Abstract
Background:
This study sought to determine the anatomical variations of the mental foramen (MF) and the mandibular canal (MC) in the full edentulous Iranian subpopulation using cone-beam computed tomography (CBCT). These variations can have significant clinical implications in dental implant surgery.Methods:
This descriptive cross-sectional study evaluated the mandible CBCT scans of 384 completely edentulous patients that required dental implant treatment. The CBCT scans were retrieved from four radiology clinics in Tehran, Iran, using quota sampling. The reconstructed images were evaluated to determine the dimensions and position of the MC and its cortication at the site of the mandibular first molar, the branching of the MC, the existence of the anterior loop of the mental nerve, and anatomical variations of the MF. The correlations of variables with age and gender were analyzed using the independent t-test, chi-square test, and analysis of variance based on the type of the variable.Results:
The cortication of the MC at the site of the mandibular first molar was present in 72.9% of the cases and was significantly more common in male patients (P = 0.0001). Bifid mandibular canal, accessory MF, and anterior loop of mental nerve were present in 9.9%, 65%, and 54.7% of the samples, respectively, and they had no significant correlation with age/gender. The mean MC diameter, the mean MF height, and the mean distance from the inferior border of the mandible to the center of MF were all significantly higher in male patients (P < 0.05). The mean distance between the MC and the buccal and lingual cortical plates had no correlation with age/gender. The mean height between the superior part of the MC and the alveolar crest was significantly lower in female patients and those within the age range of 71 - 95 years (P < 0.05). The MC opened in the MF superiorly in 40.1% of the patients with no significant correlation with age/gender.Conclusions:
Anatomical variations in the course and location of the MC and MF necessitate the precise assessment of the edentulous ridge by CBCT prior to the placement of implants.Keywords
Cone-Beam Computed Tomography Mandibular Canal Mental Foramen Dental Implants Anterior Loop of Mental Nerve
1. Background
The mandibular canal (MC) is an anatomical structure in the mandible that extends from the mandibular foramen in the ramus to the mental foramen (MF). The MC contains the inferior alveolar nerve and vascular bundle, comprising the inferior alveolar artery, vein, nerve, and lymphatic vessels (1, 2). The MC is usually a single canal, bilaterally present in the mandible in a symmetrical fashion. There might be some varieties regarding the position of the MC relative to the inferior border of the mandible and tooth apex. Therefore, the MC cannot serve as a reference point for prosthodontic or orthodontic diagnosis or treatment planning (3).
As a result of the abnormal interaction of tissues during embryonic dental development, the morphological alterations of the MC occur. It has been determined that at the time of embryonic maturation, there are three inferior dental nerves that fuse to make a single nerve; therefore, the bifid and trifid MCs manage to exist as a result of the inconclusive fusion of these three nerves (2). The developmental ossification of the mandible starts at the area of the MF and continues posteriorly, creating the MC around the neurovascular bundle. This process clarifies the diversity of MCs (4).
Determining the position of the MC, the MF, the incisive canal, and the anterior loop of the mental nerve is highly important in oral surgeries, particularly dental implant placement. Conventionally, periapical and panoramic radiographs are often used for this purpose, which have some limitations due to their two-dimensional nature. Therefore, newer imaging modalities, such as magnetic resonance imaging, computed tomography (CT), and cone-beam computed tomography (CBCT), might be used for clinical or research purposes (2).
Dental implant surgery is a minor maxillofacial surgical procedure that is unlike any prosthodontic or conservative dental treatments. It is essential to become familiar with the nerves and vessels in the maxilla and mandible areas. Anatomical variations can cause several clinical problems in patients. Therefore, they need to be precisely evaluated prior to surgical procedures, particularly dental implant placement (5). Failure in the correct determination of the anatomical position and course of the MC can lead to bleeding and trauma or several postoperative complications, such as pain or paresthesia. Damage to critical structures in the MC often occurs due to surgical procedural errors by the clinicians or failure in the correct detection of the canal course, or morphological variations in this structure. Therefore, it is critical to determine the exact location and course of the MC and related anatomical structures to keep the risk of injury to a minimum (2).
Mandibular anatomy and progressive alveolar bone resorption following tooth loss have been previously studied. However, the anatomical variations of the MC after bone resorption have not been well investigated. Regarding the position of the MC in a resorbed mandible, the distance between the MC and the buccal and lingual cortical plates often remains constant during the process of bone resorption; nevertheless, the space between the MC and the inferior and superior mandibular borders might change. The greatest change occurs in the distance between the MC and the superior border. Some systemic conditions and intake of some medications increase the resorption of canal walls. In cases of severe resorption, the superior border of the MC and its contents might remain exposed under the mucosa. In such cases, the canal wall is mainly composed of cancellous bone with occasional trabeculae. The canal contents pass through the bone marrow space and are positioned right beneath the lingual cortex (1).
The anatomical variations of the MC, such as the bifid mandibular canal (BMC), can cause several clinical complications for patients. For the prevention of damage to the neurovascular contents of the canal (e.g., hemorrhage and sensory disorders) in different surgical procedures, such as surgical extraction of third molars, implant placement, and orthognathic surgery, it is imperative to gain adequate knowledge about the course and position of the MC in ramus and body of mandible (1). Failure of inferior alveolar nerve block injection is another complication related to the anatomical variations of the MC, such as the presence of a BMC and an additional MF. When the soft tissue around the injection site is anesthetized, but the corner of the mouth on the same side is not anesthetized, the block injection has probably failed. One possibility can be the presence of an additional branch of the MC (2).
2. Objectives
With this background in mind, this study tried to show the anatomical variations of edentulous atrophic mandibles using CBCT.
3. Methods
This descriptive cross-sectional study evaluated the CBCT scans of the Iranian subpopulation with edentulous mandibles. The CBCT scans were retrieved from four oral and maxillofacial radiology clinics in Tehran, Iran, including the School of Dentistry of Shahid Beheshti University of Medical Sciences, within 2015 - 2016 using quota sampling. The number of selected CBCT scans from each center depended on the total number of CBCT scans in the respective center. The list of CBCT scans of each center was obtained, and the eligible CBCT scans were randomly selected from the list. Since both qualitative and quantitative variables were evaluated in this study, the sample size was calculated to be 384 using the sample size calculation formula for the estimation of the mean and the sample size calculation formula for the estimation of the ratio, assuming the standard deviation of the width of the MF to be 0.8, alpha = 0.05, and d = 0.08.
The inclusion criteria were the good-quality CBCT scans of the edentulous mandible of patients requiring implant placement, irrespective of their gender. The CBCT scans of patients with mandibular pathologies or trauma to the mandible and those with severe ridge resorption such that the alveolar crest was no longer present over the canal were excluded.
A total of 384 CBCT scans (384 hemi-mandibles) of patients with a completely edentulous mandible who required implant placement in the mandible were collected. The CBCT scans were taken with the NewTom VGi CBCT system (Verona, Italy) under standard conditions with the exposure setting of 110 kVp, 200 µ voxel size, and 8 × 8-cm field of view in two centers, NewTom GIANO (Verona, Italy) with the exposure settings of 90 kVp, 200 µ voxel size, and 11 × 9-cm field of view in one center, and Scanora 3D (Soredex, Helsinki, Finland) with the exposure settings of 90 kVp, 200 µ voxel size, and 7.5 × 10-cm field of view in another center with 1 mm slice intervals for cross-sectional images. For the observation and reconstruction of the images retrieved from different radiology centers, the images in the Digital Imaging and Communications in Medicine format were imported into OnDemand 3D software (version 1.0.9). The axial, sagittal, cross-sectional, and panoramic images were reconstructed. The images were displayed on a 20-inch Philips monitor with 1024-1280-pixel resolution.
The approximate location of the mandibular first molar in the edentulous mandible was calculated to be at 37 mm distance from the midline, considering the total standard width of the teeth. Therefore, the MC measurements were made at a 37 mm distance from the midline on an arc drawn on the axial view of the middle section of the mandibular ridge.
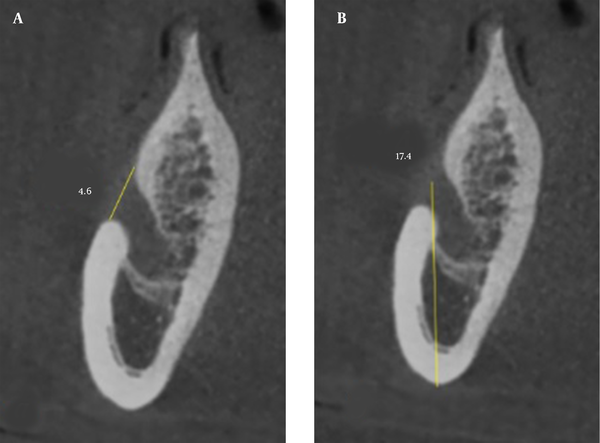
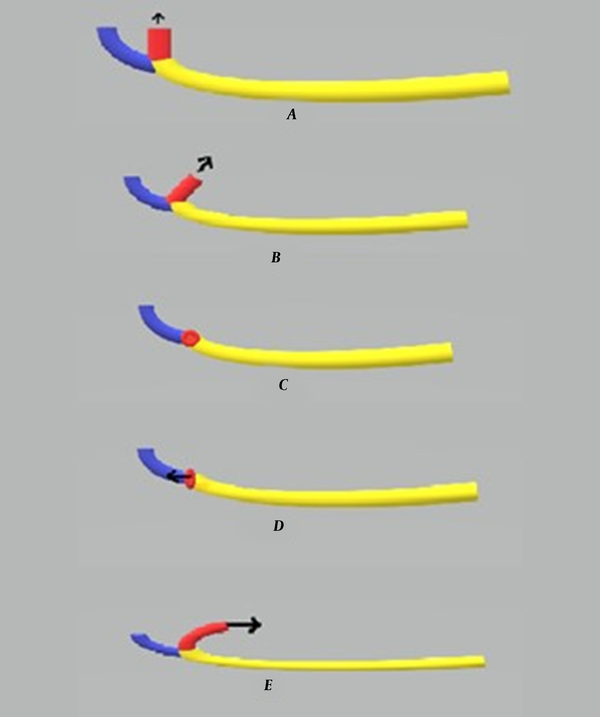
The data were collected by the observation of the reconstructed CBCT images and included the MC dimensions (Figure 1), MC cortication, buccolingual position of the MC (Figure 1), number of branches of the MC, anatomical variations of the MF (Figure 2), anterior loop of the mental nerve, and correlation of the aforementioned parameters with the age and gender of patients. All the variables were evaluated on the cross-sectional images except for the presence of accessory MF and the pattern of the opening of the MC in the MF (Figure 3) that were evaluated on three-dimensional images. All the CBCT scans were assessed in the daytime by one calibrated oral and maxillofacial radiologist. At the end of data collection, 10% of the samples were re-examined 2 weeks later by the same oral and maxillofacial radiologist with an intra-observer agreement of 1. The measured values were recorded in a checklist.
Mandibular canal (MC) variations; (A) Mean diameter of the MC; (B) Mean distance from the center of the MC to the lingual cortical plate; (C) Mean distance from the center of the MC to the buccal cortical plate; (D) Mean distance between the superior part of the MC and the alveolar crest
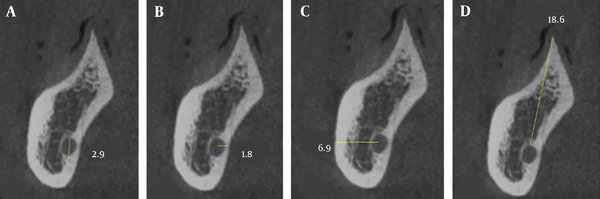
Mental foramen (MF) variations; (A) Mean height of the MF; (B) Vertical position of the MF
Pattern of opening of the mandibular canal in the mental foramen (A) Superiorly, (B) Superiorly-posteriorly, (C) Labially, (D) Anteriorly, and (E) Posteriorly.
The findings were analyzed using SPSS software (version 21; SPSS Inc., IL, USA). The normal distribution of the data was evaluated using the Shapiro-Wilk test. Normally distributed data were analyzed by the chi-square test, independent t-test, and analysis of variance. Non-normally distributed data were analyzed by non-parametric tests.
4. Results
Of 384 CBCT scans evaluated in this study, 180 (46.9%) and 204 (53.1%) scans were affiliated with female and male subjects, respectively. The mean age of the patients was 59.3 ± 11.3 years. On CBCT images of the MC, 72.9% (n = 280) had a corticated wall, and 27.1% (n = 104) did not have cortication. Of all, 89.8% (n = 345), 9.9% (n = 38), and 0.3% (n = 1) had a single MC, a BMC, and a multi-branched MC. Regarding the pattern of opening of the MC in the MF, it opened superiorly, posteriorly, superiorly and posteriorly, and labially in 40.1% (n = 154), 8.6% (n = 33), 20.3% (n = 78), and 31% (n = 119). Accessory MF was noted in 6.5% (n = 25). Additionally, 54.7% (n = 210) had an anterior loop of the mental nerve.
4.1. Mean Diameter of MC
The mean diameter of the MC in male patients was significantly greater than in female patients (3.34 ± 0.92 versus 3.15 ± 0.87 mm; P = 0.048). The difference in this parameter was not significant between the age groups of 20 - 45, 46 - 70, and 71 - 95 years (P = 0.57; Table 1).
Mean Diameter of Mandibular Canal (MC), Mean Distance from the Center of the MC to the Buccal and Lingual Cortical Plates, Mean Distance Between the Alveolar Crest and the Superior Part of the MC, Mean Height of Mental Foramen (MF), and Vertical Position of the MF
| Gender | Age (y) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Female (n = 180) | Male (n = 204) | Total (n = 384) | P-Value | 20 - 45 (n = 45) | 46 - 70 (n = 275) | 71 - 95 (n = 64) | Total (n = 384) | P-Value | |
| Mean diameter of MC (mm) | 3.15 ± 0.86 | 3.34 ± 0.91 | 3.25 ± 0.9 | 0.048 | 3.17 ± 0.81 | 3.28 ± 0.88 | 3.18 ± 1 | 3.25 ± 0.9 | 0.57 |
| Mean distance from the center of MC to the buccal cortical plate (mm) | 6.04 ± 1.28 | 6.09 ± 1.49 | 6.07 ± 1.39 | 0.7 | 5.97 ± 1.27 | 6.11 ± 1.49 | 5.93 ± 1.18 | 6.07 ± 1.39 | 0.57 |
| Mean distance from the center of MC to the lingual cortical plate (mm) | 3.66 ± 1.19 | 3.67 ± 1.25 | 3.67 ± 1.22 | 0.9 | 3.57 ± 1.01 | 3.65 ± 1.26 | 3.78 ± 1.2 | 3.67 ± 1.22 | 0.6 |
| Mean distance between the alveolar crest and the superior part of MC (mm) | 7.16 ± 4.46 | 9.01 ± 4.87 | 8.15 ± 4.77 | 0.001 | 8.07 ± 4.86 | 8.6 ± 4.67 | 6.26 ± 4.71 | 8.15 ± 4.77 | 0.002 |
| Mean height of MF (mm) | 2.64 ± 0.92 | 2.98 ± 1.01 | 2.82 ± 0.98 | 0.001 | 2.92 ± 1.1 | 2.83 ± 0.97 | 2.73 ± 0.93 | 2.82 ± 0.98 | 0.59 |
| Vertical position of MF (mm) | 12.78 ± 2.45 | 13.89 ± 2.05 | 13.37 ± 2.31 | 0.001 | 13.35 ± 2.01 | 13.47 ± 2.28 | 12.96 ± 2.63 | 13.37 ± 2.31 | 0.59 |
4.2. Mean Height of MF
The mean height of the MF in male patients was significantly greater than in female patients (2.98 ± 1.01 versus 2.64 ± 0.92 mm; P = 0.001). The difference in this parameter was not significant between different age groups (P = 0.59; Table 1).
4.3. Mean Distance from Center of MF to Inferior Border of the Mandible (i.e., Vertical Position of MF)
The mean distance from the inferior border of the mandible to the MF in male patients was significantly greater than in female patients (13.89 ± 2.05 versus 12.78 ± 2.45 mm; P = 0.001). The difference in this parameter was not significant between different age groups (P = 0.59; Table 1).
4.4. Mean Distance from Center of MC to Lingual Cortical Plate
The mean distances from the lingual cortical plate to the center of the MC were 3.67 ± 1.25 and 3.66 ± 1.19 mm in male and female patients, respectively, with no significant difference (P = 0.9). The difference in this parameter was not significant between different age groups (P = 0.6; Table 1).
4.5. Mean Distance from Center of MC to Buccal Cortical Plate
The mean distances from the buccal cortical plate to the center of the MC were 6.09 ± 1.49 and 6.04 ± 1.28 mm in male and female patients, respectively, with no significant difference (P = 0.7). The difference in this parameter was not significant between different age groups (P = 0.57; Table 1).
4.6. Mean Distance Between Superior Part of MC and Alveolar Crest
The mean height between the alveolar crest and the superior part of the MC was 9.01 ± 4.87 mm in male patients, which was significantly higher than in female patients (7.16 ± 4.46 mm) (P = 0.001). In addition, a significant difference was noted in this regard between different age groups (P = 0.002; Table 1). The least significant difference post-hoc test showed that the differences between the age ranges of 20 - 45 and 71 - 95 years (P = 0.049) and the differences between the age ranges of 46 - 70 and 71 - 95 years (P = 0.001) were significant.
4.7. Cortication, Branching, and Pattern of Opening of Mandibular Canal
The Chi-square test showed that gender had a significant correlation with the cortication of the MC wall (P = 0.001) since cortication was present in 63.9% (n = 115) and 80.9% (n = 165) of female and male patients, respectively. Cortication had no significant correlation with age (P = 0.44; Table 2). The type of the MC (i.e., the number of branches) had no significant correlation with gender (P = 0.26) or age (P = 0.36) (Table 3). The pattern of the opening of the MC in the MF had no significant correlation with gender (P = 0.09) or age (P = 0.1) (Table 4).
Cortication of Mandibular Canal, Presence of Accessory Mental Foramen, and Presence of Anterior Loop of Mental Nerve a
| Cortication of Mandibular Canal | Presence of Accessory Mental Foramen | Presence of Anterior Loop of Mental Nerve | |
|---|---|---|---|
| Gender | |||
| Female | 115 (63.9) | 8 (4.5) | 90 (49.7) |
| Male | 165 (80.9) | 17 (8.3) | 120 (58.8) |
| Total | 280 (72.9) | 25 (6.5) | 210 (54.7) |
| P-value | 0.0001 | 0.14 | 0.1 |
| Age (y) | |||
| 20 - 45 | 35 (77.8) | 2 (4.4) | 28 (62.2) |
| 46 - 70 | 202 (73.5) | 16 (5.8) | 152 (55.3) |
| 71 - 95 | 43 (67.2) | 7 (10.9) | 30 (46.9) |
| Total | 280 (72.9) | 25 (6.5) | 210 (54.7) |
| P-value | 0.44 | 0.27 | 0.26 |
| Type of Mandibular Canal | Single Branch | Bifid Mandibular Canal | Multiple Branches | P-Value |
|---|---|---|---|---|
| Gender | 0.26 | |||
| Female | 166 (92.2) | 14 (7.8) | 0 (0) | |
| Male | 179 (87.7) | 24 (11.8) | 1 (0.5) | |
| Total | 345 (89.8) | 38 (9.9) | 1 (0.3) | |
| Age (y) | 0.36 | |||
| 20 - 45 | 43 (95.6) | 2 (4.4) | 0 (0) | |
| 46 - 70 | 248 (90.2) | 26 (9.5) | 1 (0.4) | |
| 71 - 95 | 54 (84.4) | 10 (15.6) | 0 (0) | |
| Total | 345 (89.8) | 38 (9.9) | 1 (0.3) |
| Pattern of the Opening of the Mandibular Canal | Superiorly | Posteriorly | Superiorly-Posteriorly | Labially | P-Value |
|---|---|---|---|---|---|
| Gender | 0.09 | ||||
| Female | 67 (37.2) | 14 (6.8) | 32 (17.8) | 67 (37.2) | |
| Male | 87 (42.6) | 19 (9.3) | 46 (22.5) | 52 (25.5) | |
| Total | 154 (40.1) | 33 (8.6) | 78 (20.3) | 119 (31) | |
| Age (y) | 0.1 | ||||
| 20 - 45 | 18 (40) | 2 (4.4) | 14 (31.1) | 11 (24.4) | |
| 46 - 70 | 116 (42.2) | 27 (9.8) | 51 (18.5) | 81 (29.5) | |
| 71 - 95 | 20 (31.3) | 4 (6.3) | 13 (20.3) | 27 (42.2) | |
| Total | 154 (40.1) | 33 (8.6) | 78 (20.3) | 119 (31) |
4.8. Presence of Accessory Mental Foramen and Anterior Loop of Mental Nerve
The presence of accessory MF had no significant correlation with gender (P = 0.14) or age (P = 0.27). The presence of the anterior loop of the mental nerve had no significant correlation with gender (P = 0.1) or age (P = 0.26) (Table 2).
5. Discussion
This study assessed the anatomical variations of edentulous atrophic mandibles using CBCT. The results showed that the mean diameter of the MC was significantly greater in male patients (3.34 mm) than in female patients (3.15 mm); however, the difference between the age groups was not significant. The reported MC diameter by de Oliveira-Santos et al. was within the ranges of 2.1 - 4 and 0 - 2 mm in 74% and 8% of the cases, respectively, with no significant correlation with age or gender (6). Chrcanovic et al. analyzed the inner diameter of the MC from CBCT scans at 3 mm intervals, starting at the lowest point of the mandibular foramen to 21 mm underneath it. In almost all levels, male patients demonstrated a significantly larger inner diameter of the MC than female patients, and age had no significant effect on the measurements (7). Al-Shayyab et al. studied the MC diameter and its correlation with age and gender in a Jordanian population in three regions of interest by CBCT (i.e., (A) mandibular foramen, (B) mandibular angle, and (C) mesial to the second mandibular molar). The mean diameter values of the MC in regions A, B, and C were 3 ± 0.8, 4 ± 0.8, and 3.1 ± 0.8, respectively, and significantly higher in males than in females (P < 0.001). In contrast to the present study, adults exhibited a significantly lower MC diameter than younger patients (8).
In this study, 72.9% of the cases had MC wall cortication, which was significantly more common in male patients (80.9% of males versus 63.9% of females) and had no correlation with age. De Oliveira-Santos et al. observed MC cortication in 59% of the hemi-mandibles with no significant correlation with age or gender (6).
In this study, 89.8% of the cases had a single MC; nevertheless, 9.9% and 0.3% of the cases had bifid canals and multi-branched canals, respectively. This parameter had no significant correlation with age or gender. Bifid or multi-branched canals have been previously reported using panoramic radiography (2, 3), CT (3), and CBCT (6). According to panoramic radiography, the frequency of this anatomical variation ranges from 0.08 to 0.95% (2, 3). However, on panoramic radiographs, the anatomy of the mylohyoid groove, which often forms a bony canal and sometimes originates from the MC, can mimic a BMC (9). However, this type of error does not occur in CBCT because the bifid form of the canal can be observed and ensured in different spatial planes. The first reports on BMC using panoramic radiography reported 1% prevalence rate for this anatomical variant (2). More recent studies reported a frequency range of 0.09 to 36%, which can be due to the differences in sample size, method of examination, and type of imaging modality since panoramic radiography underestimates the prevalence of this anatomical variation in comparison to CBCT and direct examination of the dry mandible (3, 10).
De Castro et al. assessed mandibular canal branching (MCB) with CBCT and concluded that the prevalence of MCB was 41.1%, among which 61.5% presented one branch; nevertheless, 38.5% presented more than one MCB. There was no statistically significant difference in gender regarding the presence of MCB or the pattern of presence (i.e., single branch or multiple branches) (11). Okumus and Dumlu demonstrated BMCs in 200 (40%) of the 500 subjects and in 248 of the 1000 sides (24.8%) (12). Of all the 321 patients, Zhou et al. observed 84 (26.17%) cases of BMCs and 105 (16.36%) sides of unilateral bifurcation (13). Von Arx and Bornstein reported that the frequency of BMCs per patient ranged from 9.8 to 66.5% and per mandibular side from 7.7 to 46.5%. Furthermore, gender or age is inconclusive regarding the presence of BMCs (14). The detection of BMC prior to mandibular surgeries and implant placement in this region is highly important to prevent related complications (2).
In this study, 6.5% of patients had accessory MF with no significant correlation with age or gender. The prevalence of accessory MF with a diameter of minimally 50% of the diameter of the main MF was 6% in a study by de Oliveira-Santos et al., and the prevalence of accessory MF with a diameter < 50% of the main MF was 8% in their study (6). The prevalence of accessory MF was 10% in a study by Al-Khateeb et al. on 860 panoramic radiographs of a Jordanian population (15). The reported prevalence of accessory MF was 3.2% in a study by Leite et al. (16) and 6.5% in a study by Kalender et al. (17).
Vieira et al. evaluated the CBCT scans of 480 MCs. Regarding the presence of accessory MF, a prevalence of 7.9% was observed in the evaluated hemi-mandibles. No statistically significant difference was observed between different genders and ages (18).
In this study, the mean distance from the MC to the buccal and lingual cortical plates had no significant correlation with age or gender. This distance can be used to determine the course of the MC. According to Nair et al., the MC at the site of the molars is closer to the inferior border of the mandible and the lingual cortical plate. The MC might have different anatomical shapes in the horizontal plane (19). Juodzbalys et al. reported that the MC and the inferior alveolar neurovascular bundle in the body of the mandible had an S-shaped course, and it approximated the lingual surface at the site of molars and then approximated the vestibular surface in more anterior areas (20).
Khorshidi et al. evaluated the shortest linear distances from the most lingual and buccal parts of the canal to the corresponding cortical plates of the mandible in four different regions. In most cases, the MC was located more lingual at all sites to the point it got to the MF. Nevertheless, at the MF, it was situated in close proximity to the buccal cortical plate. The distance from the MC to the buccal border of the mandible varied quite extensively from 1 to 7.7 mm. Overall, the mean bone thickness of the female group was considerably lower in horizontal distances than the male group (21).
Al-Shayyab et al. measured buccal and lingual distances from the MC to the external cortical surfaces (i.e., MC-B and MC-L, respectively) in three regions of (A) mandibular foramen, (B) mandibular angle, and (C) mesial to the second mandibular molar and compared the measurements between different age and gender groups. Adults exhibited a decrease in the average MC-L value and a growth in the average MC-B value in comparison to young patients. MC-L distances were not considerably different between male and female subjects. MC-B in areas B and C showed notably higher measurements in males than in females in adults (8). The determination of the position and course of the MC relative to the compact lateral bone plates is highly important prior to implant placement and in the selection of implant type (20).
In this study, the mean height from the alveolar crest to the superior part of the MC in male patients was significantly higher than in female patients (9.01 versus 7.16 mm). Additionally, this distance in the age range of 71 - 95 years was significantly lower than in other age groups. This value ranged from 15.3 to 17.4 mm in a study by Watanabe et al. (22). This distance is highly variable and should be individually measured for each patient.
In the current study, the mean height of the MF in male patients was significantly higher than in female patients (2.98 versus 2.64 mm), with no significant correlation with age. This value was 3.47 mm in a study by Neiva et al. on 22 Caucasian skulls (23).
In this study, the mean distance from the inferior border of the mandible to the center of the MF in male patients was significantly higher than in female patients (13.89 versus 12.78 mm), with no significant correlation with age. Neiva et al. reported this distance to be 12 mm (23). The inferior border of the mandible can be used to determine the vertical position of the MF in edentulous patients.
In this study, the prevalence of the anterior loop of the mental nerve was 54.7%, with no significant correlation with age or gender. De Oliveira-Santos et al. reported that the anterior loop with over 2 mm length had a prevalence of 22-28% (6). Preoperative assessment for the presence of the anterior loop is imperative since patients would experience a higher rate of sensory disturbances and hemorrhagic complications in case of its presence. It reportedly has a prevalence range of 28 to 62.7% (2, 24).
The pattern of the opening of the MC in the MF in the current study was superior in 40.7%, with no significant correlation with age or gender. In a study by Fabian et al., the pattern of the opening of the MC was superior in 44% and superior and posterior in 40% (25).
5.1. Limitations
One limitation of this study was the lack of information about the age of edentulism since this information was not available in patients’ records retrieved from the archives. Future multi-center studies are required to assess the anatomical variations of the mandible in different populations and ethnic groups. In addition, the results of CBCT can be compared to those of CT and panoramic radiography to determine the efficacy of each imaging modality for such assessments. Last but not least, the differences in anatomical variations should be compared between dentate and edentulous patients in future studies.
5.2. Conclusions
Considering the anatomical variations in the position of the MC, knowledge in this regard is imperative to prevent the traumatization of the inferior alveolar nerve. Therefore, CBCT is recommended prior to surgical procedures in this region to gain knowledge about the anatomical variations in each patient and apply the necessary modifications in anesthetic injection or surgical technique to achieve the best outcome with the least complications.
Acknowledgements
References
-
1.
Yaghmaei M, Mashhadiabbas F, Shahabi S, Zafarbakhsh A, Yaghmaei S, Khojasteh A. Histologic evaluation of inferior alveolar lymphatics: an anatomic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(5):564-7. [PubMed ID: 21333563]. https://doi.org/10.1016/j.tripleo.2010.11.013.
-
2.
Valenzuela-Fuenzalida JJ, Cariseo C, Gold M, Diaz D, Orellana M, Iwanaga J. Anatomical variations of the mandibular canal and their clinical implications in dental practice: a literature review. Surg Radiol Anat. 2021;43(8):1259-72. [PubMed ID: 33630105]. https://doi.org/10.1007/s00276-021-02708-7.
-
3.
Sanchis JM, Penarrocha M, Soler F. Bifid mandibular canal. J Oral Maxillofac Surg. 2003;61(4):422-4. [PubMed ID: 12684957]. https://doi.org/10.1053/joms.2003.50004.
-
4.
Ramirez KR. Presence of two mandibular canals and distinction of the inferior alveolar and mental nerves proximal to the mandible: A case study. Transl Res Anat. 2019;14:6-8. https://doi.org/10.1016/j.tria.2019.02.002.
-
5.
Kageyama I, Maeda S, Takezawa K. Importance of anatomy in dental implant surgery. J Oral Biosci. 2021;63(2):142-52. [PubMed ID: 33524607]. https://doi.org/10.1016/j.job.2021.01.002.
-
6.
de Oliveira-Santos C, Souza PH, de Azambuja Berti-Couto S, Stinkens L, Moyaert K, Rubira-Bullen IR, et al. Assessment of variations of the mandibular canal through cone beam computed tomography. Clin Oral Investig. 2012;16(2):387-93. [PubMed ID: 21448636]. https://doi.org/10.1007/s00784-011-0544-9.
-
7.
Chrcanovic BR, de Carvalho Machado V, Gjelvold B. A morphometric analysis of the mandibular canal by cone beam computed tomography and its relevance to the sagittal split ramus osteotomy. Oral Maxillofac Surg. 2016;20(2):183-90. [PubMed ID: 26875084]. https://doi.org/10.1007/s10006-016-0550-9.
-
8.
Al-Shayyab MH, Qabba'ah K, Alsoleihat F, Baqain ZH. Age and gender variations in the cone-beam computed tomographic location of mandibular canal: Implications for mandibular sagittal split osteotomy. Med Oral Patol Oral Cir Bucal. 2019;24(4):e545-54. [PubMed ID: 31232390]. [PubMed Central ID: PMC6667004]. https://doi.org/10.4317/medoral.22969.
-
9.
Kim MS, Yoon SJ, Park HW, Kang JH, Yang SY, Moon YH, et al. A false presence of bifid mandibular canals in panoramic radiographs. Dentomaxillofac Radiol. 2011;40(7):434-8. [PubMed ID: 21960401]. [PubMed Central ID: PMC3528137]. https://doi.org/10.1259/dmfr/87414410.
-
10.
Fukami K, Shiozaki K, Mishima A, Kuribayashi A, Hamada Y, Kobayashi K. Bifid mandibular canal: confirmation of limited cone beam CT findings by gross anatomical and histological investigations. Dentomaxillofac Radiol. 2012;41(6):460-5. [PubMed ID: 22116121]. [PubMed Central ID: PMC3520398]. https://doi.org/10.1259/dmfr/60245722.
-
11.
de Castro MAA, Barra SG, Vich MOL, Abreu MHG, Mesquita RA. Mandibular canal branching assessed with cone beam computed tomography. Radiol Med. 2018;123(8):601-8. [PubMed ID: 29663186]. https://doi.org/10.1007/s11547-018-0886-3.
-
12.
Okumus O, Dumlu A. Prevalence of bifid mandibular canal according to gender, type and side. J Dent Sci. 2019;14(2):126-33. [PubMed ID: 31210887]. [PubMed Central ID: PMC6562102]. https://doi.org/10.1016/j.jds.2019.03.009.
-
13.
Zhou X, Gao X, Zhang J. Bifid mandibular canals: CBCT assessment and macroscopic observation. Surg Radiol Anat. 2020;42(9):1073-9. [PubMed ID: 32399625]. https://doi.org/10.1007/s00276-020-02489-5.
-
14.
von Arx T, Bornstein MM. The bifid mandibular canal in three-dimensional radiography: morphologic and quantitative characteristics. Swiss Dent J. 2021;131(1):10-28. [PubMed ID: 33325209].
-
15.
Al-Khateeb T, Al-Hadi Hamasha A, Ababneh KT. Position of the mental foramen in a northern regional Jordanian population. Surg Radiol Anat. 2007;29(3):231-7. [PubMed ID: 17375258]. https://doi.org/10.1007/s00276-007-0199-z.
-
16.
Leite GM, Lana JP, de Carvalho Machado V, Manzi FR, Souza PE, Horta MC. Anatomic variations and lesions of the mandibular canal detected by cone beam computed tomography. Surg Radiol Anat. 2014;36(8):795-804. [PubMed ID: 24337387]. https://doi.org/10.1007/s00276-013-1247-5.
-
17.
Kalender A, Orhan K, Aksoy U. Evaluation of the mental foramen and accessory mental foramen in Turkish patients using cone-beam computed tomography images reconstructed from a volumetric rendering program. Clin Anat. 2012;25(5):584-92. [PubMed ID: 21976294]. https://doi.org/10.1002/ca.21277.
-
18.
Vieira CL, Veloso S, Lopes FF. Location of the course of the mandibular canal, anterior loop and accessory mental foramen through cone-beam computed tomography. Surg Radiol Anat. 2018;40(12):1411-7. [PubMed ID: 30120507]. https://doi.org/10.1007/s00276-018-2081-6.
-
19.
Nair UP, Yazdi MH, Nayar GM, Parry H, Katkar RA, Nair MK. Configuration of the inferior alveolar canal as detected by cone beam computed tomography. J Conserv Dent. 2013;16(6):518-21. [PubMed ID: 24347885]. [PubMed Central ID: PMC3842719]. https://doi.org/10.4103/0972-0707.120964.
-
20.
Juodzbalys G, Wang HL, Sabalys G. Anatomy of Mandibular Vital Structures. Part II: Mandibular Incisive Canal, Mental Foramen and Associated Neurovascular Bundles in Relation with Dental Implantology. J Oral Maxillofac Res. 2010;1(1). e3. [PubMed ID: 24421959]. [PubMed Central ID: PMC3886037]. https://doi.org/10.5037/jomr.2010.1103.
-
21.
Khorshidi H, Raoofi S, Ghapanchi J, Shahidi S, Paknahad M. Cone Beam Computed Tomographic Analysis of the Course and Position of Mandibular Canal. J Maxillofac Oral Surg. 2017;16(3):306-11. [PubMed ID: 28717288]. [PubMed Central ID: PMC5493549]. https://doi.org/10.1007/s12663-016-0956-9.
-
22.
Watanabe H, Mohammad Abdul M, Kurabayashi T, Aoki H. Mandible size and morphology determined with CT on a premise of dental implant operation. Surg Radiol Anat. 2010;32(4):343-9. [PubMed ID: 19812884]. https://doi.org/10.1007/s00276-009-0570-3.
-
23.
Neiva RF, Gapski R, Wang HL. Morphometric analysis of implant-related anatomy in Caucasian skulls. J Periodontol. 2004;75(8):1061-7. [PubMed ID: 15455732]. https://doi.org/10.1902/jop.2004.75.8.1061.
-
24.
Uchida Y, Noguchi N, Goto M, Yamashita Y, Hanihara T, Takamori H, et al. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve damage when installing endosseous implants in the interforaminal region: a second attempt introducing cone beam computed tomography. J Oral Maxillofac Surg. 2009;67(4):744-50. [PubMed ID: 19304029]. https://doi.org/10.1016/j.joms.2008.05.352.
-
25.
Fabian FM. Position, shape and direction of opening of the mental foramen in dry mandibles of Tanzanian adult black males. Ital J Anat Embryol. 2007;112(3):169-77. [PubMed ID: 18078238].