Abstract
Background:
One of the main challenges of all health systems is achieving equity in healthcare financing. The Kakwani index is an equity index used to show how distant a financing source is from the proportional status.Objectives:
The present study aimed to measure the equity of Iran’s health system financing in rural and urban areas between 2001 and 2010 using the Kakwani index.Materials and Methods:
This study analyzed secondary data for the years 2001 through 2010 in Iran. The data of annual household expenditures and an income survey conducted by the statistical center of Iran (SCI) were used in this study. In addition, out of pocket payments and health insurance premiums, as two sources of healthcare financing, were investigated regarding vertical equity. The T-test was used to test the dominance of the curves.Results:
The Kakwani index was negative (regressive) for out of pocket payments among both rural and urban households (-0.168 in 2001 to -0.197 to 2010, and 0.104 in 2001 to 0.156 in 2010, respectively), it but did not follow a regular trend during the study period. On the other hand, the Kakwani index was positive (progressive) for health insurance premium payments in rural areas (0.065 in 2001 to 0.095 in 2010). In urban areas, this index was negative for health insurance between 2001 and 2006 (-0.04 and -0.004), respectively), but positive between 2007 and 2010 (0.003 and 0.016, respectively). The dominance test (T-test) showed the concentration curves of out of pocket payments in both areas dominated the Lorenz curve in all years, but the dominance test (T-test) for health insurance premium payments did not follow a regular trend during the study period.Conclusions:
Due to the negativity of the Kakwani index for out-of-pocket payments, a great burden on the households can be predicted, and the progressivity of health insurance premium payments implies that expanding insurance coverage may lead to more equitable financing. Thus, the government should take the responsibility to expand the service and cost coverage of insurance plans and to develop policies that protect poor people.Keywords
Health care Financing Equity Vertical Equity Kakwani Index Iran
1. Background
Financing is one of the main functions of health systems and has an important effect on its three goals, particularly fairness in financial contributions and the assurance of all individuals’ access to health services (1). Without an appropriate finance system, only a limited number of individuals would have timely access to health services. In fact, financing a health system determines whether individuals can purchase the services, or whether the services are available when they are needed (2). In general, different countries make use of four methods for financing their health systems: tax-based systems, out-of-pocket payments, social health insurance, and private insurance programs (3). These methods have various effects on the functional indices of the health system, such as equity. Therefore, during the final decades of the 20th century, health researchers came to see the necessity of introducing and using new instruments to assess and investigate equity in health care financing (4). Gottschalk, Cantor, and Hurst et al. (5-7) each presented methods for evaluating equity in financing, but none of them showed the progressive or regressive nature of financing approaches. In his regular review of the various indices introduced for the assessment of the progressive or regressive nature of the tax, Lambert (1993) (8) came to the conclusion that only the Kakwani index was appropriate for use in the health care field. The Kakwani index reveals how distant a financing source is from the proportional status. This index ranges from -2 to 1; the use of negative positive positive and zero show regressively, progressivity, and proportionality, respectively. The progressivity (regressively) of the financing source shows the increase (decrease) in the proportion of the individuals’ payment for health services by the increase in their income (9).On average, almost 6% of the world’s GDP is spent on health care, and per capita of health expenditure in Iran is higher than that of north African and eastern Mediterranean countries (10). Based on Iran’s national health accounts (NHA) reports, Iran’s health care system is mainly financed through general health insurance payments, the government’s budget, individuals’ out of pocket expenses, and public taxes. According to the NHA, the burden of health system financing in Iran has transferred in recent years from the public to the private sector; most of this has been achieved through out of pocket payments. Between 1998 and 2001, the contributions by the public sector decreased from 52% to 38%, while those from the private sector increased from 48% to 60%. In addition, considering the lack of development in private insurance, most of the expenditures were paid for out of pocket (11-13). Other regional studies in various provinces of the country have revealed households’ exposure to catastrophic health expenditures (14-17). In Iran, policies, such as section 90 of the 4th development plan, increase of the health sector’s share of the GDP, and expand urban inpatient insurance, and rural insurance has been proposed to achieve equal financing.
2. Objectives
The present study aims to evaluate the equity of two financing resources of out of pocket payments and insurance premiums in households’ budgets, using the Kakwani index from 2001 to 2010.
3. Materials and Methods
The present study was performed using the data from the annual household expenditure and income survey conducted by the Iranian statistics center. Although the survey’s primary purpose is to show household expenditure patterns, the measures collected have the potential for equity analysis in health care financing. The statistical unit of this study includes one household living in an urban or rural area of the country between the years 2001 and 2010.
3.1. Data Analysis
3.1.1. Equality or Inequity of Income
Income equality or inequality (the Gini coefficient) is computed with reference to the Lorenz curve, which plots the cumulative proportion of the population, ranked by income, on its x-axis, against plots of the cumulative share of total income earned by population on its y-axis. The Gini coefficient is twice the area between the 45-degree line (the line of equality) and the Lorenz curve. In cases of perfect income equality or perfect income inequality, the Gini coefficient is 0 or 1, respectively. In our study, the Gini coefficient is calculated using Brown’s Equation, as as follows:
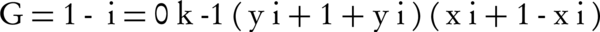
Where yi is the ith decile's income, yi+1 is the (i+1) th decile's income, xi is the number of the households in the ith decile, and xi+1 is the number of the households in the (i+1)th decile (18).
3.1.2. Equality or Inequality of Pay for Health Care (Concentration Index)
The concentration curve, which plots the cumulative share of what is paid for health care on its y-axis, against the cumulative proportion of the population, ranked by income, on its x-axis, can be used to identify whether socioeconomic inequality in health variables exists. However, the concentration curve does not give a measure of the magnitude of inequality in health variables. The concentration index, which is calculated with reference to the concentration curve, is twice the area between the concentration curve and the 45-degree line (the perfect equality line). In the case of no inequality in the health variables, the concentration index is zero. If the concentration curve lies below the line of equality, indicating a disproportionate concentration of the health variable among the rich, the index is positive. If the concentration curve lies above the 45-degreeline, demonstrating that the health variable is concentrated on the poor, the index is negative (19). In our study, inequality in health care payments (the concentration index) is calculated using the following Equation:

Where P is the cumulative percentage of population in the income decile and L is the cumulative percentage of healthcare payments in each decile (9).
3.1.3. The Kakwani Progressivity Index
The Kakwani progressivity index (KPI) is computed by subtracting the Gini coefficient from the concentration index (9).
KPI = CI - GI
The Kakwani progressivity index for health care payments is defined as twice the area between the Lorenz curve of income distribution and the concentration curve of the health care payments. The concentration curve of health care payments is above the Lorenz curve of income if richer individuals pay proportionally less of their income in health care payments than do poorer individuals, so that the health care financing system is regressive. Conversely, if health care financing is progressive, the concentration curves below the Lorenz curve. The range of Kakwani progressivity index is from +1, denoting the highest degree of progressivity, to -2, reflecting the highest possible degree of regressively. A value of zero for the Kakwani progressivity index would indicate that health care payments were proportional to income (20).
3.1.4. Dominance Test (T-test)
In order to test the dominance of the concentration curves or the Lorenz curve, the distribution free techniques of statistical inference were used. More information about this technique can be found in other articles (21-25).
The following Equation was was used in the present study:
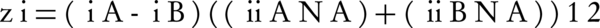
Where indicates cumulative proportions of income in each decile, indicates cumulative proportions of out-of-pocket payments or health insurance premium payments, indicates the variance of the cumulative proportion of income of each decile, and is the variance of out-of-pocket payments or health insurance premium payments of each decile. In addition, N shows the sample size of each year (21-25). Calculating Z, there would be four possible situations. These four situations are shown in Table 1. The critical value for Z is 2.02. The largest positive and negative values of Z were considered and compared with the critical value which is accepted from Cisse (24).
Testing for Stochastic Dominance Between Lorenz and Concentration Curves
| Z+ Significant | Z+ Not Significant | |
|---|---|---|
| Z- Significant | The two curves cross | B dominates A (the reference) |
| Z- Not Significant | A dominates (the reference) B | The two curves are equal |
4. Results
In this section, we present the estimated Gini coefficient for income, concentration index for health expenditure, and the Kakwani index for (i) health insurance premium payments, (ii) out of pocket payments, and (iii) the total household health expenditures ((i)+(ii)=(iii). Our results showed that the proportion of health expenditures to household income for urban and rural households was, respectively, 8% and 7% in 2001, 9% and 8% in 2006, and 11% and 10% in 2010. Further, in 2001, this proportion was 16% for first-decile urban and rural households, while it was 6% and 4% for 10th-decile urban and rural households, respectively (Table 2).
Proportion of Health Expenditures to Earned Incomes in the 1st and 10th Deciles in Rural and Urban Areas
| Proportion of Health Expenditures, % | 2001 | 2006 | 2010 |
|---|---|---|---|
| First decile | |||
| Rural | 0.16 | 0.2 | 0.26 |
| Urban | 0.16 | 0.24 | 0.28 |
| Tenth decile | |||
| Rural | 0.04 | 0.07 | 0.08 |
| Urban | 0.06 | 0.07 | 0.09 |
| All deciles | |||
| Rural | 0.07 | 0.08 | 0.10 |
| Urban | 0.08 | 0.09 | 0.11 |
During the study period, the Gini coefficient of income distribution for both rural and urban households had a decreasing trend (Table 3). Furthermore, the concentration index was positive for out of pocket payments in both rural and urban areas between 2001 and 2010. Although the changing trend of the concentration index was positive, it was descending and got closer to zero. The concentration index was positive for health insurance premium payments in both urban and rural areas, and the concentration of the payments was higher among the higher deciles, yet it did not follow a regular trend (Table 3).
The Trend of Changes in the Gini Coefficient, Concentration Index, and Kakwani Index for Out-of-Pocket Payments and Insurance Premiums Among Urban and Rural Households, 2001 - 2010
| The Trend of Changes | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 |
|---|---|---|---|---|---|---|---|---|---|---|
| Gini coefficient | ||||||||||
| Rural | 0.424 | 0.426 | 0.418 | 0.417 | 0.415 | 0.41 | 0.408 | 0.395 | 0.396 | 0.397 |
| Urban | 0.39 | 0.389 | 0.374 | 0.375 | 0.367 | 0.368 | 0.365 | 0.364 | 0.357 | 0.356 |
| Concentration index (out of pocket) | ||||||||||
| Rural | 0.256 | 0.248 | 0.247 | 0.24 | 0.236 | 0.233 | 0.23 | 0.228 | 0.22 | 0.2 |
| Urban | 0.286 | 0.282 | 0.27 | 0.268 | 0.267 | 0.26 | 0.245 | 0.233 | 0.222 | 0.2 |
| Concentration index (pealth insurance) | ||||||||||
| Rural | 0.489 | 0.468 | 0.453 | 0.438 | 0.48 | 0.475 | 0.48 | 0.485 | 0.486 | 0.49 |
| Urban | 0.35 | 0.348 | 0.34 | 0.363 | 0.365 | 0.364 | 0.368 | 0.374 | 0.37 | 0.372 |
| KPI (out-of-pocket) | ||||||||||
| Rural | -0.168 | -0.178 | -0.171 | -0.177 | -0.179 | -0.177 | -0.178 | -0.167 | -0.176 | -0.197 |
| Urban | -0.104 | -0.107 | -0.104 | -0.107 | -0.1 | -0.108 | -0.12 | -0.131 | -0.135 | -0.156 |
| KPI (health insurance) | ||||||||||
| Rural | 0.065 | 0.042 | 0.035 | 0.021 | 0.065 | 0.065 | 0.072 | 0.09 | 0.09 | 0.093 |
| Urban | -0.04 | -0.041 | -0.034 | -0.012 | -0.002 | -0.004 | 0.003 | 0.01 | 0.013 | 0.016 |
| KPI (total household health expenditures) | ||||||||||
| Rural | -0.142 | -0.138 | -0.152 | -0.144 | -0.154 | -0.142 | -0.121 | -0.126 | -0.113 | -0.120 |
| Urban | -0.113 | -0.094 | -0.095 | -0.089 | -0.082 | -0.078 | -0.081 | -0.092 | -0.097 | -0.098 |
The Kakwani index was negative for out of pocket payments among both rural and urban households and did not follow a regular trend during the study period. In addition, the Kakwani index was positive for health insurance premium payments in rural areas. In the urban areas, on the other hand, this index was negative between 2001 and 2006, but positive between 2006 and 2010; the Kakwani index for health insurance premium payments was closer to zero. On the other hand, the Kakwani index was more negative for out-of-pocket payments. The Kakwani index forth urban and rural households' total payments during the study period was negative, but it did not follow a regular trend. The dominance test showed the concentration curves of out-of-pocket payments in both areas, which dominated the Lorenz curve in all years studied. Except for 2006 and 2007, the concentration curves of health insurance premium payments in rural areas coincided with the Lorenz curve throughout the study period. In 2006 and 2007, the Lorenz curve dominated the concentration curves of health insurance premium payments. Except for 2010, the concentration curves of the health insurance premium payments in urban areas coincided with the Lorenz curve (Table 4).
Results of the Dominancy Tests
| Out of Pocket | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 |
|---|---|---|---|---|---|---|---|---|---|---|
| Rural | ||||||||||
| Z+ | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Z- | -40.10 | -34.68 | -32.5 | -25.84 | -24.32 | -33.23 | -34.48 | -34.48 | -39.25 | -28.48 |
| Urban | ||||||||||
| Z+ | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Z- | -20.2 | -19.66 | -18.95 | -19.51 | -15.15 | -10.84 | -14.04 | -30.21 | -33.53 | -15.24 |
| Health Insurance | ||||||||||
| Rural | ||||||||||
| Z+ | 25.83 | 19.44 | 7.07 | 16.99 | 25.57 | 9.6 | 5.73 | 9.4 | 12.08 | 22.73 |
| Z- | -15.50 | -11.11 | -18.86 | -21.84 | -12.78 | 0 | 0 | -3.13 | -6.04 | -4.55 |
| Urban | ||||||||||
| Z+ | 9.54 | 5.3 | 2.27 | 4.69 | 7.38 | 7.79 | 8.54 | 5.88 | 8.9 | 12.15 |
| Z- | -21.48 | -29.33 | -22.77 | -16.43 | -17.24 | -18.18 | -17.09 | -18.64 | -11.86 | 0 |
5. Discussion
The present study aimed to measure the equity of Iran’s health system financing in rural and urban areas between 2001 and 2010 using the Kakwani and concentration indexes. Since financing Iran’s health system is mainly based on out of pocket payments and social insurance (12, 13), the vertical equity of each of these financing methods was investigated as well. According to the results, the Gini coefficient had an average status in both urban and rural areas during the study period; of course, the index had a better status in the urban areas. The highest rates of inequity in the urban and rural areas occurred during 2001 and 2002, respectively. Nevertheless, since 2001 and up to 2010, a decrease was observed in income inequity among the population deciles. Hajizadeh’s study (1995 - 2000) and Moradi’s study (1997 - 2007) have also shown income inequity (25, 26). The concentration index was positive for out-of-pocket payments and social insurance premiums in both urban and rural areas, which shows their concentration among the households of higher income population deciles. At first glance, the positivity of the concentration index for out-of-pocket payments may represent a higher contribution by wealthier households to health payments and confirm the equity in the payments. Nonetheless, in Iran, where the health system is mainly financed through out-of-pocket payments when using healthcare services (12, 13), this index can represent the wealthy benefiting from the healthcare services. Thus, the lower deciles’ neglecting to use the healthcare services might have decreased their out-of-pocket payments and, eventually, resulted in the positivity of the concentration index. Moradi et al. (1997-2007) showed that the concentration of using healthcare services in Iran was among wealthier households (26). Furthermore, more the positivity of the concentration index of insurance premiums compared to that of the out-of-pocket payments may show the proportionality of the insurance premiums to the households’ incomes. On the other hand, it may represent the lack of insurance coverage among lower deciles’ households and, consequently, they are not paying insurance premiums. The Kakwani index was affected by income distribution (the Gini coefficient) and payment distribution (the concentration index). The total Kakwani index, including insurance premiums and out-of-pocket payments, was regressive during the study period, which means that the poor were spending a greater amount of their income on health care. However, this index for insurance premiums in the rural areas during the study period shows the progressivity of this financing resource. The progressivity of this financing resource has had a better trend in the rural areas since 2005. This might have resulted from the execution of a rural health insurance plan (2004) and, as the Gini coefficient showed, improvements in the income distribution in rural areas during the study period. Moreover, most of the lower income deciles’ villagers work in informal sectors of the economy and are covered by rural health insurance whose premiums arepaid by the government. The higher income deciles’ villagers, on the other hand, work in the formal sector of the economy, are covered by compulsory health insurance plans, and have to pay insurance premiums. The Kakwani index was negative for insurance premiums in urban areas between 2001 and 2005; this shows the regressively of this financing resource. Nevertheless, since the income distribution status improved during that time, this index became positive after 2006, and consequently, the distribution of insurance premium payments has become equal among urban income deciles. Urban dwellers usually work in the formal sectors of the economy and are covered by various insurances. Since the insurance premium is computed as a percentage of income (proportional) in the social security organization, and as per capita in the medical services insurance organization, which is quite regressive (27), the negativity of the index is quite natural unless income distribution is improved. The Kakwani index was positive for social insurance premiums in Iran from 1995 through 2000 (26). The Kakwani index was also positive for social insurance premiums in Thailand, Tanzania, Malaysia, Slovakia, and France, which might be due to provision of insurance coverage in the formal sector of those countries economiesand the inclusion of higher deciles’ members in the insurance plan (4, 28-31). On the other hand, social insurance premiums were regressive in Japan, Taiwan, South Korea, the Netherlands, and Germany (30, 31). The Kakwani index was negative for out-of-pocket payments in both areas during the study period, which shows the regressive nature of this financing resource. Although the concentration index was positive for out-of-pocket payments, the regressive nature of this financing resource may emphasize the fact that it is not only that the poor pay a higher amount of their income for the purchasing of healthcare services, but also that they benefit less from the health services. This apparently shows the injustice toward the poor since, on one hand, they pay a higher amount of their income for using healthcare services and, on the other hand, they may not actually make use of them. This results in worse health status among the lower deciles’ households, eventually leading to inequities in health status. Overall, this implies that the financial burden of the health system is mainly on lower income deciles’ shoulders. Other studies have also shown the regressive nature of out-of-pocket payments in most financing systems and that its financial burden is on the poor households’ shoulders (3, 32-34). The Kakwani index was reported negative for out-of-pocket payments in Iran between 1995 and 2000, and also 1997 - 2007. Also, it was shown that the individuals in higher income deciles paid for healthcare services eight times more than those in lower income deciles (26). The Kakwani index was reported negative for out-of-pocket payments in studies performed in Tanzania, Slovakia, the Ivory Coast, Guinea, Mali, and Senegal, where a lack of insurance coverage and richer groups’ paying less for healthcare services were considered the reasons for this situation (28, 29, 34). On the other hand, the Kakwani index was positive for out-of-pocket payments in Malaysia and Sri Lanka, resulting from the governments’ paying health subsidies to the lower deciles (31). Although regarding vertical equity, how the insurance premium is received in urban and rural areas is relatively appropriate, according to the NHA, with 50% of the total expenses of the health sector being paid out-of-pocket. In addition, more than 90% and less than 10% of the total private health expenditures are paid out-of-pocket and through insurance premiums, respectively (34). Thus, the proportion of out-of-pocket payments is quite high in the financing system. Based on these results, the financial burden of out-of-pocket payments is on low-income individuals’ shoulders. Therefore, the equity and distribution of the financial burden of out-of-pocket payments is much more important than the distribution of the financial burden of insurance premiums. Overall, it seems that vertical equity in health system financing has not been highly desirable. In fact, there are problems in both the insurance and financing systems of the health care sector, and the rate of out-of-pocket payments is quite high. Thus, the general policies in the health sector, and particularly regarding financing, should first aim at interventions and ways to reduce out-of-pocket payment for all households. Considering the regressive nature of the Kakwani index, low-income households should be supported through exemption plans. Further, in spite of the Iranian government’s efforts to implement universal coverage, it seems that its focus was just on coverage width, and less attention was paid to coverage height and depth. Therefore, revising the health insurance benefit package and the amount of the co-payments should be considered, as many necessary medical services are not covered by Iran’s current insurance plans and individuals are asked to directly at the time when the health service is provided. The financing system has many different aspects, and each of these has a different weight for the calculation of the Kakwani index as an index for equity in health financing. All of these aspects were not included in this study, so the Kakwani index was calculated without considering these weights.
Acknowledgements
References
-
1.
World Health Organization. The world health report 2000: health systems: improving performance. World Health Organization; 2000.
-
2.
World Health Organization. Increasing access to health workers in remote and rural areas through improved retention: global policy recommendations. World Health Organization; 2010.
-
3.
Gottret P, Schieber G. Health financing revisited: a practitioner's guide. Washington DC: World Bank; 2006.
-
4.
Kiss S, Kolman X, Filko M. Equity in health care finance in Slovakia–the impact of the reform. Rotterdam, Erasmus University; 2007.
-
5.
Gottschalk P, Wolfe B, Haveman R. Health care financing in the US, UK and Netherlands: Distributional consequences. University of Wisconsin-Madison, Institute for Research on Poverty; 1989.
-
6.
Cantor JC. The burden of financing health care in the United States. 1988.
-
7.
Hurst SL, Miller DM, Muzio JC. Spectral techniques in digital logic: Academic Press. Inc., 24–28 Oval Road, London NW1 7DX and Orlando, FL 32887, 1985, xv+ 314 pp., ISBN 0-12-362680-3. Signal Processing. 1985;9(2):138.
-
8.
Lambert PJ, Aronson JR. Inequality Decomposition Analysis and the Gini Coefficient Revisited. The Economic Journal. 1993;103(420):1221. https://doi.org/10.2307/2234247.
-
9.
O'Donnell OA, Wagstaff A. Analyzing health equity using household survey data: a guide to techniques and their implementation. World Bank Publications; 2008.
-
10.
Maher A, ahmadi AM, shokri JA. Survey of different approaches to health system financing in the selected countries during the period 1998-2004 and introducing new financing mechanisms for iran. Eco Res. 2008;8(1):149-55.
-
11.
Davari M, Haycox A, Walley T. Health care financing in iran; is privatization a good solution? Iran J Public Health. 2012;41(7):14-23. [PubMed ID: 23113205].
-
12.
Kermani MS, Ghaderi H, Yousefi A. Demand for medical care in the urban areas of Iran: an empirical investigation. Health Econ. 2008;17(7):849-62. [PubMed ID: 17990285]. https://doi.org/10.1002/hec.1308.
-
13.
World Health Organization. Health system profile, Islamic Republic of Iran. World health organization. 2006.
-
14.
Hanji MA, Fazayeli A. Equity of health care financing in Iran. Int J Soc Welf. 2005;5(19):279-300.
-
15.
Daneshkohan A, Karami M, Najafi F, Matin BK. Household catastrophic health expenditure. Iran J Public Health. 2011;40(1):94-9. [PubMed ID: 23113061].
-
16.
Kavosi Z, Rashidian A, Pourreza A, Majdzadeh R, Pourmalek F, Hosseinpour AR, et al. Inequality in household catastrophic health care expenditure in a low-income society of Iran. Health Policy Plan. 2012;27(7):613-23. [PubMed ID: 22279081]. https://doi.org/10.1093/heapol/czs001.
-
17.
Statistical Center of Iran. 2005.Records Complex-Household Expenditure and Income Survey in Urban and Rural Area.
-
18.
Giles DEA. Calculating a Standard Error for the Gini Coefficient: Some Further Results*. Oxford Bulletin of Economics and Statistics. 2004;66(3):425-33. https://doi.org/10.1111/j.1468-0084.2004.00086.x.
-
19.
Wagstaff A, O’Donnell O, van Doorslaer E. Quantitative techniques for health equity analysis. Washington, DC: World Bank publications; 2007.
-
20.
Bishop JA, Chow KV, Formby JP. Testing for Marginal Changes in Income Distributions with Lorenz and Concentration Curves. International Economic Review. 1994;35(2):479. https://doi.org/10.2307/2527065.
-
21.
Davidson R, Duclos JY. Statistical Inference for the Measurement of the Incidence of Taxes and Transfers. Econometrica. 1997;65(6):1453. https://doi.org/10.2307/2171744.
-
22.
Beach C, Davidson R. Distribution-Free Statistical Inference with Lorenz Curves and Income Shares. The Review of Economic Studies. 1983;50(4):723. https://doi.org/10.2307/2297772.
-
23.
Bishop JA, Chakraborti S, Thistle PD. Asymptotically Distribution-Free Statistical Inference for Generalized Lorenz Curves. Rev Econ Stat. 1989;71(4):725. https://doi.org/10.2307/1928121.
-
24.
Cisse B, Luchini S, Moatti JP. Progressivity and horizontal equity in health care finance and delivery: what about Africa? Health Policy. 2007;80(1):51-68. [PubMed ID: 16584803]. https://doi.org/10.1016/j.healthpol.2006.02.011.
-
25.
Hajizadeh M, Connelly LB. Equity of Health Care Financing in Iran: The Effect of Extending Health Insurance to the Uninsured. Oxford Development Studies. 2010;38(4):461-76. https://doi.org/10.1080/13600818.2010.524697.
-
26.
Moradi A. Estimation of the Inequality Concentration Index of Health Care Financing through Beta Lorenz Curve, the Case of Islamic Republic of Iran. 2010.
-
27.
Bishop JA, Formby JP, Zheng B. Inference tests for Gini-based tax progressivity indexes. J BUS ECON STAT. 1998;16(3):322-30.
-
28.
Borghi J, Ataguba J, Mtei G, Akazili J, Meheus F, Rehnberg C, et al. Methodological challenges in evaluating health care financing equity in data-poor contexts: lessons from Ghana, South Africa and Tanzania. Adv Health Econ Health Serv Res. 2008;21:133-56.
-
29.
Prakongsai P, Limwattananon S, Tangcharoensathien V. The equity impact of the universal coverage policy: lessons from Thailand. Adv Health Econ Health Serv Res. 2009;21:57-81. https://doi.org/10.1108/s0731-2199(2009)0000021006.
-
30.
Wagstaff A, van Doorslaer E, van der Burg H, Calonge S, Christiansen T, Citoni G, et al. Equity in the finance of health care: some further international comparisons. Journal of Health Economics. 1999;18(3):263-90. https://doi.org/10.1016/s0167-6296(98)00044-7.
-
31.
Yu C, Whynes DK, Sach TH. Equity in health care financing: The case of Malaysia. International Journal for Equity in Health. 2008;7(1):15. https://doi.org/10.1186/1475-9276-7-15.
-
32.
Smith S, Normand C. Analysing equity in health care financing: a flow of funds approach. Soc Sci Med. 2009;69(3):379-86. [PubMed ID: 19540030]. https://doi.org/10.1016/j.socscimed.2009.05.030.
-
33.
Balarajan Y, Selvaraj S, Subramanian SV. Health care and equity in India. The Lancet. 2011;377(9764):505-15. https://doi.org/10.1016/s0140-6736(10)61894-6.
-
34.
Kazemian M. Iran's National Health Accounts: Years 1971-2001, Analytical Framework and Methodological Issues. Malaysian Journal of Public Health Medicine. 2005;5(2):149-65.