Abstract
Background:
Brain stroke is the main cause of death and disability worldwide. This disease can cause major complications in patients and place a great burden of care on caregivers. Therefore, this study was conducted to determine the effect of telenursing on the burden of care in caregivers and the rate of complications in patients with acute brain stroke discharged from neurological wards.Methods:
This two-arm parallel-group single-blind randomized clinical trial study was carried out on 72 patients with acute brain stroke discharged from neurological wards in Qom, Iran, in 2019. The patients and their caregivers were divided to control and intervention groups using random block allocation. In addition to the usual training of the ward, the intervention group received training and counseling based on their needs through phone calls for 4 weeks. However, the control group received only the usual ward training. Immediately after discharge from the hospital and 1 month later, the average care load in caregivers and urinary problems, bedsores, and the number of falls in patients were measured. A demographic questionnaire, Caregiver Burden Inventory, Braden Scale, Morse Scale, and a urinary problem checklist were used for data collection. The data were analyzed using the chi-square test, Mann-Whitney U test, independent t-test, and paired t-test by SPSS software (version 24).Results:
After the intervention, the mean scores of the caregiver’s burden of care in the control and counseling groups were 35.22 ± 17.215 and 8.00 ± 7.556, respectively (P < 0.001). In addition, the counseling group experienced remarkably fewer urinary problems (P < 0.001) and falling (P = 0.011).Conclusions:
This study showed that telenursing reduced the burden of care in caregivers and decreased urinary tract infections and the number of falls in patients with acute stroke. Therefore, nurses and healthcare providers can use this program to improve the lifestyle of patients with acute brain stroke and their caregivers.Keywords
Telenursing Caregiver Burden Stroke Pressure Ulcer Urinary Tract Infection Accidental Falls
1. Background
Brain stroke is the third cause of death worldwide and one of the most important diseases with long-term complications (1, 2). It is the main reason for repeated hospitalization (1). Speaking disorders, numbness in body organs, sudden vision impairment, sudden dizziness, imbalance in walking, and severe headache are among the acute symptoms of the disease (3). Moreover, it causes different levels of personal performance disorders and long-term complications (4), such as motionlessness, imbalance and falling, bedsores, swallowing and speaking disorders, defecation and urinary problems, visual impairment, injuries caused by poor oral hygiene, malnutrition, and other secondary problems (5).
About 80% of stroke patients become dependent on caregivers after discharge from the hospital (6). In such conditions, caregivers usually face situations for which they have not been trained (7). According to studies, the highest care burden in caregivers of patients with brain stroke is at the time of hospitalization and the first month after discharge. In this period, they are in need of quick learning of care techniques (8, 9). Because patient care is affected by the life changes of caregivers, this issue needs further attention (10). The caregivers need information about the disease, management of behavioral, psychological, and physical problems, and access to supportive organizations (11).
Although patients with brain stroke and their caregivers receive special caring guidelines at the time of discharge from the hospital, this supportive care might not continue after discharge from the hospital (12). The lack of sufficient information can interfere with the recovery of patients; therefore, the patients and their families should not be left alone in this situation (13). Continuity in care reduces anxiety and promotes client health and activity (14). Remote learning is an effective way of patient teaching because it eliminates time and space limitations (15). Telenursing is a kind of nurse communication with a remote patient to provide information for patient care (16). It is an affordable and effective way to support caregiving at home (10).
2. Objectives
Given the high prevalence of brain stroke and its major complications in developing countries, including Iran, the main purpose of this study was to determine the impact of remote follow-up and counseling on the caregivers’ burden of care and the frequency of some complications in stroke patients discharged from the neurology wards of hospitals affiliated with Qom University of Medical Sciences, Qom, Iran.
3. Methods
This two-arm parallel-group single-blind randomized clinical trial study was approved by the Ethics Committee of Shiraz University of Medical Sciences, Fars, Iran (ethics code: IR.SUMS.REC.1398.297).
3.1. Sample Size
The required sample size in this study was estimated at 72 patients with their primary caregivers, based on the results of Ghane et al.’s study (17), at the error level of 0.05, power of 90%, and 30% probability of sample dropping. The sample size was calculated by G*Power software (version 3.1.9.2).
3.2. Recruitment
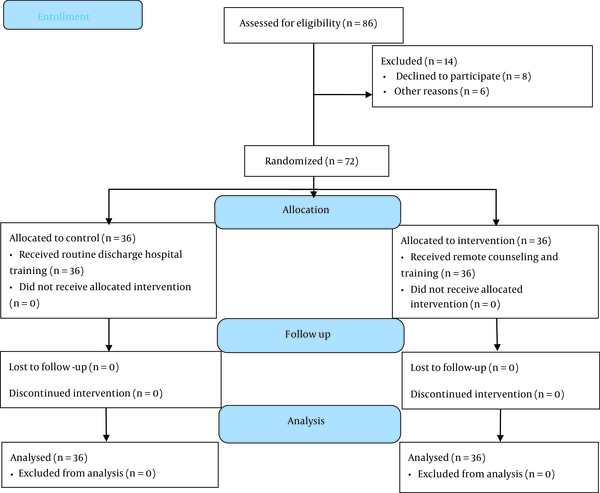
After approving the project by the Ethics Committee of Shiraz University of Medical Sciences and obtaining all licenses from Qom University of Medical Sciences, the researcher referred to the Department of Neurology and searched for patients who had the necessary criteria to enter the study. After explaining the purpose and process of the research to patients and their caregivers, those who were satisfied with participating in the study read and signed an informed consent form. Recruitment began in September 2019 and ended in January 2020. In this period, 86 patients with acute brain stroke were assessed for eligibility, 14 of whom did not meet the inclusion criteria (8 patients declined to participate, and 6 patients had other exclusion criteria). All 72 eligible patients entered the study and continued their collaboration up to the end of the study (Figure 1). The inclusion criteria were having an acute stroke diagnosis approved by a neurologist, willingness to participate in research, access to a cellphone, normal hearing, vision, and mental ability, and having a caregiver under several conditions, including fluency in Farsi, no neurological and mental disorders, and not a member of the medical center. The exclusion criteria were readmission, history of the previous hospitalization due to stroke, patient death, unwillingness to continue cooperation, and presence of pressure ulcers at discharge time.
Flow diagram of study
3.3. Randomization and Blinding
The patients were divided into two intervention and control groups by block randomization. In the case of block size 4, there were six possible combinations of the group assignment. One of these combinations was selected at random, and the four participants were assigned accordingly. This process was repeated until all the samples were included and the sampling sequence recorded in a table. According to the preset table, all of the patients were divided into intervention and control groups. The patients were blinded to group allocation. Although general information about the study was provided to all participants, consultations were only given to the intervention group based on the patients’ needs, and the control group was not aware of their content.
3.4. Tools for Data Collection
The data were collected by five tools, including a demographic questionnaire, Caregiver Burden Inventory (CBI), Braden Scale, Morse Scale, and a urinary problem checklist.
- Demographic Questionnaire: This questionnaire contained information about individual characteristics, medical history, used medication, and the patient’s primary caregiver.
- Caregiver Burden Inventory: CBI has been devised by Novak and Guest (1989) to measure objective and subjective care load. This inventory includes five subscales that are time-related care burden, complementary care burden, physical care burden, social care burden, and emotional care burden. The Cronbach’s alpha of time-related and complementary care burden was 0.85. The Cronbach’s alpha coefficients of physical, social, and emotional care burden subscales were 0.86, 0.77, and 0.73, respectively (18). In Iranian society, the content validity index of the Farsi version of this questionnaire was measured at 91.8%, 90.2%, 93.6%, and 91.86% in terms of relevancy, clarity, fluency, and altogether, respectively (19). Its construct validity was approved by known group comparison and criterion validity. In addition, internal consistency and test-retest reliability were 0.930 and 0.960, respectively (20). The CBI consists of 24 items, with minimum and maximum scores of 0 and 96, respectively. Obtaining grades over 36 indicates an excessive care burden on the individual.
- Braden Scale: This is a standard tool for the measurement of susceptibility to pressure ulcers, which consists of six subscales of sensory perception, moisture, activity, mobility, friction, and shear. The validity and reliability of the Braden Scale were approved by some studies (21).
- Morse Scale: This is a standard tool for the measurement of susceptibility to falls, which consists of six items of the fall history, presence of a secondary diagnosis, use of an ambulatory aid, use of an intravenous apparatus or heparin lock, impaired gait, and impaired mental status. Its predictive validity and interrater reliability were approved (22).
- Urinary problem checklist: This checklist consists of eight items related to the signs and symptoms of urinary problems, which were scored based on the presence or absence of the signs and symptoms (Table 1).
Diagnostic Criteria of Desired Outcomes
| Outcomes | Diagnostic Criteria |
|---|---|
| Caregiver burden | The burden of care placed on the primary caregiver and measured by Novak’s care questionnaire |
| Falls | Sudden and involuntary falls from walking, standing, or sitting position |
| Bedsores | Any skin damage in the form of loss of the surface layer of the skin to the occurrence of deep secondary wounds to immobility and pressure |
| Urinary problems | The existence of any of the following urinary signs and symptoms: frequent urination, pain and burning sensation in urination, polyuria and oliguria, bad smell of urine, darkness and turbidity of urine, and the presence of purulent discharge |
3.5. Intervention
The intervention included a standard educational content to increase patient-caregiver awareness of preventative measures for the three most common stroke complications, including bedsores, urinary infections, and falls. In addition, information about available medical and support centers was provided to caregivers. The participants in the intervention group received remote training and counseling by a specialist nurse to reduce the caregiver burden of care and prevent pressure ulcers, falls, and urinary tract problems in addition to routine training in the hospital.
The tool for training and consulting with the participants was their mobile phones. It was the best way of fast, easy, and low-cost consulting without the need for expensive hardware and software according to the age, economic, and educational conditions of the participants since most of them lived in rural areas and did not have access to quality internet.
In the first week after discharge, all patients in the intervention group received educational content during at least three phone calls. In the next 3 weeks, counseling and telephone follow-up were performed based on their needs. The phone calls were from 8 a.m. to 8 p.m., and each call lasted between 15 to 20 minutes. In addition, the participants in the intervention group could call the nurse if they needed telephone counseling at any time of day and night. However, the control group received only routine discharge training provided by the department personnel. Due to ethical considerations, after data collection, a brief summary of the teaching in the form of pamphlets was provided for patients in the control group.
3.6. Information Collection and Analysis
Prior to the intervention, the burden of care in caregivers was evaluated by the CBI. The risks of falls, bedsores, and urinary tract infections in patients were evaluated by Morse and Braden scales and the checklist for urinary tract infections. One month after the intervention, the caregiver burden of care, the number of falls, the presence of signs and symptoms of bedsores, and urinary tract infections in patients were assessed through telephone interviews (Table 1). In case of ambiguity about pressure ulcers or urinary problems, the researcher examined ambiguous cases directly. After data collection, the data were analyzed using the chi-square test, Mann-Whitney U test, independent t-test, and paired t-test by SPSS software (version 24).
4. Results
According to the findings of this study, 86% of caregivers of patients with stroke had an excessive burden of care when their patients were discharged from the hospital. The findings showed no significant differences between the baseline characteristics of the two groups, except for kinship between the patients and their caregivers. In addition, before the intervention, the mean scores of the CBI, susceptibility scores to pressure ulcers, and falling in the two groups were not different significantly. However, before the intervention, the rates of urinary problems in the two groups were significantly different (Table 2).
| Variables | Intervention Group | Control Group | P-Value |
|---|---|---|---|
| Patient Characteristics | |||
| Age (y) | 65.89 ± 12.559 | 69.72 ± 14.587 | 0.237 b |
| Gender | 0.151 c | ||
| Male | 24 (66.7) | 18 (50.0) | |
| Female | 12 (33.3) | 18 (50.0) | |
| Educational status | 0.107 c | ||
| High school | 30 (83.3) | 35 (97.2) | |
| Diploma and higher | 6 (16.7) | 1 (2.8) | |
| Marital status | 0.448 c | ||
| Single | 0 (0.0) | 0 (0.0) | |
| Married | 26 (72.2) | 23 (63.9) | |
| Divorced/Wife’s death | 10 (27.8) | 13 (36.1) | |
| Job status * | 0.358 c | ||
| Practitioner | 13 (36.1) | 8 (22.2) | |
| Unemployed/Retired | 11 (30.6) | 11 (31) | |
| Housewife | 12 (33.3) | 17 (47.2) | |
| Type of stroke | 0.260 c | ||
| Ischemic | 30 (83.3) | 34 (94.4) | |
| Hemorrhagic | 6 (16.7) | 2 (5.6) | |
| Days of hospitalization * | 8.44±4.319 | 11.75±10.581 | 0.087 b |
| Urinary catheter | 9 (25.0) | 7 (19.4) | 0.571 c |
| Braden score | 19.17±4.482 | 18.06±4.720 | 0.309 |
| Morse score | 37.361±28.1193 | 42.917±28.7942 | 0.410 |
| Caregiver Characteristics | |||
| Age (y) | 44.11±12.524 | 44.47±10.840 | 0.895 b |
| Gender | 0.674 c | ||
| Male | 4 (11.1) | 2 (5.6) | |
| Female | 32 (88.9) | 34 (94.4) | |
| Educational status | 0.950 c | ||
| High school | 23 (63.9) | 23 (63.9) | |
| Diploma | 6 (16.7) | 8 (22.2) | |
| Higher than diploma | 7 (19.4) | 5 (14.0) | |
| Employment status | 1.000 c | ||
| Employed | 6 (16.7) | 6 (16.7) | |
| Housewife | 29 (80.6) | 29 (80.6) | |
| Unemployed/Retired | 1 (2.8) | 1 (2.8) | |
| Marital status | 0.565 c | ||
| Single | 4 (11.1) | 3 (8.3) | |
| Married | 30 (83.3) | 33 (91.7) | |
| Divorced/Wife’s death | 2 (5.6) | 0 (0.0) | |
| Kinship with the patient | 0.038 c | ||
| Spouse | 19 (52.8) | 12 (33.3) | |
| Daughter | 8 (22.2) | 20 (55.6) | |
| Others | 9 (25.1) | 4 (11.2) | |
There was a significant difference between the burden of care in caregivers in the control and counseling groups after the intervention (27.56; 95% CI: 22.96 - 32.15). The CBI score decreased after one month in the counseling group and increased in the control group. In addition, during the study, the control patients had more experience of falling down and urinary problems than the counseling group [n = 7 (19.4%) vs. n = 0 (0.0%); P = 0.011; n = 22 (61.1%) vs. n = 0 (0.0%); P < 0.001, respectively].
None of the signs of pressure ulcers were identified in the intervention group; nevertheless, in the control group, five cases (13.9%) showed signs of pressure ulcers, although this difference was not statistically significant (P = 0.054). Table 3 shows the study outcomes before and after the intervention in the two groups.
| Outcome | Control Group | Intervention | P-Value (Intergroup) | ||
|---|---|---|---|---|---|
| Before | After | Before | After | ||
| CBI score | 24.50 (15, 34) | 34.50 (22.25, 48.75) | 25.00 (16.25, 34.00) | 6.00 (0.25, 14.25) | < 0.001 b |
| P-value (intragroup) | < 0.001 c | < 0.001 c | - | ||
| Diff CBI (before-after) | -11.00 (-16.75, -6.00) | 18.00 (11.00, 23.00) | < 0.001 b | ||
| Symptomatic of urinary infection | 4 (11.1) | 22 (61.1) | 11 (30.6) | 0 (0.0) | < 0.001 d |
| P-value (intragroup) | < 0.001 c | < 0.001 c | - | ||
| Pressure sore | - | 5 (13.9) | - | 0 (0.0) | 0.054 d |
| Falling down | - | 7 (19.4) | - | 0 (0.0) | 0.011 d |
5. Discussion
This study was performed on 72 patients with acute stroke and their caregivers to investigate the effect of telenursing on care burden in caregivers, the incidence of bedsores, the frequency of symptomatic urinary infections, and the number of falls in patients. According to the findings of this study, 86% of caregivers of participants in the intervention and control groups had an extensive care burden at the time of discharge from the hospital. In this context, other studies emphasized that the caregivers of patients with acute brain stroke experience high care burden (17).
The results showed that training and telephone counseling to caregivers according to their educational needs effectively reduced their caregiver burden. This result is consistent with the results of other studies conducted on patients who had open-heart surgery, Alzheimer’s, and heart failure (23-25). Regarding the incidence of pressure ulcers, none of the participants in the intervention group reported the signs of pressure ulcers; however, bedsores were observed in five (14%) participants in the control group. Although this finding can be clinically important, the difference was not statistically significant. In this regard, Shahrokhi et al. stated that telephone education and counseling could not improve caregiving performance in preventing pressure ulcers (10). Another study conducted on 160 bedridden elderly patients emphasized that home teaching can improve the caregiver’s performance in the prevention of pressure ulcers (26).
Regarding symptomatic urinary infections, before the intervention, both groups had some signs and symptoms of urinary infections; nonetheless, after the intervention, none of the participants in the counseling group had signs and symptoms of new urinary infections, and even some of the previous cases had recovered; however, 61% of the participants in the control group had new symptomatic urinary infections. This finding suggests that the telenursing program can effectively help prevent new urinary infections and treat previous cases. Similar to the aforementioned finding, de Souza-Junior et al. showed that remote education and counseling in patients with urinary catheterization leads to a decreased chance of getting infected with urinary infections and other related problems (27).
Falls were considered another outcome of this study. Based on the results, none of the participants in the counseling group reported falls; nevertheless, 19.4% of the participants in the control group experienced falls. In this respect, Williams et al. demonstrated that remote education and counseling prevent falls in patients with acute brain stroke (28). However, Hill et al. stated that providing personal fall prevention training before discharge did not reduce the number of patients’ falls at home after discharge (29).
Moreover, similar studies have indicated that remote follow-up can help the patient and his/her family to be active in the treatment process; for example, Ferraris et al. concluded in their research that remote follow-up via email could be an effective way for better management of the classical ketogenic regimen, especially in patients living away from the reference care center (30). The evidence suggests that telenursing is an appropriate tool for the enhancement of health-related awareness to provide patient care at home (10). Telenursing reduces patients’ hospitalization and enhances the patients’ adherence to diets and medications (31-33).
Among communication technologies, the telephone has the most applicability in telenursing due to its availability (10). Phone follow-up is cost-effective, has no specific timeframe, and reduces depression and anxiety in patients’ caregivers (6). Studies showed that phone follow-up significantly improved self-care in patients with chronic respiratory failure after discharge (34). Moreover, the results of another study showed that phone follow-up effectively reduced the weight of obese adolescents (16). Based on the results of the present study, remote education and counseling reduced the care burden on caregivers and prevented the long-term consequences of the disease, such as pressure ulcers, urinary problems, and the possibility of falling in patients.
5.1. Limitations
In this study, only symptomatic cases of urinary tract infections were detected. The diagnosis of asymptomatic patients is one of the limitations of this study. In addition, instead of incident cases, the frequency of urinary tract infections in the control and test groups before and after the intervention was compared. Furthermore, the process of completing the questionnaires was time-consuming, which could have caused dissatisfaction among the participants.
5.2. Conclusions
Telenursing has effectively reduced the burden of care on caregivers, the occurrence of urinary problems, and the possible falling in patients with acute stroke. Therefore, considering the importance of following up on patient care after hospital discharge and the important role of nurses in this issue, it is suggested to provide the necessary training and skills for telenursing programs for nurses that improve the health and quality of life of patients with acute stroke and their caregivers.
References
-
1.
Ghayeghran AR, Bakhshayesh Eghbali B, Hosseini Nejad M, Kazem Nejad E. Survey of Various Post Stroke Pain Syndromes and the Related Risk Factors. J Guilan Univ Med Sci. 2012;21(82):1-7.
-
2.
GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736-88. [PubMed ID: 30496103]. [PubMed Central ID: PMC6227606]. https://doi.org/10.1016/S0140-6736(18)32203-7.
-
3.
Walter K. What Is Acute Ischemic Stroke? JAMA. 2022;327(9):885. [PubMed ID: 35230392]. https://doi.org/10.1001/jama.2022.1420.
-
4.
Lutz BJ, Young ME, Cox KJ, Martz C, Creasy KR. The crisis of stroke: experiences of patients and their family caregivers. Top Stroke Rehabil. 2011;18(6):786-97. [PubMed ID: 22436315]. [PubMed Central ID: PMC3822775]. https://doi.org/10.1310/tsr1806-786.
-
5.
Bibi S. Nursing Management of patient with cerebral Vascular Accident Stroke. Pak J Chest Med. 2017;23(3):116-8.
-
6.
Goudarzian M, Fallahi-Khoshknab M, Dalvandi A, Delbari A, Biglarian A. Effect of Telenursing on Levels of Depression and Anxiety in Caregivers of Patients with Stroke: A Randomized Clinical Trial. Iran J Nurs Midwifery Res. 2018;23(4):248-52. [PubMed ID: 30034482]. [PubMed Central ID: PMC6034534]. https://doi.org/10.4103/ijnmr.IJNMR_242_16.
-
7.
Bakas T, Jessup NM, McLennon SM, Habermann B, Weaver MT, Morrison G. Tracking patterns of needs during a telephone follow-up programme for family caregivers of persons with stroke. Disabil Rehabil. 2016;38(18):1780-90. [PubMed ID: 26680007]. [PubMed Central ID: PMC4912456]. https://doi.org/10.3109/09638288.2015.1107767.
-
8.
Bibi S. Stroke Caregiving: Difficult Times, Resource Use, and Needs During the First 2 Years. J Gerontol Nurs. 2006;32(4):37-44. https://doi.org/10.3928/00989134-20060401-07.
-
9.
Cameron JI, Naglie G, Silver FL, Gignac MA. Stroke family caregivers' support needs change across the care continuum: a qualitative study using the timing it right framework. Disabil Rehabil. 2013;35(4):315-24. [PubMed ID: 22686259]. https://doi.org/10.3109/09638288.2012.691937.
-
10.
Shahrokhi A, Azimian J, Amouzegar A, Oveisi S. Effect of Telenursing on Outcomes of Provided Care by Caregivers of Patients With Head Trauma After Discharge. J Trauma Nurs. 2018;25(1):21-5. [PubMed ID: 29319646]. https://doi.org/10.1097/JTN.0000000000000338.
-
11.
Young ME, Lutz BJ, Creasy KR, Cox KJ, Martz C. A comprehensive assessment of family caregivers of stroke survivors during inpatient rehabilitation. Disabil Rehabil. 2014;36(22):1892-902. [PubMed ID: 24467676]. [PubMed Central ID: PMC4959419]. https://doi.org/10.3109/09638288.2014.881565.
-
12.
Wan LH, Zhang XP, Mo MM, Xiong XN, Ou CL, You LM, et al. Effectiveness of Goal-Setting Telephone Follow-Up on Health Behaviors of Patients with Ischemic Stroke: A Randomized Controlled Trial. J Stroke Cerebrovasc Dis. 2016;25(9):2259-70. [PubMed ID: 27371106]. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.05.010.
-
13.
Ashghali Farahani M, Najafi Ghezeljeh T, Haghani S, Alazmani-Noodeh F. The effect of a supportive home care program on caregiver burden with stroke patients in Iran: an experimental study. BMC Health Serv Res. 2021;21(1):346. [PubMed ID: 33858400]. [PubMed Central ID: PMC8048267]. https://doi.org/10.1186/s12913-021-06340-4.
-
14.
Hekmatpou D, Baghban EM, Mardanian Dehkordi L. Erratum: The Effect Of Patient Care Education On Burden Of Care And Quality Of Life Of Caregivers Of Stroke Patients [Corrigendum]. J Multidiscip Healthc. 2019;12:881. [PubMed ID: 31806985]. [PubMed Central ID: PMC6842897]. https://doi.org/10.2147/JMDH.S232970.
-
15.
Chakeri A, Salehi S, Ab Gharebagh Z, Haghani S. Evaluating effect of Tele-nursing on the quality of life of cancer patients admitted to selected hospitals of Tehran University of Medical Sciences, 2014-2015. Int J Ayurveda Res. 2018;9(2):83-7. https://doi.org/10.47552/ijam.v9i2.1069.
-
16.
Bennett EA, Kolko RP, Chia L, Elliott JP, Kalarchian MA. Treatment of Obesity Among Youth With Intellectual and Developmental Disabilities: An Emerging Role for Telenursing. West J Nurs Res. 2017;39(8):1008-27. [PubMed ID: 28349744]. [PubMed Central ID: PMC5913737]. https://doi.org/10.1177/0193945917697664.
-
17.
Ghane G, Ashghali Farahani M, Seyedfatemi N, Haghani H. [Effectiveness of supportive educative program on the burden in family caregivers of hemodialysis patients]. Cent Eur J Nurs Midwifery. 2017;14(10):885-95. Persian.
-
18.
Novak M, Guest C. Application of a multidimensional caregiver burden inventory. Gerontologist. 1989;29(6):798-803. [PubMed ID: 2516000]. https://doi.org/10.1093/geront/29.6.798.
-
19.
Abbasi A, Shamsizadeh M, Asayesh H, Rahmani H, Hosseini S, Talebi M. [The relationship between caregiver burden with coping strategies in Family caregivers of cancer patients]. Iran J Nurs Res. 2013;1(3):62-71. Persian.
-
20.
Shafiezadeh A, Heravi-Karimooi M, Mirzaee A, Rejeh N, Sharif Nia H, Montazeri A. Psychometric characteristics of the Iranian Caregiver Burden Inventory (CBI) in caregivers of elderly patients with Alzheimer. Health Qual Life Outcomes. 2020;18(1):255. [PubMed ID: 32727503]. [PubMed Central ID: PMC7391597]. https://doi.org/10.1186/s12955-020-01509-7.
-
21.
Wei M, Wu L, Chen Y, Fu Q, Chen W, Yang D. Predictive Validity of the Braden Scale for Pressure Ulcer Risk in Critical Care: A Meta-Analysis. Nurs Crit Care. 2020;25(3):165-70. [PubMed ID: 31985893]. https://doi.org/10.1111/nicc.12500.
-
22.
Baek S, Piao J, Jin Y, Lee SM. Validity of the Morse Fall Scale implemented in an electronic medical record system. J Clin Nurs. 2014;23(17-18):2434-40. [PubMed ID: 24112535]. https://doi.org/10.1111/jocn.12359.
-
23.
Chiang LC, Chen WC, Dai YT, Ho YL. The effectiveness of telehealth care on caregiver burden, mastery of stress, and family function among family caregivers of heart failure patients: a quasi-experimental study. Int J Nurs Stud. 2012;49(10):1230-42. [PubMed ID: 22633448]. https://doi.org/10.1016/j.ijnurstu.2012.04.013.
-
24.
NasrAbadi T, Sharafi SH, Fallah Tafti B, Vaezi AA, Heidari MR. [Investigating the effect of continuous care model on social health status of family caregivers in hospitalized patients undergoing coronary artery bypass graft surgery]. J Shahid Sadoughi Univ Med Sci. 2016;24(6):513-23. Persian.
-
25.
Salehi Nejad S, Azami M, Motamedi F, Sedighi B, Shahesmaili A. [The effect of web-based information intervention in caregiving burden in caregivers of patients with dementia]. Journal of Health and Biomedical Informatics. 2017;4(3):181-91. Persian.
-
26.
Alhammadi HMA, Ogale RJ. Effectiveness of home caregivers teaching program on prevention of decubitus ulcer in bed ridden elderly patients. Int J Nurs Stud. 2020;7(2):67-9.
-
27.
de Souza-Junior VD, Mendes IAC, Mazzo A, de Godoy S, Dos Santos CA. Telenursing Intervention for Clean Intermittent Urinary Catheterization Patients: A Pilot Study. Comput Inform Nurs. 2017;35(12):653-60. [PubMed ID: 28692432]. https://doi.org/10.1097/CIN.0000000000000370.
-
28.
Williams LM, Hubbard KE, Daye O, Barden C. Telenursing in the intensive care unit: transforming nursing practice. Crit Care Nurse. 2012;32(6):62-9. [PubMed ID: 23203956]. https://doi.org/10.4037/ccn2012525.
-
29.
Hill AM, McPhail SM, Haines TP, Morris ME, Etherton-Beer C, Shorr R, et al. Falls After Hospital Discharge: A Randomized Clinical Trial of Individualized Multimodal Falls Prevention Education. J Gerontol A Biol Sci Med Sci. 2019;74(9):1511-7. [PubMed ID: 30721940]. [PubMed Central ID: PMC7330456]. https://doi.org/10.1093/gerona/glz026.
-
30.
Ferraris C, Guglielmetti M, Tamagni E, Trentani C, De Giorgis V, Pasca L, et al. Use of Remote Monitoring by E-mail for Long-Term Management of the Classic Ketogenic Diet. Nutrients. 2020;12(6). [PubMed ID: 32575586]. [PubMed Central ID: PMC7353224]. https://doi.org/10.3390/nu12061833.
-
31.
Shahabi N, Kolivand M, Salari N, Abbasi P. The effect of telenursing training based on family-centered empowerment pattern on compliance with diet regimen in patients with diabetes mellitus type 2: a randomized clinical trial. BMC Endocr Disord. 2022;22(1):36. [PubMed ID: 35139832]. [PubMed Central ID: PMC8830007]. https://doi.org/10.1186/s12902-022-00953-4.
-
32.
Najafi SS, Shaabani M, Momennassab M, Aghasadeghi K. The nurse-led telephone follow-up on medication and dietary adherence among patients after myocardial infarction: a randomized controlled clinical trial. Int J Community Based Nurs Midwifery. 2016;4(3):199-208. [PubMed ID: 27382586]. [PubMed Central ID: PMC4925999].
-
33.
Sato D. Effectiveness of Telenursing for Postoperative Complications in Patients with Prostate Cancer. Asia Pac J Oncol Nurs. 2020;7(4):396-403. [PubMed ID: 33062837]. [PubMed Central ID: PMC7529028]. https://doi.org/10.4103/apjon.apjon_28_20.
-
34.
Lao X, Zhang J, Bai C. The implication of telehealthcare in COPD management of China. Expert Rev Respir Med. 2013;7(5):459-63. [PubMed ID: 24138690]. https://doi.org/10.1586/17476348.2013.838019.