Abstract
Background:
Females encounter various stresses during life. Different courses of female’s life, namely menstruation, pregnancy, and childbirth, cause particular physical and mental changes that make them more vulnerable.Objectives:
The purpose of this study was to investigate the effect of group counseling based on cognitive-behavioral approach on pregnancy-specific stress and anxietyMethods:
This randomized trial recruited 62 qualified pregnant females during year 2016. The participants were selected through convenience sampling and divided to 2 groups, the intervention and the control group, based on randomized blocks of 4. The control group received routine prenatal care and an instructional package for dealing with stresses during pregnancy. The intervention group received counseling for 6 sessions of 90 minutes besides routine prenatal care. Both groups were evaluated at baseline and at the end of the study using pregnancy-specific stress and anxiety questionnaire. The collected data were analyzed using the SPSS16 software.Results:
Based on the results of this study, the 2 groups did not significantly differ in terms of age, educational level, occupation, ethnicity, and housing. The score of stress during pregnancy was not significantly different at baseline either. However, mean score of stress after the intervention was significantly lower in the intervention group than the control group (P = 0.001).Conclusions:
Cognitive-behavioral counseling can be used as an optional method for reducing the pregnancy-specific stress and anxiety, and improving the pregnant female’s mental health.Keywords
Counseling Pregnancy-Specific Stress and Anxiety Cognitive-Behavioral Pregnancy
1. Background
Pregnancy is an event that changes how a woman looks at the world and effects her health, emotions, and social roles (1). Although it is considered an enjoyable life event that helps females grow, pregnancy and motherhood can induce some degrees of stress and anxiety in females due to physical and mental changes they bring with themselves (2).
Studies suggest that stress and anxiety are a psychological problem in pregnant females with a U-shaped relationship; that is, the level of stress and anxiety escalates in the first and third trimesters (3-6). Studies have reported the prevalence of stress and anxiety during pregnancy as 6% to 78%; that is, 6% of the population is reportedly exposed to high levels of stress and 78% is exposed to low or moderate levels (7-9). Stress during pregnancy can be associated with adverse pregnancy outcomes such as miscarriage, fetal weight loss, increased stress hormone levels, chronic hypertension, premature birth, infant mortality, changes in endocrine secretion, changes in hypothalamic-pituitary function, suppressed immune system, changes in the number of lymphocytes and reduced CD4/CD8 ratio, nausea, vomiting, preeclampsia, and some degree of mental disorder (10-16). The complications associated with pregnancy-induced stress are a leading cause of maternal perinatal mortality (17). Stress also leads to adverse health behaviors such as smoking and alcohol consumption, which act as an intermediary between stress and its manifestations (18). Some researchers believe that severe stress during pregnancy negatively effects the mother-infant relationship and reduces the mother’s ability to play her maternal role (19, 20). Female’s mental health therefore deserves greater attention, as hopefulness, vitality, and freshness are mental attributes that can significantly affect the mothers’ functioning and active performance of her maternal role and essentially lead to a happier future generation (21). Today, a variety of non-pharmacological interventions are available to the public for the control of stress and anxiety, with the most common being counseling and training by nurses and midwives as healthcare providers with a significant role in preventing pregnancy and postpartum stress and anxiety (22). Counseling or therapy is a stress management strategy that can be offered with a variety of different approaches, including the cognitive-behavioral approach (23).
Psychological education based on cognitive-behavioral approach teaches mothers coping strategies and problem-solving skills, enables them to evaluate psychological situations and pressures, and changes their perspective toward themselves, the world, the future, and the attitudes that apparently lead to their greater vulnerability to emotional disorders, and as a result they feel better about themselves and their children (24, 25).
Many studies have addressed the effect of non-pharmaceutical interventions, such as stress management based on cognitive-behavioral method on stress, anxiety, and depression of females in Iran and other countries. For example, in their studies, Karamozian (2015), Jabari (2012), and Yominakano (2013) found that stress management based on cognitive-behavioral approach significantly obviates female’s anxiety (2, 26, 27). However, the search conducted by the researchers failed to find a study on the effect of group counseling on pregnancy-specific stress and anxiety. Counseling may be performed on people or in groups. To the best of our knowledge, group counseling is superior to individual counseling in critical situations when stress accompanies uncomfortable moods, and individuals find themselves broken, inefficient, helpless, fearful, and failed. Group counseling is a thoughtful effort to change thoughts, feelings, and behaviors of group members (28).
2. Objectives
Given the importance of maternal and fetal health and given the effect of psychological problems on pregnancy outcomes, the present study was conducted to determine the effect of group cognitive-behavioral therapy on pregnancy-specific stress and anxiety.
3. Methods
3.1. Study Design
The present controlled, randomized, parallel trial was conducted on 70 pregnant females aged 18 to 35 that had referred to select healthcare centers in Karaj, Iran. According to a review of literature and relevant studies on the subject, the minimum sample size was estimated as 31 per group with a standard deviation of 8; considering a sample loss of 10%, 35 samples were ultimately assigned to each group.
The appropriate sample size was determined, according to the following formula:
The participants were selected from eligible primiparous females that had referred to selected healthcare centers of Karaj, Iran.
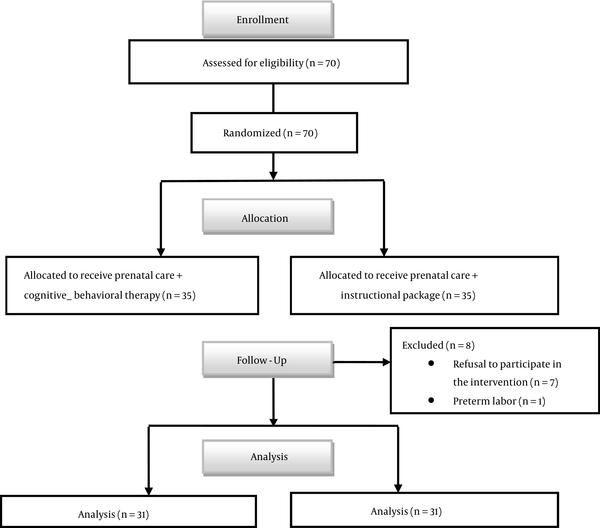
The study inclusion criteria consisted of age of 18 to 35, Iranian nationality, gestational age of 20 to 32 weeks (post LMP or according to the 12 week ultrasound), singleton pregnancy, primiparity, a minimum of high school diploma, having stress based on the pregnancy-specific stress and anxiety questionnaire, a self-reported lack of mental illness and depressive disorders and not using anti-anxiety and anti-stress medications or antidepressants according to the self-reports. The exclusion criteria consisted of a failure to participate in 2 or more sessions of therapy, unwillingness to continue participation in the study, and having experienced adverse life events during the past 6 months (such as the death of the husband or a first-degree relative, divorce, husband’s imprisonment, etc.). The 70 eligible participants were divided to 2 groups in randomized blocks of 4, namely the intervention group (cognitive-behavioral counseling + routine care) and the control group (routine care + the instructional package). In the course of the study, 2 females had preterm labor and 7 refused to participate in the intervention and were thus excluded from the study, leaving 62 participants to complete the research (Figure 1).
Consort Flow Diagram
3.2. Data and Measures
Data were collected with 2 questionnaires, including a demographic form (with items on age, education, occupation, ethnicity, housing status, living arrangements, income, and living with spouse’s family) and the pregnancy worries and stress questionnaire (PWSQ). The PWSQ has 25 items within 6 categories, including maternal health (6 items), infant health (5 items), experience of childbirth and motherhood (4 items), mother-child bonding (2 items), personal-family domain (5 items), and personal-occupational domain (3 items). The scoring system was based on a 5-point Likert scale (always, often, sometimes, rarely, and never) with minimum and maximum scores of zero and 100. The validity and reliability of the tool were confirmed in Iran by a study conducted on Iranian females by Fariba Navidpour et al. (2015). The Cronbach’s alpha (0.89) and test-retest reliability were used to confirm the tool as an appropriate measure of pregnancy-specific stress and anxiety among Iranian females (24).
3.3. Process
This randomized trial was conducted in 2016 at selected centers of Alborz province. Before beginning the study, permissions were obtained from the research deputy, ethics committee, and president of the university and relevant units. The researcher visited the centers for sampling and identified eligible pregnant females and explained the study objectives to them. Written consents were obtained from those willing to participate in the study. The subjects were divided to an intervention and a control group in randomized blocks of 4.
In addition to routine prenatal care provided for both groups, the control group also received instructional booklets on how to deal with stress and anxiety during pregnancy (the same topics covered for the intervention group) and the intervention group also participated in 6 cognitive-behavioral therapy sessions of 90 minutes twice per week based on Michael Baum’s treatment guide (Table 1). At the end of the 6 sessions, both groups were given the PWSQ to fill out and their pre- and post-intervention data were compared and then analyzed using the SPSS-16 software.
Interventions Performed for Control and Intervention Groups
| Meeting | Intervention Group (Cognitive - Behavioral Counseling + Routine Care) | Control Group (Routine Care) |
|---|---|---|
| Session 1 | Introduction to stress and stress coping methods | Introduction to pregnancy and its symptoms and personal and psychological health |
| Session 2 | Education and counseling subjective methods for coping with stress | Personal and psychological health |
| Session 3 | Counseling physical methods for coping with stress | Sexual health |
| Session 4 | Identifying ineffective thoughts and cognitive errors | Nutrition and nutritional supplements |
| Session 5 | Reviewing assignments, and performing abdominal breathing and muscular relaxation | Introduction to risk factors |
| Session 6 | Problem-solving training | Breastfeeding training and postpartum care instructional booklets |
The intervention group received routine counseling (the same as the control group) plus the above counseling in every session
The research project was confirmed by the ethics committee of Alborz University of Medical Sciences and health services on 23rd of April, 2016, under the code Abzums.Rec.1395.19 and was registered at the Iranian registry of clinical trials with ID number IRCT2016052527728N2.
4. Results
The study was conducted on 62 pregnant females divided to an intervention (cognitive-behavioral therapy and routine care) and a control (routine care and the instructional package) group. The normality of the variables was assessed using the Kolmogorov-Smirnov test and the 2 groups were found to be matching and did not differ significantly in terms of age, level of education, employment status, housing status, and ethnicity (P = 0.001); however, a significant difference was observed between the groups in terms of income (P = 0.02) (Table 2).
The Demographic Characteristics of the Participants of the Intervention and Control Groups
| Variables and Levels | Intervention Group N = 31, f (%) | Control Group N = 31, f (%) | Total N = 62, f (%) | P Value |
|---|---|---|---|---|
| Age | 0.50 | |||
| 24 - 18 | 9 (29) | 10 (32.3) | 19 (30.64) | |
| 29 - 25 | 14 (45.2) | 15 (48.4) | 29 (46.77) | |
| 35 - 30 | 8 (25.8) | 6 (19.4) | 14 (22.58) | |
| Education | 0.09 | |||
| Diploma | 12 (38.7) | 19 (61.3) | 31 (50) | |
| Associate degree and bachelor | 18 (58.1) | 11 (35.5) | 29 (46.77) | |
| Master and other | 1 (3.2) | 1 (3.2) | 2 (3.22) | |
| Job Status | 0.64 | |||
| Housekeeper | 29 (93.5) | 28 (90.3) | 57 (91.93) | |
| Employed | 2 (6.5) | 3 (9.7) | 5 (8.06) | |
| Income | 0.02 | |||
| Weak | 1 (3.2) | 7 (22.6) | 8 (12.90) | |
| Average | 25 (80.6) | 22 (71) | 47 (75.80) | |
| Good | 5 (16.1) | 2 (6.5) | 7 (11.29) | |
| Housing | 0.18 | |||
| Owner | 13 (41.9) | 8 (25.8) | 21 (33.87) | |
| Roomer | 18 (58.1) | 23 (74.2) | 41 (66.12) | |
| Nationality | 0.68 | |||
| Fars | 22 (71) | 18 (58.1) | 40 (64.51) | |
| Kurd | 0 (0) | 5 (16.1) | 5 (8.06) | |
| Turk | 3 (9.7) | 6 (19.4) | 9 (14.51) | |
| Lore | 6 (19.4) | 2 (6.5) | 8 (12.90) |
According to the findings, the PWSQ score did not differ significantly between the 2 groups before the intervention (P > 0.05); after the intervention, however, the mean total PWSQ score was 21.12 ± 15.06 in the intervention group and 39.09 ± 19.55 in the control group. The mean subscale scores were lower in the intervention group than in the controls and made a statistically significant post-intervention difference between the groups (P = 0.01). These scores suggest the effectiveness of the intervention in reducing pregnancy-specific stress. A maximum error rate of 5% was taken into account for all the tests (Table 3).
A Comparison of the Total and Subscale Scores of the Pregnancy Worries and Stress Questionnaire Between the Two Groups
| Stress and Worry of Pregnancy | Before Intervention, N = 31, Mean ± SD | Immediately After Intervention, N = 31, Mean ± SD | P Value |
|---|---|---|---|
| Experience of childbirth and motherhood | |||
| Intervention group | 6.32 ± 3.73 | 3.90 ± 3.36 | 0.001 |
| Control group | 6 ± 4.28 | 7.03 ± 4.22 | 0.03 |
| Infant health | |||
| Intervention group | 4.45 ± 2.76 | 2.32 ± 2.59 | 0.001 |
| Control group | 5.19 ± 3.91 | 4.09 ± 3.03 | 0.6 |
| Mother-child bonding | |||
| Intervention group | 3.12 ± 1.62 | 1.64 ± 1.66 | 0.001 |
| Control group | 3.67 ± 2.28 | 3.61 ± 2.40 | 0.80 |
| Maternal health | |||
| Intervention group | 11.70 ± 5 | 6.83 ± 4.77 | 0.001 |
| Control group | 11.32 ± 5.28 | 12.48 ± 5.37 | 0.9 |
| Personal-family | |||
| Intervention group | 6.64 ± 3.45 | 4.58 ± 3.67 | 0.001 |
| Control group | 8.45 ± 4.91 | 8.38 ± 4.84 | 0.91 |
| Personal-occupational | |||
| Intervention group | 2.70 ± 2.43 | 1.83 ± 2.35 | 0.002 |
| Control group | 3.19 ± 2.90 | 3.48 ± 2.93 | 0.31 |
| Total score | |||
| Intervention group | 34.96 ± 13.89 | 21.12 ± 15.06 | 0.05 |
| Control group | 37.83 ± 19.41 | 39.09 ± 19.55 | 0.53 |
5. Discussion
The results obtained in this study regarding the effect of group cognitive-behavioral therapy on pregnancy-specific stress and anxiety revealed a lower score of stress and anxiety in the intervention group than in the controls after the counseling intervention, which suggests that the use of psychological therapies such as cognitive-behavioral therapy for stress help significantly reduce stress and anxiety in pregnant females. Several studies have examined the effect of group cognitive-behavioral therapy on psychological problems during pregnancy and have unanimously confirmed the positive effects of this therapy in reducing pregnancy-specific anxiety, depression, and stress (25, 26). In one study, Mosallanejad et al. (2012) examined the effect of group cognitive-behavioral therapy on the mental health and courageousness of infertile females undergoing assisted reproductive technologies (ART) and found that group therapy interventions, especially cognitive behavioral therapy, help reduce the score of anxiety, depression, and stress in females undergoing ART (27). In another study, Urizar et al. (2011) examined the effect of cognitive-behavioral therapy for prenatal stress management on saliva cortisol levels in low-income mothers and their infants and found the stress management intervention to be effective in regulating biological markers of stress in mothers and their infants (28). Karamoozian et al. (2013) also examined the effectiveness of a cognitive-behavioral stress management intervention on anxiety and depression during pregnancy and found that providing psychological therapies such as cognitive-behavioral stress management in healthcare centers help effectively improve mothers’ mental health during pregnancy (29). The present study found no significant differences between the 2 groups in terms of the pre-intervention scores of the 6 subscales of pregnancy-specific stress and anxiety while the post-test scores were lower in the intervention group compared to the controls. Cognitive-behavioral therapy appears to have led to this decline. In a study on the effect of cognitive behavioral therapy in reducing mental health problems in females with recurrent pregnancy loss, Yumi Nakano et al. found that the mean score of depression has decreased in the intervention group after cognitive-behavioral therapy (26). Cognitive-behavioral therapy is based on simple principles and follows clearly defined goals. The first and perhaps most important principle in cognitive-behavioral therapy is that direct (immediate) situations and the individual’s interpretation of those situations are what determine his/her behavior. In cognitive therapy, the focus is on these situations and on specific issues rather than general problems.
It seems that the main mechanism of the effect of counseling on reducing maternal stress and anxiety is helping them recognize cognitive errors and irrational beliefs, and change these distorted thoughts and inefficient behaviors using regular discussions and carefully organized behavioral tasks (30).
Given the present study results, although stress control topics were made available to mothers in the form of an educational package, the mean score of stress increased in this group after the intervention. It can therefore be concluded that mere educational content is not sufficient, and counselor’s presence and role in controlling pregnancy stress is highly effective.
Today, given the long history of psychology and the many techniques of therapy and counseling available, and given the increased attention of physicians and researchers to non-pharmacological methods and their revival in the society, finding appropriate alternatives to different chemical medications that effectively improve mental health in pregnancy is essential. The strengths of this study include the use of similar counselor, care practitioner, and therapy sessions for both groups and the random selection of the subjects.
5.1. Limitations
The limitations of this study include the lack of complete control over the mothers’ mental health, their daily encounters with stress and their lifestyle, which may have affected their mental health, and also the mothers’ different mastery and use of life skills, such as stress management, anger management, and problem-solving, given the personal, cultural, and economic differences between them, which may have led to over- or underestimation of stress.
5.2. Conclusion
The findings show that group cognitive-behavioral therapy can be used as a treatment option for reducing pregnancy-specific stress; to increase the effectiveness of this intervention, it does not suffice to examine cognitive errors and negative automatic thoughts; rather, special attention should be paid to irrational and false underlying assumptions and core beliefs of pregnant females and their reform, as well as to their coping skills in the face of stress. It also appears that paying attention to the mental health of pregnant females and the active presence of midwifery consultants in healthcare centers in addition to the centers’ provision of routine prenatal care could help effectively reduce pregnancy-specific stress and anxiety and maternal and fetal complications.
Acknowledgements
References
-
1.
Abdollahzadeh R, Hassanzadeh AM, Ahmadi S, Taheri M, Hosseini M. Relationship between social support with depression and anxiety during third trimester pregnancy. Iran J Nurs Res. 2012;7(26):1-10.
-
2.
Karamoozian M, Askarizadeh G. Impact of prenatal cognitive-behavioral stress management intervention on maternal anxiety and depression and newborns' apgar scores. Iran J Neonatol. 2015;6(2):14-23.
-
3.
Figueiredo B, Conde A. Anxiety and depression symptoms in women and men from early pregnancy to 3-months postpartum: parity differences and effects. J Affect Disord. 2011;132(1-2):146-57. [PubMed ID: 21420178]. https://doi.org/10.1016/j.jad.2011.02.007.
-
4.
Mohammadi ZD, Bosaknejad S, Sarvghad S. A survey on the effectiveness of stress management training with cognitive-behavioral group therapy approach on state/trait anxiety, pregnancy anxiety and mental health of primiparous women. Jentashapir J Health Res. 2013;3(4):495-504.
-
5.
Teixeira C, Figueiredo B, Conde A, Pacheco A, Costa R. Anxiety and depression during pregnancy in women and men. J Affect Disord. 2009;119(1-3):142-8. [PubMed ID: 19346001]. https://doi.org/10.1016/j.jad.2009.03.005.
-
6.
Dolatian M, Mahmoodi Z, Alavi-Majd H, Moafi F, Ghorbani M, Mirabzadeh A. Psychosocial factors in pregnancy and birthweight: Path analysis. J Obstet Gynaecol Res. 2016;42(7):822-30. [PubMed ID: 27098096]. https://doi.org/10.1111/jog.12991.
-
7.
Carolan-Olah M, Barry M. Antenatal stress: an Irish case study. Midwifery. 2014;30(3):310-6. [PubMed ID: 23684696]. https://doi.org/10.1016/j.midw.2013.03.014.
-
8.
Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatry. 2012;25(2):141-8. [PubMed ID: 22262028]. https://doi.org/10.1097/YCO.0b013e3283503680.
-
9.
Takahasi EH, Alves MT, Alves GS, Silva AA, Batista RF, Simoes VM, et al. Mental health and physical inactivity during pregnancy: a cross-sectional study nested in the BRISA cohort study. Cad Saude Publica. 2013;29(8):1583-94. [PubMed ID: 24005924].
-
10.
Aktas S, Yesilcicek Calik K. Factors Affecting Depression During Pregnancy and the Correlation Between Social Support and Pregnancy Depression. Iran Red Crescent Med J. 2015;17(9). eee16640. [PubMed ID: 26473071]. https://doi.org/10.5812/ircmj.16640.
-
11.
Divney AA, Sipsma H, Gordon D, Niccolai L, Magriples U, Kershaw T. Depression during pregnancy among young couples: the effect of personal and partner experiences of stressors and the buffering effects of social relationships. J Pediatr Adolesc Gynecol. 2012;25(3):201-7. [PubMed ID: 22578481]. https://doi.org/10.1016/j.jpag.2012.02.003.
-
12.
Glazier RH, Elgar FJ, Goel V, Holzapfel S. Stress, social support, and emotional distress in a community sample of pregnant women. J Psychosom Obstet Gynaecol. 2004;25(3-4):247-55. [PubMed ID: 15715023].
-
13.
Nik Rahan G, Kajbaf M, Nori A, Zarean E, Naghshine E. The relationship between personality traits, coping styles and stress levels pregnant women. Faculty Edu Sci Isfahan Univ; 2010.
-
14.
Slusarczyk J, Trojan E, Glombik K, Budziszewska B, Kubera M, Lason W, et al. Prenatal stress is a vulnerability factor for altered morphology and biological activity of microglia cells. Front Cell Neurosci. 2015;9:82. [PubMed ID: 25814933]. https://doi.org/10.3389/fncel.2015.00082.
-
15.
Shishehgar S, Mahmoodi A, Dolatian M, Mahmoodi Z, Bakhtiary M, Alavi Majd H. The Relationship of Social Support and Quality of Life with the Level of Stress in Pregnant Women Using the PATH Model. Iran Red Crescent Med J. 2013;15(7):560-5. [PubMed ID: 24396574]. https://doi.org/10.5812/ircmj.12174.
-
16.
Shaban Z, Dolatian M, Shams J, Alavi-Majd H, Mahmoodi Z, Sajjadi H. Post-Traumatic Stress Disorder (PTSD) Following Childbirth: Prevalence and Contributing Factors. Iran Red Crescent Med J. 2013;15(3):177-82. [PubMed ID: 23983994]. https://doi.org/10.5812/ircmj.2312.
-
17.
Cardwell MS. Stress: pregnancy considerations. Obstet Gynecol Surv. 2013;68(2):119-29. [PubMed ID: 23417218]. https://doi.org/10.1097/OGX.0b013e31827f2481.
-
18.
Krabbendam L, Smits L, de Bie R, Bastiaanssen J, Stelma F, van Os J. The impact of maternal stress on pregnancy outcome in a well-educated Caucasian population. Paediatr Perinat Epidemiol. 2005;19(6):421-5. [PubMed ID: 16269069]. https://doi.org/10.1111/j.1365-3016.2005.00679.x.
-
19.
Jabbari Z, Hashemi H, Haghayegh SA. Survey on effectiveness of cognitive behavioral stress management on the stress, anxiety, and depression of pregnant women. 2012.
-
20.
Jokar E, Rahmati A. The effect of stress inoculation training on anxiety and quality of sleep of pregnant women in third trimester. J Fundamental Mental Health. 2015;17(2):103-9.
-
21.
Fava GA, Ruini C, Rafanelli C, Finos L, Conti S, Grandi S. Six-year outcome of cognitive behavior therapy for prevention of recurrent depression. Am J Psychiatry. 2004;161(10):1872-6. [PubMed ID: 15465985]. https://doi.org/10.1176/ajp.161.10.1872.
-
22.
Akbarzadeh M, Toosi M, Zare N, Sharif F. Effect of learning attachment behaviors on anxiety and maternal fetal attachment in first pregnant women. Evidence Based Care. 2011;1(1):21-34.
-
23.
Kar N. Cognitive behavioral therapy for the treatment of post-traumatic stress disorder: a review. Neuropsychiatr Dis Treat. 2011;7:167-81. [PubMed ID: 21552319]. https://doi.org/10.2147/NDT.S10389.
-
24.
Saisto T, Halmesmaki E. Fear of childbirth: a neglected dilemma. Acta Obstet Gynecol Scand. 2003;82(3):201-8. [PubMed ID: 12694113].
-
25.
Taraghijah S, Hamdiyeh M. Effects of cognitive behavioral group counseling in depression.
-
26.
Dunkel Schetter C. Psychological science on pregnancy: stress processes, biopsychosocial models, and emerging research issues. Annu Rev Psychol. 2011;62:531-58. [PubMed ID: 21126184]. https://doi.org/10.1146/annurev.psych.031809.130727.
-
27.
Nakano Y, Akechi T, Furukawa TA, Sugiura-Ogasawara M. Cognitive behavior therapy for psychological distress in patients with recurrent miscarriage. Psychol Res Behav Manag. 2013;6:37-43. [PubMed ID: 23901302]. https://doi.org/10.2147/PRBM.S44327.
-
28.
Kristaini J. Consultation theory and application. Tehran: Roshd; 2011.
-
29.
Navidpour F, Dolatian M, Yaghmaei F, Majd HA, Hashemi SS. Examining Factor Structure and Validating the Persian Version of the Pregnancy's Worries and Stress Questionnaire for Pregnant Iranian Women. Glob J Health Sci. 2015;7(6):308-18. [PubMed ID: 26153186]. https://doi.org/10.5539/gjhs.v7n6p308.
-
30.
Hawton K, Clark DM. Cognitive behaviour therapy for psychiatric problems. Tehran: Arjomand; 2014.