Abstract
Context:
In many healthcare systems, the quality of the healthcare delivered is monitored using a number of “indicators.” In the present review, we investigate studies that address issues with the care delivered by healthcare providers. To do this, we employ indicators of the quality of those healthcare services.Evidence Acquisition:
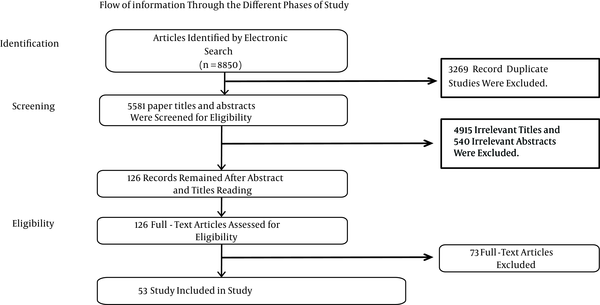
The studies for the review were identified by searching a number of electronic databases, including Cochrane Library, PubMed, Scopus, Ovid (Medline), the Social Sciences Citation Index, SID (Scientific Information Database, or Persian database), and Iran Medex (Persian database). Of 8,850 studies published between January 1971 and May 2015, 53 met the study criteria and were reviewed. In this study, the following key words were searched, both alone and in combination: health, healthcare, health care, provider*, effectiveness, quality, clinical outcome, patient satisfaction, and quality of life. We also considered healthcare quality indicators such as “clinical outcome,” “patient satisfaction,” and “quality of life” for our assessment of the quality of healthcare providers.Results:
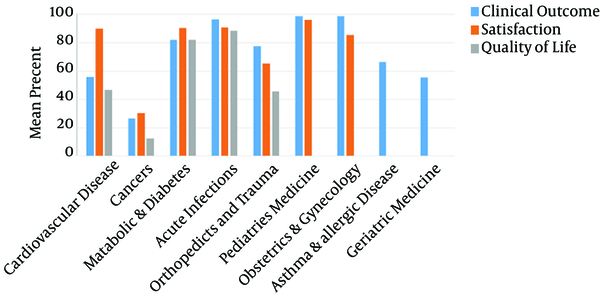
Of the 53 papers selected, 18 assessed the quality of care provided for cardiovascular disorders, 12 studied cancer conditions, eight dealt with metabolic disorders and diabetes, six focused on acute infection, three assessed orthopedics and trauma conditions, two studied pediatric conditions, two assessed obstetrics and gynecology conditions, one dealt with asthma and allergic disease conditions, and one assessed geriatric conditions. In our assessment of improvements in healthcare providers’ performance based on healthcare quality indicators, improvements in clinical outcomes ranged from 26.6% for cancer conditions to 98.8% for pediatric and gynecological conditions. An acceptable level of patient satisfaction was achieved in the range of 30.2% for cancer conditions to 96.0% for pediatric conditions, while improvements to quality of life ranged from 12.5% for cancer conditions to 88.7% for acute infection.Conclusions:
Taking account of three indicators for assessing the quality of healthcare providers (clinical outcome, patient satisfaction, and quality of life), the highest improvement levels among providers were observed for pediatric and gynecological conditions, and the lowest improvement levels were found for cancer conditions.Keywords
1. Context
Currently, one of the main problems with public policies and healthcare assessment is the lack of valid information on the performance and quality of healthcare service provision (1). The most pressing consequence of this problem is that there is little reliable information available on the quality of healthcare providers, but such information is needed to guide public and individual choices (1, 2). Thus, improving competition and efficiency in the area of healthcare is a focal issue in current reforms to medical financing and health plan choices (3). Although these reforms are clearly influenced by cost and clinical expenses, quality is increasingly a matter for concern (4). Using performance indicators and assessing outcomes are among the methods that can be used to measure and monitor the quality of care and service provision (5-8); also, developing and reporting indicators have led to quality improvements in many countries. A number of studies focus on the design and implementation of such indicators in healthcare systems (6, 9-14). There are many reasons for the problem of qualitative information. First, measurement and evaluation are problematic because the collection of relevant information (often based on the long-term outcome of the patient) is difficult for health service providers. Second, even if the information is relevant and appropriate, its multidimensional nature leads to other issues (15, 16). Specifically, clinical care quality encompasses a number of different outcomes, including service and care processing, and all of these factors are involved in quality assessment (17). The third obstacle in assessing the quality of healthcare is the limited number of patients for studies and the effects of a large number of factors other than provider quality on measuring the quality of the health services delivered by any one provider (17). Last, orientation and prejudice are issues that may change how patients are treated and, in turn, may affect healthcare providers’ results. Typically, trends are the result of systematic differences between patients (18). All of these issues have constrained the value of explicit information in relation to quality of healthcare, particularly significant health outcomes (18-20). Unfortunately there is no published study available that assesses the state of the quality of healthcare providers’ performance, because no globally confirmed indicators have been defined for evaluating healthcare providers’ performance (21). In fact, it seems that the best way to assess providers’ performance is to investigate the effects of their healthcare services on clinical outcomes and patients’ satisfaction with the services (22). In this regard, each country has tried to design and implement indicators that correspond to its own conditions. Evidently, drawing on the experience and indicators used by other countries is helpful in meeting the above goal, and in this sense, a summary of all published indicators may be very helpful. It is evident that using the indicators developed by other countries and their experiences of those indicators will help us to implement our objectives here. To facilitate this, the current paper will contain a list of the indicators published in other countries. In this systematic review, we describe all studies relating to issues with providers’ delivery of quality healthcare by employing indicators of the quality of healthcare services.
2. Evidence Acquisition
2.1. Study Population and Data Collection
Systematic review procedures have already been considered and published in the international protocol (Prospero). The studies were identified via a search of numerous electronic databases, including Cochrane Library, PubMed, Scopus, Ovid (Medline), the Social Sciences Citation Index, SID (scientific information database, or Persian database), and Iran Medex (Persian database). Information was also obtained by scanning reference lists for the articles included, and through consultations with experts in the field.
Our sample was based on data from January 1971 to May 2015. Only manuscripts in English and Persian with available full texts were reviewed. The reviewed articles included cross-sectional, descriptive, qualitative, and systematic review studies. Conference presentations, case reports, and intervention studies were excluded from the review process.
The key words searched individually and in combination included the following: health, healthcare, health care, provider, effectiveness, quality, clinical outcome, patient satisfaction, and quality of life.
The articles were evaluated by two reviewers based on the STROBE checklist (23), the CASP checklist for qualitative studies (24), and the PRISMA checklist (25). Also, the Cochrane risk of bias assessment tool was used to evaluate the risk of bias associated with individual studies (26).
The following data were extracted from each article: the country, the conditions studied, the study design and sample descriptions (patients and general physicians), the date of data collection, the measured criteria, and the standards used to judge the quality and results. Along with the reviewer, two referees independently examined the identified studies and articles based on the article title and abstract in terms of the qualification and eligibility of each paper. Selected full-text articles were reviewed and evaluated independently by the two referees. The population providing healthcare services was regarded as the main criterion, with no restrictions on the category of service provider job (for example, doctors, nurses, etc.), the level of services provided (for example, primary care or hospital care), or the target population for those services. In this study, a meta-analysis was not possible due to inconsistencies in the results of previous studies and their different methodologies. Hence, the scholars had to calculate the mean score of improvements statistically and present them in descriptive terms. Of the 8,850 articles identified by the abovementioned key words, 53 studies met the study criteria and were reviewed (Figure 1).
Flow Diagram of the Data Search
2.2. Criteria for Quality and Safety of Healthcare Providers
According to the primary review and the content analysis of the results, the quality of healthcare was evaluated based on three criteria (27-31). The first is “patient satisfaction,” which refers to the relationship between a physician or another healthcare professional and a patient. This includes interpersonal processes such as the provision of information and emotional support, and the involvement of patients in making decisions based on their preferences (29). The second criterion is “clinical outcomes,” which refers to a patient’s health status or a change in a patient’s health status, such as an improvement in symptoms or mobility resulting from medical care received. This includes both intended outcomes such as the relief of pain, and unintended outcomes such as mortality or other complications (5). The third criterion is “quality of life,” which refers to a patient’s health-related quality of life as assessed using various tools. Thus, patients’ satisfaction with healthcare services, observed improvements in their clinical outcomes as recorded in hospital files, and evaluation of their quality of life (if available) were included in the sources of data collected (32).
3. Results
Since we were unable to find studies titled “quality of healthcare provider performance,” we had to take “healthcare quality” indicators into account as an assessment of healthcare performance quality. These indicators are described in the method section. The improvements in the indicators in terms of patient satisfaction, health outcomes, and quality of life were considered the end points for measuring the quality of healthcare performance. Concerning the composition of papers according to the studied conditions, of the 53 study papers, 18 evaluated the quality of care provided for cardiovascular disorders (33-50) and 12 evaluated cancer conditions (51-62). Eight assessed metabolic disorders and diabetes (63-70), six assessed acute infections (71-76), three assessed orthopedic and trauma conditions (77-79), two assessed pediatric conditions (80, 81), two assessed obstetric and gynecological conditions (82, 83), one assessed asthma and allergic diseases (84), and one assessed geriatric conditions (85). The majority of the studies (51 in 53 articles) were carried out in high-income countries. Also, 32 of the papers were published in the United States. Twenty seven of the articles (51.0%) were simple and descriptive, 17 were cross-sectional studies (32.0%), three were systematic reviews (5.7%), and six were qualitative studies (11.3%). With regard to the strategy employed in the studies, 28 (52.8%) followed random sampling, and in 25 (47.2%), sampling was based on the self-selection method. Regarding the number of procedures reviewed, seven papers had less than 50 (13.2%), 14 papers had between 50 and 100 (26.4%), 26 had between 101 and 500 (49.1%), and only six had more than 500 (11.3%). The major indicators of healthcare quality were patients’ level of satisfaction in 11 papers (20.8%), improvements observed in clinical outcomes in 53 papers (100%), and patients’ quality of life in nine papers (17.0%). The assessment of improvements in healthcare providers’ performance (based on healthcare quality) (Table 1) indicated that improvements in clinical outcomes ranged from 26.6% in cancer conditions to 98.8% in both pediatric and gynecological conditions, and an acceptable level of patient satisfaction was achieved in the range of 30.2% for cancer conditions to 96.0% for pediatric conditions. Also, improvements in quality of life ranged from 12.5% for cancer conditions to 88.7% for acute infections.
Improvements in Healthcare Provider Performance (Based on Healthcare Quality)
| Condition Studied/Number of Subgroups | Criterion | Rate of Improvement, % | Number of Studies |
|---|---|---|---|
| Cardiovascular disease | 18 | ||
| 18 | Clinical outcome | 55.9 | |
| 4 | Satisfaction | 89.9 | |
| 4 | Quality of life | 46.6 | |
| Cancers | 12 | ||
| 12 | Clinical outcome | 26.6 | |
| 2 | Satisfaction | 30.2 | |
| 2 | Quality of life | 12.5 | |
| Metabolic diseases and diabetes | 8 | ||
| 8 | Clinical outcome | 82.2 | |
| 1 | Satisfaction | 90.5 | |
| 1 | Quality of life | 82.2 | |
| Acute infections | 6 | ||
| 6 | Clinical outcome | 96.6 | |
| 1 | Satisfaction | 90.8 | |
| 1 | Quality of life | 88.7 | |
| Orthopedics and trauma | 3 | ||
| 3 | Clinical outcome | 77.4 | |
| 1 | Satisfaction | 65.2 | |
| 1 | Quality of life | 45.6 | |
| Pediatric medicine | 2 | ||
| 2 | Clinical outcome | 98.8 | |
| 1 | Satisfaction | 96.0 | |
| Obstetrics and gynecology | 2 | ||
| 2 | Clinical outcome | 98.8 | |
| 1 | Satisfaction | 85.6 | |
| Asthma and allergic diseases | 1 | ||
| 1 | Clinical outcome | 66.5 | |
| Geriatric medicine | 1 | ||
| 1 | Clinical outcome | 55.6 |
According to the results, healthcare systems for obstetrics and gynecology and pediatric medicine show the highest rate of improvement in clinical outcomes with 98.8%, while acute infection stands in second place with 96.6%. By contrast, healthcare systems for cancer conditions show the minimum rate of improvement in clinical outcomes with a mean of 26.6%; this result may be attributable to a lack of definitive treatment methods for cancers. Clinical outcomes for metabolic diseases and diabetes, orthopedic conditions, trauma, asthma and allergic diseases, geriatric diseases, and cardiovascular diseases show the next highest rate of improvement, with 82.2%, 77.4%, 66.5%, 55.9%, 55.6%, and 26.6%, respectively. As well as clinical outcomes, patient satisfaction had the highest rate of improvement for pediatric medical healthcare, with a rate of 96%. Acute infections, metabolic conditions and diabetes, cardiovascular disease, obstetrics and gynecology, orthopedics and trauma, and cancers come next with 90.8%, 90.5%, 89.9%, 85.6%, 65.2%, and 30.2%, respectively. From the above results, it can be concluded that the clinical outcomes for obstetrics and gynecology, pediatric medicine, and acute infections are of the best quality compared to healthcare in other areas. By contrast, cancers have the lowest healthcare quality of all healthcare services (Figure 2).
Rates of Healthcare Quality in Different Healthcare Systems
4. Conclusions
Based on this review, there is no effective indicator for properly assessing healthcare providers’ performance and their role in improving the quality of healthcare services. Based on three different healthcare indicators, namely, clinical outcome, patient satisfaction, and patient quality of life, and taking account of patients’ statements and medical record descriptions, it was found that in most clinical conditions, proper healthcare services led to considerable improvements in patients’ outcomes, satisfaction, and quality of life. This was especially the case in some fields, such as pediatrics and gynecology. However, unfavorable outcomes were also found, and decreased satisfaction were an issue in some cases, for example, cancer. In general, we consider the abovementioned indicators to be the most relevant for assessing the quality of healthcare providers’ performance.
In any study or rating of the quality of healthcare provision, defining parameters to measure the quality of healthcare services is the main problem. The quality of healthcare providers’ services can be rated using several parameters. For example, Bailit et al. state that for obstetrics and gynecology, the risk-adjusted primary cesarean delivery rate is a good marker of maternal and neonatal outcomes (82). Also, there is a very important need for such information when it comes to planning public health policies, and Cardemil et al. (2012) showed that individuals planning community health worker assessments as part of community case management can use these results to make an informed choice of methods on the basis of their own objectives and the local context (80). This information can even be used by other countries to plan healthcare programs for the future, and Santana and Stelfox (2012) showed that their findings regarding the quality indicators used by trauma centers to measure performance could be useful for countries with similar systems of trauma care (79).
Schuster et al. (86) and Sawyer et al. (87) examined a large number of studies and concluded that only 50% of the patients had received advise on preventive care, while 70% had received the recommended acute disease care, and 20% had received the recommended acute contraindicated care. McGlynn et al. (88) and Min et al. (89) concluded that only 55% of their study participants received the recommended care, and in addition, many patients in their study did not receive high-quality healthcare; in other words, it seemed that many patients were not satisfied with the performance of their healthcare providers. In general, the close relationship between the quality of healthcare services and the performance of health service providers is undeniable (90). Studies indicate that when healthcare administrators, healthcare providers, patients, and parents cooperate collaboratively, healthcare quality and safety, as well as the patients’ and service providers’ satisfaction, increase, and costs are reduced (91). In addition, the main parties responsible for improvements in healthcare provider quality vary. A service provider may comprise an organization, a team, or simply an individual health worker (90). However, while all are ideally committed to the broad goals of a quality policy in a general system, their main concern is ensuring that the services they offer are of the highest possible standard and meet the needs of individual users, families, and the community. The results of improved quality in health service provision are not restricted merely to the providers of care or to health services (92).
Another point that should be considered in evaluating the role of healthcare providers is access to high-quality services. Interpersonal communication between service providers and customers is very effective in high-quality healthcare services. This type of communication is one of the most important components of improving customer satisfaction and compliance, and enhancing clinical outcomes (93). Patients who understand the nature of their own illness believe that their service provider is concerned about their health and are more satisfied with the services they receive. As a consequence, they are more likely to engage with the healthcare system. In this context, consideration of several factors, for example, effective interpersonal communication, is necessary (93).
It can be concluded that the greatest effect of improvements in healthcare service provision was observed in pediatrics and gynecology, while the least improvement was found in cancer conditions. In this regard, the results may be affected by some strong confounders such as the development status of the country, the suitability of the indicators used for assessing the quality of healthcare providers, the type of study, the number of procedures, and the time of the quality assessment. More importantly, the nature of clinical conditions can be a major factor affecting clinical outcomes, patient satisfaction, and patient quality of life Therefore, the naturally poor outcome with regard to cancer conditions explains a low satisfaction level with the related healthcare providers.
4.1. Study Limitations
This study was limited to articles published in English and Persian. Other restrictions include the number of databases searched and the limited number of indexes available on health and medical care quality. Thus, it is suggested that future studies be conducted using more databases, other languages, and possible also other indicators.
Acknowledgements
References
-
1.
Hakkinen U, Iversen T, Peltola M, Seppala TT, Malmivaara A, Belicza E, et al. Health care performance comparison using a disease-based approach: the EuroHOPE project. Health Policy. 2013;112(1-2):100-9. [PubMed ID: 23680074]. https://doi.org/10.1016/j.healthpol.2013.04.013.
-
2.
El-Hindawy MAM, Alamasi AMS. Measurement of the strategic performance of hospitality in the kingdom of saudi arabia: A balanced scorecard approach (BSC). Arab Eco Busi J. 2014;9(1):12-26. https://doi.org/10.1016/j.aebj.2013.02.001.
-
3.
Van der Wees PJ, Nijhuis-van der Sanden MW, van Ginneken E, Ayanian JZ, Schneider EC, Westert GP. Governing healthcare through performance measurement in Massachusetts and the Netherlands. Health Policy. 2014;116(1):18-26. [PubMed ID: 24138729]. https://doi.org/10.1016/j.healthpol.2013.09.009.
-
4.
Webber C, Brundage MD, Siemens DR, Groome PA. Quality of care indicators and their related outcomes: a population-based study in prostate cancer patients treated with radiotherapy. Radiother Oncol. 2013;107(3):358-65. [PubMed ID: 23722081]. https://doi.org/10.1016/j.radonc.2013.04.017.
-
5.
Mainz J. Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care. 2003;15(6):523-30. [PubMed ID: 14660535].
-
6.
Rubin HR, Pronovost P, Diette GB. From a process of care to a measure: the development and testing of a quality indicator. Int J Qual Health Care. 2001;13(6):489-96. [PubMed ID: 11769752].
-
7.
Tabrizi J, Saadati M, Sadeghi BH. Developmentofperformanceindicatorsforpatientand publicinvolvementin hospital:Expertconsensusrecommendations based on the available evidence. J Clin Res Gov. 2013;2:26-30.
-
8.
Janati A, Valizadeh S, Jafarabadi MA. Development of financial indicators of hospital performance. J clin res governance. 2014;3:92-8.
-
9.
Chiu WT, Yang CM, Lin HW, Chu TB. Development and implementation of a nationwide health care quality indicator system in Taiwan. Int J Qual Health Care. 2007;19(1):21-8. [PubMed ID: 17124255]. https://doi.org/10.1093/intqhc/mzl063.
-
10.
Gibberd R, Pathmeswaran A, Burtenshaw K. Using clinical indicators to identify areas for quality improvement. J Qual Clin Pract. 2000;20(4):136-44. [PubMed ID: 11207951].
-
11.
Holmes ACN, Judd FK, Yeatman R, Lloyd JH, Dakis J, Cairns F, et al. A 12-month follow up of the implementation of clinical indicators in a consultation–liaison service. Aust N Z J Psychiatry. 2001;35(2):236-9.
-
12.
Ballard DJ. Indicators to improve clinical quality across an integrated health care system. Int J Qual Health Care. 2003;15 Suppl 1:i13-23. [PubMed ID: 14660519].
-
13.
Brand C, Lam SK, Roberts C, Gorelik A, Amatya B, Smallwood D, et al. Measuring performance to drive improvement: development of a clinical indicator set for general medicine. Intern Med J. 2009;39(6):361-9. [PubMed ID: 19220555]. https://doi.org/10.1111/j.1445-5994.2009.01913.x.
-
14.
Anderson BG, Noyce JA. Clinical indicators and their role in quality management. Aust Clin Rev. 1992;12(1):15-21. [PubMed ID: 1586291].
-
15.
What is patient centre health care? A review of definitions and principles. London; 2007.
-
16.
Advancing the Practice of Patient and Family Centered Care, How to Get Started. Bethesda; 2008.
-
17.
Lown BA, Manning CF. The Schwartz Center Rounds: evaluation of an interdisciplinary approach to enhancing patient-centered communication, teamwork, and provider support. Acad Med. 2010;85(6):1073-81. [PubMed ID: 20505412]. https://doi.org/10.1097/ACM.0b013e3181dbf741.
-
18.
Shahian DM, Normand SL. Autonomy, beneficence, justice, and the limits of provider profiling. J Am Coll Cardiol. 2012;59(25):2383-6. [PubMed ID: 22698493]. https://doi.org/10.1016/j.jacc.2011.12.050.
-
19.
Lager A, Guldbrandsson K, Fossum B. The chance of Sweden's public health targets making a difference. Health Policy. 2007;80(3):413-21. [PubMed ID: 16750871]. https://doi.org/10.1016/j.healthpol.2006.05.005.
-
20.
van Herten LM, Gunning-Schepers LJ. Targets as a tool in health policy. Part I: Lessons learned. Health Policy. 2000;53(1):1-11. [PubMed ID: 10940459].
-
21.
Hussey PS, Mattke S, Morse L, Ridgely MS. Evaluation of the use of AHRQ and other quality indicators. Santa Monica, CA: AHRQ Publication; 2007.
-
22.
Prakash B. Patient satisfaction. J Cutan Aesthet Surg. 2010;3(3):151-5. [PubMed ID: 21430827]. https://doi.org/10.4103/0974-2077.74491.
-
23.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453-7. [PubMed ID: 18064739]. https://doi.org/10.1016/S0140-6736(07)61602-X.
-
24.
Critical appraisal skills programme (CASP). 2008. Available from: http://www.casp-uk.net/.
-
25.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):1-34. [PubMed ID: 19631507]. https://doi.org/10.1016/j.jclinepi.2009.06.006.
-
26.
Higgins JPT, Altman DG. Assessing risk of bias in included studies. 2008:187-241. https://doi.org/10.1002/9780470712184.ch8.
-
27.
Sadeghi-Bazargani H, Farhoudi M, Hajebrahimi S, Naghavi-Behzad M, Sohrabnavi Z, Azami-Aghdash S. A systematic review on clinical indicators, their types and codification processes. J Clin ResGovernance. 2014;4(1).
-
28.
Nerenz D, Neil. N. Performance measures for health care system. Commissioned paper for the center for health management research. 2001:1-38.
-
29.
Ha JF, Longnecker N. Doctor-patient communication: a review. Ochsner J. 2010;10(1):38-43. [PubMed ID: 21603354].
-
30.
Brook RH, McGlynn EA, Cleary PD. Quality of health care. Part 2: measuring quality of care. N Engl J Med. 1996;335(13):966-70. [PubMed ID: 8782507]. https://doi.org/10.1056/NEJM199609263351311.
-
31.
Donabedian A. Evaluating the quality of medical care. Milbank Mem Fund Q. 1966;44(3):Suppl:166-206. [PubMed ID: 5338568].
-
32.
Cella DF. Quality of life: concepts and definition. J Pain Symptom Manage. 1994;9(3):186-92. [PubMed ID: 8014530].
-
33.
Amsterdam EA, Peterson ED, Ou FS, Newby LK, Pollack CVJ, Gibler WB, et al. Comparative trends in guidelines adherence among patients with non-ST-segment elevation acute coronary syndromes treated with invasive versus conservative management strategies: Results from the CRUSADE quality improvement initiative. Am Heart J. 2009;158(5):748-54. [PubMed ID: 19853692]. https://doi.org/10.1016/j.ahj.2009.09.008.
-
34.
Duvernoy CS, Smith DE, Manohar P, Schaefer A, Kline-Rogers E, Share D, et al. Gender differences in adverse outcomes after contemporary percutaneous coronary intervention: an analysis from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2) percutaneous coronary intervention registry. Am Heart J. 2010;159(4):677-83. [PubMed ID: 20362729]. https://doi.org/10.1016/j.ahj.2009.12.040.
-
35.
Byrd JB, Vigen R, Plomondon ME, Rumsfeld JS, Box TL, Fihn SD, et al. Data quality of an electronic health record tool to support VA cardiac catheterization laboratory quality improvement: the VA Clinical Assessment, Reporting, and Tracking System for Cath Labs (CART) program. Am Heart J. 2013;165(3):434-40. [PubMed ID: 23453115]. https://doi.org/10.1016/j.ahj.2012.12.009.
-
36.
Cahalin LP, Myers J, Kaminsky L, Briggs P, Forman DE, Patel MJ, et al. Current trends in reducing cardiovascular risk factors in the United States: focus on worksite health and wellness. Prog Cardiovasc Dis. 2014;56(5):476-83. [PubMed ID: 24607011]. https://doi.org/10.1016/j.pcad.2013.10.002.
-
37.
Patterson ME, Hernandez AF, Hammill BG, Fonarow GC, Peterson ED, Schulman KA, et al. Process of care performance measures and long-term outcomes in patients hospitalized with heart failure. Med Care. 2010;48(3):210-6. [PubMed ID: 20125043]. https://doi.org/10.1097/MLR.0b013e3181ca3eb4.
-
38.
Dennison CR, Hughes S. Reforming cardiovascular care: quality measurement and improvement, and pay-for-performance. J Cardiovasc Nurs. 2009;24(5):341-3. [PubMed ID: 19707095]. https://doi.org/10.1097/JCN.0b013e3181b4346e.
-
39.
Bonow RO, Masoudi FA, Rumsfeld JS, Delong E, Estes NA, Goff DCJ, et al. ACC/AHA classification of care metrics: performance measures and quality metrics: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. J Am Coll Cardiol. 2008;52(24):2113-7. [PubMed ID: 19056002]. https://doi.org/10.1016/j.jacc.2008.10.014.
-
40.
Werner RM, Bradlow ET, Asch DA. Does hospital performance on process measures directly measure high quality care or is it a marker of unmeasured care? Health Serv Res. 2008;43(5 Pt 1):1464-84. [PubMed ID: 22568614]. https://doi.org/10.1111/j.1475-6773.2007.00817.x.
-
41.
Glickman SW, Schulman KA, Peterson ED, Hocker MB, Cairns CB. Evidence-based perspectives on pay for performance and quality of patient care and outcomes in emergency medicine. Ann Emerg Med. 2008;51(5):622-31. [PubMed ID: 18358566]. https://doi.org/10.1016/j.annemergmed.2008.01.010.
-
42.
Riba AL. Evidence-based performance and quality improvement in the acute cardiac care setting. Crit Care Clin. 2008;24(1):201-29. [PubMed ID: 18241786]. https://doi.org/10.1016/j.ccc.2007.09.002.
-
43.
Mehta RH, Peterson ED, Califf RM. Performance measures have a major effect on cardiovascular outcomes: a review. Am J Med. 2007;120(5):398-402. [PubMed ID: 17466646]. https://doi.org/10.1016/j.amjmed.2006.12.018.
-
44.
Bottle A, Sanders RD, Mozid A, Aylin P. Provider profiling models for acute coronary syndrome mortality using administrative data. Int J Cardiol. 2013;168(1):338-43. [PubMed ID: 23063211]. https://doi.org/10.1016/j.ijcard.2012.09.048.
-
45.
Osborne NH, Nicholas LH, Ghaferi AA, Upchurch GRJ, Dimick JB. Do popular media and internet-based hospital quality ratings identify hospitals with better cardiovascular surgery outcomes? J Am Coll Surg. 2010;210(1):87-92. [PubMed ID: 20123337]. https://doi.org/10.1016/j.jamcollsurg.2009.09.038.
-
46.
Wang Y, Lichtman JH, Dharmarajan K, Masoudi FA, Ross JS, Dodson JA, et al. National trends in stroke after acute myocardial infarction among Medicare patients in the United States: 1999 to 2010. Am Heart J. 2015;169(1):78-85. [PubMed ID: 25497251]. https://doi.org/10.1016/j.ahj.2014.06.011.
-
47.
Burden B, Taft E. A data-driven approach to improving clinical outcomes in cardiac care. J Healthc Qual. 1999;21(2):32-6. [PubMed ID: 10350983].
-
48.
Metcalfe M. Improving the safety of oxygen therapy in the treatment of acute myocardial infarctions. Int Emerg Nurs. 2012;20(2):94-7. [PubMed ID: 22483005]. https://doi.org/10.1016/j.ienj.2011.01.004.
-
49.
Mehta RH, Montoye CK, Faul J, Nagle DJ, Kure J, Raj E, et al. Enhancing quality of care for acute myocardial infarction: shifting the focus of improvement from key indicators to process of care and tool use: the American College of Cardiology Acute Myocardial Infarction Guidelines Applied in Practice Project in Michigan: Flint and Saginaw Expansion. J Am Coll Cardiol. 2004;43(12):2166-73. [PubMed ID: 15193675]. https://doi.org/10.1016/j.jacc.2003.08.067.
-
50.
Lau WL, Ix JH. Clinical detection, risk factors, and cardiovascular consequences of medial arterial calcification: a pattern of vascular injury associated with aberrant mineral metabolism. Semin Nephrol. 2013;33(2):93-105. [PubMed ID: 23465497]. https://doi.org/10.1016/j.semnephrol.2012.12.011.
-
51.
Sigurdardottir KR, Kaasa S, Rosland JH, Bausewein C, Radbruch L, Haugen DF, et al. The European Association for Palliative Care basic dataset to describe a palliative care cancer population: Results from an international Delphi process. Palliat Med. 2014;28(6):463-73. [PubMed ID: 24503559]. https://doi.org/10.1177/0269216314521264.
-
52.
Tota JE, Ramanakumar AV, Franco EL. Lung cancer screening: review and performance comparison under different risk scenarios. Lung. 2014;192(1):55-63. [PubMed ID: 24153450]. https://doi.org/10.1007/s00408-013-9517-x.
-
53.
Karanikolos M, Ellis L, Coleman MP, McKee M. Health systems performance and cancer outcomes. J Natl Cancer Inst Monogr. 2013;2013(46):7-12. [PubMed ID: 23962507]. https://doi.org/10.1093/jncimonographs/lgt003.
-
54.
Kanavos P, Schurer W. The dynamics of colorectal cancer management in 17 countries. Eur J Health Econ. 2010;10 Suppl 1:S115-29. [PubMed ID: 20012129]. https://doi.org/10.1007/s10198-009-0201-2.
-
55.
Vercelli M, Lillini R, Capocaccia R, Quaglia A, Socio-Economic I, Health Working G, et al. Use of SERTS (Socio-Economic, health Resources and Technologic Supplies) models to estimate cancer survival at provincial geographical level. Cancer Epidemiol. 2012;36(6):566-74. [PubMed ID: 22906484]. https://doi.org/10.1016/j.canep.2012.07.010.
-
56.
Parkes MW, Morrison KE, Bunch MJ, Hallstrom LK, Neudoerffer RC, Venema HD, et al. Towards integrated governance for water, health and social–ecological systems: The watershed governance prism. Glob Environ Chang. 2010;20(4):693-704. https://doi.org/10.1016/j.gloenvcha.2010.06.001.
-
57.
Aizer AA, Paly JJ, Efstathiou JA. Multidisciplinary care and management selection in prostate cancer. Semin Radiat Oncol. 2013;23(3):157-64. [PubMed ID: 23763881]. https://doi.org/10.1016/j.semradonc.2013.01.001.
-
58.
Hawley ST, Janz NK, Lillie SE, Friese CR, Griggs JJ, Graff JJ, et al. Perceptions of care coordination in a population-based sample of diverse breast cancer patients. Patient Educ Couns. 2010;81 Suppl:S34-40. [PubMed ID: 21074963]. https://doi.org/10.1016/j.pec.2010.08.009.
-
59.
Maliski SL, Connor SE, Oduro C, Litwin MS. Access to health care and quality of life for underserved men with prostate cancer. Semin Oncol Nurs. 2011;27(4):267-77. [PubMed ID: 22018406]. https://doi.org/10.1016/j.soncn.2011.07.005.
-
60.
Cheville AL, Basford JR, Troxel AB, Kornblith AB. Performance of common clinician- and self-report measures in assessing the function of community-dwelling people with metastatic breast cancer. Arch Phys Med Rehabil. 2009;90(12):2116-24. [PubMed ID: 19969178]. https://doi.org/10.1016/j.apmr.2009.06.020.
-
61.
Hanson LC. Improving access and quality of care for African Americans with advanced cancer. N C Med J. 2009;70(2):155-8. [PubMed ID: 19489376].
-
62.
Farmer P, Frenk J, Knaul FM, Shulman LN, Alleyne G, Armstrong L, et al. Expansion of cancer care and control in countries of low and middle income: a call to action. Lancet. 2010;376(9747):1186-93. [PubMed ID: 20709386]. https://doi.org/10.1016/S0140-6736(10)61152-X.
-
63.
Aron DC. Quality indicators and performance measures in diabetes care. Curr Diab Rep. 2014;14(3):472. [PubMed ID: 24496919]. https://doi.org/10.1007/s11892-013-0472-y.
-
64.
Shani M, Nakar S, Lustman A, Baievsky T, Rosenberg R, Vinker S. Patient characteristics correlated with quality indicator outcomes in diabetes care. Br J Gen Pract. 2010;60(578):655-9. [PubMed ID: 20849693]. https://doi.org/10.3399/bjgp10X515368.
-
65.
Nicolucci A, Greenfield S, Mattke S. Selecting indicators for the quality of diabetes care at the health systems level in OECD countries. Int J Qual Health Care. 2006;18 Suppl 1:26-30. [PubMed ID: 16954513]. https://doi.org/10.1093/intqhc/mzl023.
-
66.
Khadilkar A, Whitehead J, Taljaard M, Manuel D. Quality of diabetes care in the Canadian forces. Can J Diabetes. 2014;38(1):11-6. [PubMed ID: 24485207]. https://doi.org/10.1016/j.jcjd.2013.08.264.
-
67.
Calsbeek H, Ketelaar NA, Faber MJ, Wensing M, Braspenning J. Performance measurements in diabetes care: the complex task of selecting quality indicators. Int J Qual Health Care. 2013;25(6):704-9. [PubMed ID: 24150483]. https://doi.org/10.1093/intqhc/mzt073.
-
68.
Hirsch AG, Scheck McAlearney A. Measuring Diabetes Care Performance Using Electronic Health Record Data: The Impact of Diabetes Definitions on Performance Measure Outcomes. Am J Med Qual. 2014;29(4):292-9. [PubMed ID: 24006028]. https://doi.org/10.1177/1062860613500808.
-
69.
Boyle PJ, O'Neil KW, Berry CA, Stowell SA, Miller SC. Improving diabetes care and patient outcomes in skilled-care communities: successes and lessons from a quality improvement initiative. J Am Med Dir Assoc. 2013;14(5):340-4. [PubMed ID: 23291279]. https://doi.org/10.1016/j.jamda.2012.11.010.
-
70.
Govender I, Ehrlich R, Van Vuuren U, De Vries E, Namane M, De Sa A, et al. Clinical audit of diabetes management can improve the quality of care in a resource-limited primary care setting. Int J Qual Health Care. 2012;24(6):612-8. [PubMed ID: 23118094]. https://doi.org/10.1093/intqhc/mzs063.
-
71.
Nicolle LE. Infection prevention issues in long-term care. Curr Opin Infect Dis. 2014;27(4):363-9. [PubMed ID: 24921424]. https://doi.org/10.1097/QCO.0000000000000071.
-
72.
Elizabeth Wilcox M, Herridge MS. Clinical year in review III: mechanical ventilation, acute respiratory distress syndrome, nonpulmonary intensive care unit, and quality performance assessment metrics in your practice. Proc Am Thorac Soc. 2011;8(5):404-10. [PubMed ID: 21926390]. https://doi.org/10.1513/pats.201108-043TT.
-
73.
Linder JA, Kaleba EO, Kmetik KS. Using electronic health records to measure physician performance for acute conditions in primary care: empirical evaluation of the community-acquired pneumonia clinical quality measure set. Med Care. 2009;47(2):208-16. [PubMed ID: 19169122]. https://doi.org/10.1097/MLR.0b013e318189375f.
-
74.
Linder JA, Jung E, Housman D, Eskin MS, Schnipper JL, Middleton B, et al. The Acute Respiratory Infection Quality Dashboard: a performance measurement reporting tool in an electronic health record. AMIA Annu Symp Proc. 2007:1035. [PubMed ID: 18694133].
-
75.
Schulte B, Eickmeyer H, Heininger A, Juretzek S, Karrasch M, Denis O, et al. Detection of pneumonia associated pathogens using a prototype multiplexed pneumonia test in hospitalized patients with severe pneumonia. PLoS One. 2014;9(11):110566. [PubMed ID: 25397673]. https://doi.org/10.1371/journal.pone.0110566.
-
76.
Shin DW, Choi JE, Kim JH, Joo JS, Choi JY, Kang J, et al. What is the best practical survey method for the comparative assessment of palliative care services: results from a national quality assessment project in Korea. J Pain Symptom Manage. 2011;42(2):251-64. [PubMed ID: 21458215]. https://doi.org/10.1016/j.jpainsymman.2010.11.023.
-
77.
Moore L, Stelfox HT, Boutin A, Turgeon AF. Trauma center performance indicators for nonfatal outcomes: a scoping review of the literature. J Trauma Acute Care Surg. 2013;74(5):1331-43. [PubMed ID: 23609287]. https://doi.org/10.1097/TA.0b013e31828c4787.
-
78.
Moore L, Stelfox HT, Turgeon AF. Complication rates as a trauma care performance indicator: a systematic review. Crit Care. 2012;16(5):R195. [PubMed ID: 23072526]. https://doi.org/10.1186/cc11680.
-
79.
Santana MJ, Stelfox HT. Quality indicators used by trauma centers for performance measurement. J Trauma Acute Care Surg. 2012;72(5):1298-302. [PubMed ID: 22673258]. https://doi.org/10.1097/TA.0b013e318246584c.
-
80.
Cardemil CV, Gilroy KE, Callaghan-Koru JA, Nsona H, Bryce J. Comparison of methods for assessing quality of care for community case management of sick children: an application with community health workers in Malawi. Am J Trop Med Hyg. 2012;87(5 Suppl):127-36. [PubMed ID: 23136288]. https://doi.org/10.4269/ajtmh.2012.12-0389.
-
81.
Rowe AK, Osterholt DM, Kouame J, Piercefield E, Herman KM, Onikpo F, et al. Trends in health worker performance after implementing the Integrated Management of Childhood Illness strategy in Benin. Trop Med Int Health. 2012;17(4):438-46. [PubMed ID: 22950471]. https://doi.org/10.1111/j.1365-3156.2012.02976.x.
-
82.
Bailit JL, Love TE, Dawson NV. Quality of obstetric care and risk-adjusted primary cesarean delivery rates. Am J Obstet Gynecol. 2006;194(2):402-7. [PubMed ID: 16458637]. https://doi.org/10.1016/j.ajog.2005.07.045.
-
83.
Trojano GA. I365 surgical staging in non epithelial ovarian tumors, is it really necessary? Int J Gynaecol Obstet. 2012;119:S252. https://doi.org/10.1016/s0020-7292(12)60395-6.
-
84.
Okelo SO, Butz AM, Sharma R, Diette GB, Pitts SI, King TM, et al. Interventions to modify health care provider adherence to asthma guidelines: a systematic review. Pediatrics. 2013;132(3):517-34. [PubMed ID: 23979092]. https://doi.org/10.1542/peds.2013-0779.
-
85.
Boustani MA, Munger S, Gulati R, Vogel M, Beck RA, Callahan CM. Selecting a change and evaluating its impact on the performance of a complex adaptive health care delivery system. Clin Interv Aging. 2010;5:141-8. [PubMed ID: 20517483].
-
86.
Schuster MA, McGlynn EA, Brook RH. How good is the quality of health care in the United States? Milbank Q. 1998;76(4):517-63. [PubMed ID: 9879302].
-
87.
Sawyer SM, Ambresin AE, Bennett KE, Patton GC. A measurement framework for quality health care for adolescents in hospital. J Adolesc Health. 2014;55(4):484-90. [PubMed ID: 24698286]. https://doi.org/10.1016/j.jadohealth.2014.01.023.
-
88.
McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635-45. [PubMed ID: 12826639]. https://doi.org/10.1056/NEJMsa022615.
-
89.
Min L, Cryer H, Chan CL, Roth C, Tillou A. Quality of Care Delivered Before vs After a Quality-Improvement Intervention for Acute Geriatric Trauma. J Am Coll Surg. 2015;220(5):820-30. [PubMed ID: 25840534]. https://doi.org/10.1016/j.jamcollsurg.2014.12.041.
-
90.
Mayberry RM, Nicewander DA, Qin H, Ballard DJ. Improving quality and reducing inequities: a challenge in achieving best care. Proc (Bayl Univ Med Cent). 2006;19(2):103-18. [PubMed ID: 16609733].
-
91.
Reiling J, Hughes RG, Murphy MR. The Impact of Facility Design on Patient Safety. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD); 2008. [PubMed ID: 21328735].
-
92.
Bahadori M, Raadabadi M, Heidari Jamebozorgi M, Salesi M, Ravangard R. Measuring the quality of provided services for patients with chronic kidney disease. Nephrourol Mon. 2014;6(5):21810. [PubMed ID: 25695038]. https://doi.org/10.5812/numonthly.21810.
-
93.
Negri B, Brown DL, Hernandez O, Rosenbaum J, Roter D. Improving interpersonal communication between health care providers and clients. Bethesda US. 1997:3-59.