.11.013.
-
70.
Goldzweig CL, Orshansky G, Paige NM, Miake-Lye IM, Beroes JM, Ewing BA, et al. Electronic health record-based interventions for improving appropriate diagnostic imaging: A systematic review and meta-analysis. Ann Intern Med. 2015;162(8):557-65. [PubMed ID: 25894025]. https://doi.org/10.7326/M14-2600.
-
71.
Thrall JH. Appropriateness and imaging utilization: "computerized provider order entry and decision support". Acad Radiol. 2014;21(9):1083-7. [PubMed ID: 25107862]. https://doi.org/10.1016/j.acra.2014.02.019.
-
72.
Britton DJ, Bloch RB, Strout TD, Baumann MR. Impact of a computerized order set on adherence to Centers for Disease Control guidelines for the treatment of victims of sexual assault. J Emerg Med. 2013;44(2):528-35. [PubMed ID: 22921854]. https://doi.org/10.1016/j.jemermed.2012.06.016.
-
73.
Durand DJ, Feldman LS, Lewin JS, Brotman DJ. Provider cost transparency alone has no impact on inpatient imaging utilization. J Am Coll Radiol. 2013;10(2):108-13. [PubMed ID: 23273974]. https://doi.org/10.1016/j.jacr.2012.06.020.
-
74.
Yang MS, Choi SI, Song WJ, Kim SH, Cho SH, Min KU, et al. Electronic Consultation Support System for Radiocontrast Media Hypersensitivity Changes Clinicians' Behavior. Allergy Asthma Immunol Res. 2018;10(2):165-71. [PubMed ID: 29411557]. [PubMed Central ID: PMC5809765]. https://doi.org/10.4168/aair.2018.10.2.165.
-
75.
Schneider E, Ruggieri P, Fromwiller L, Underwood R, Gurland B, Yurkschatt C, et al. An electronic safety screening process during inpatient computerized physician order entry improves the efficiency of magnetic resonance imaging exams. Acad Radiol. 2013;20(12):1592-7. [PubMed ID: 24200487]. https://doi.org/10.1016/j.acra.2013.09.006.
-
76.
Wasser EJ, Prevedello LM, Sodickson A, Mar W, Khorasani R. Impact of a real-time computerized duplicate alert system on the utilization of computed tomography. JAMA Intern Med. 2013;173(11):1024-6. [PubMed ID: 23609029]. [PubMed Central ID: PMC4445932]. https://doi.org/10.1001/jamainternmed.2013.543.
-
77.
Rubinstein M, Hirsch R, Bandyopadhyay K, Madison B, Taylor T, Ranne A, et al. Effectiveness of Practices to Support Appropriate Laboratory Test Utilization: A Laboratory Medicine Best Practices Systematic Review and Meta-Analysis. Am J Clin Pathol. 2018;149(3):197-221. [PubMed ID: 29471324]. [PubMed Central ID: PMC6016712]. https://doi.org/10.1093/ajcp/aqx147.
-
78.
Eaton KP, Chida N, Apfel A, Feldman L, Greenbaum A, Tuddenham S, et al. Impact of nonintrusive clinical decision support systems on laboratory test utilization in a large academic centre. J Eval Clin Pract. 2018;24(3):474-9. [PubMed ID: 29446193]. [PubMed Central ID: PMC6050580]. https://doi.org/10.1111/jep.12890.
-
79.
Bellodi E, Vagnoni E, Bonvento B, Lamma E. Economic and organizational impact of a clinical decision support system on laboratory test ordering. BMC Med Inform Decis Mak. 2017;17(1):179. [PubMed ID: 29273037]. [PubMed Central ID: PMC5741908]. https://doi.org/10.1186/s12911-017-0574-6.
-
80.
Algaze CA, Wood M, Pageler NM, Sharek PJ, Longhurst CA, Shin AY. Use of a Checklist and Clinical Decision Support Tool Reduces Laboratory Use and Improves Cost. Pediatrics. 2016;137(1). [PubMed ID: 26681782]. https://doi.org/10.1542/peds.2014-3019.
-
81.
Levick DL, Stern G, Meyerhoefer CD, Levick A, Pucklavage D. "Reducing unnecessary testing in a CPOE system through implementation of a targeted CDS intervention". BMC Med Inform Decis Mak. 2013;13:43. [PubMed ID: 23566021]. [PubMed Central ID: PMC3629995]. https://doi.org/10.1186/1472-6947-13-43.
-
82.
MacMillan TE, Gudgeon P, Yip PM, Cavalcanti RB. Reduction in Unnecessary Red Blood Cell Folate Testing by Restricting Computerized Physician Order Entry in the Electronic Health Record. Am J Med. 2018;131(8):939-44. [PubMed ID: 29729235]. https://doi.org/10.1016/j.amjmed.2018.03.044.
-
83.
Roshanov PS, You JJ, Dhaliwal J, Koff D, Mackay JA, Weise-Kelly L, et al. Can computerized clinical decision support systems improve practitioners' diagnostic test ordering behavior? A decision-maker-researcher partnership systematic review. Implement Sci. 2011;6:88. [PubMed ID: 21824382]. [PubMed Central ID: PMC3174115]. https://doi.org/10.1186/1748-5908-6-88.
-
84.
Procop GW, Keating C, Stagno P, Kottke-Marchant K, Partin M, Tuttle R, et al. Reducing duplicate testing: a comparison of two clinical decision support tools. Am J Clin Pathol. 2015;143(5):623-6. [PubMed ID: 25873494]. https://doi.org/10.1309/AJCPJOJ3HKEBD3TU.
-
85.
Otto CC, Shuptar SL, Milord P, Essick CJ, Nevrekar R, Granovsky SL, et al. Reducing Unnecessary and Duplicate Ordering for Ovum and Parasite Examinations and Clostridium difficile PCR in Immunocompromised Patients by Using an Alert at the Time of Request in the Order Management System. J Clin Microbiol. 2015;53(8):2745-8. [PubMed ID: 26063860]. [PubMed Central ID: PMC4508420]. https://doi.org/10.1128/JCM.00968-15.
-
86.
Georgiou A, Lang S, Rosenfeld D, Westbrook JI. The use of computerized provider order entry to improve the effectiveness and efficiency of coagulation testing. Arch Pathol Lab Med. 2011;135(4):495-8. [PubMed ID: 21466368]. https://doi.org/10.1043/2010-0286-SO.1.
-
87.
Jenkins I, Doucet JJ, Clay B, Kopko P, Fipps D, Hemmen E, et al. Transfusing Wisely: Clinical Decision Support Improves Blood Transfusion Practices. Jt Comm J Qual Patient Saf. 2017;43(8):389-95. [PubMed ID: 28738984]. https://doi.org/10.1016/j.jcjq.2017.04.003.
-
88.
McKinney ZJ, Peters JM, Gorlin JB, Perry EH. Improving red blood cell orders, utilization, and management with point-of-care clinical decision support. Transfusion. 2015;55(9):2086-94. [PubMed ID: 25857393]. https://doi.org/10.1111/trf.13103.
-
89.
Hibbs SP, Nielsen ND, Brunskill S, Doree C, Yazer MH, Kaufman RM, et al. The impact of electronic decision support on transfusion practice: A systematic review. Transfus Med Rev. 2015;29(1):14-23. [PubMed ID: 25535095]. https://doi.org/10.1016/j.tmrv.2014.10.002.
-
90.
Goodnough LT, Shah N. Is there a "magic" hemoglobin number? Clinical decision support promoting restrictive blood transfusion practices. Am J Hematol. 2015;90(10):927-33. [PubMed ID: 26113442]. https://doi.org/10.1002/ajh.24101.
-
91.
Yerrabothala S, Desrosiers KP, Szczepiorkowski ZM, Dunbar NM. Significant reduction in red blood cell transfusions in a general hospital after successful implementation of a restrictive transfusion policy supported by prospective computerized order auditing. Transfusion. 2014;54(10 Pt 2):2640-5. [PubMed ID: 24673396]. https://doi.org/10.1111/trf.12627.
-
92.
Goodnough LT, Shieh L, Hadhazy E, Cheng N, Khari P, Maggio P. Improved blood utilization using real-time clinical decision support. Transfusion. 2014;54(5):1358-65. [PubMed ID: 24117533]. https://doi.org/10.1111/trf.12445.
-
93.
Smith M, Triulzi DJ, Yazer MH, Rollins-Raval MA, Waters JH, Raval JS. Implementation of a simple electronic transfusion alert system decreases inappropriate ordering of packed red blood cells and plasma in a multi-hospital health care system. Transfus Apher Sci. 2014;51(3):53-8. [PubMed ID: 25458903]. https://doi.org/10.1016/j.transci.2014.10.022.
-
94.
Yazer MH, Triulzi DJ, Reddy V, Waters JH. Effectiveness of a real-time clinical decision support system for computerized physician order entry of plasma orders. Transfusion. 2013;53(12):3120-7. [PubMed ID: 23627673]. https://doi.org/10.1111/trf.12228.
-
95.
Butler CE, Noel S, Hibbs SP, Miles D, Staves J, Mohaghegh P, et al. Implementation of a clinical decision support system improves compliance with restrictive transfusion policies in hematology patients. Transfusion. 2015;55(8):1964-71. [PubMed ID: 25906831]. https://doi.org/10.1111/trf.13075.
-
96.
Fernandez Perez ER, Winters JL, Gajic O. The addition of decision support into computerized physician order entry reduces red blood cell transfusion resource utilization in the intensive care unit. Am J Hematol. 2007;82(7):631-3. [PubMed ID: 17236185]. https://doi.org/10.1002/ajh.20888.
-
97.
Schiff GD, Amato MG, Eguale T, Boehne JJ, Wright A, Koppel R, et al. Computerised physician order entry-related medication errors: analysis of reported errors and vulnerability testing of current systems. BMJ Qual Saf. 2015;24(4):264-71. [PubMed ID: 25595599]. [PubMed Central ID: PMC4392214]. https://doi.org/10.1136/bmjqs-2014-003555.
-
98.
Gurwitz JH, Field TS, Rochon P, Judge J, Harrold LR, Bell CM, et al. Effect of computerized provider order entry with clinical decision support on adverse drug events in the long-term care setting. J Am Geriatr Soc. 2008;56(12):2225-33. [PubMed ID: 19093922]. https://doi.org/10.1111/j.1532-5415.2008.02004.x.
-
99.
Fischer MA, Vogeli C, Stedman M, Ferris T, Brookhart MA, Weissman JS. Effect of electronic prescribing with formulary decision support on medication use and cost. Arch Intern Med. 2008;168(22):2433-9. [PubMed ID: 19064827]. https://doi.org/10.1001/archinte.168.22.2433.
-
100.
McCoy AB, Waitman LR, Lewis JB, Wright JA, Choma DP, Miller RA, et al. A framework for evaluating the appropriateness of clinical decision support alerts and responses. J Am Med Inform Assoc. 2012;19(3):346-52. [PubMed ID: 21849334]. [PubMed Central ID: PMC3341775]. https://doi.org/10.1136/amiajnl-2011-000185.