Dear Editor,
Primary central nervous system lymphoma (PCNSL) is a rare brain neoplasm with a very poor prognosis and limited treatment options (1). These malignant tumors include about 2% of all primary brain neoplasms (2). The treatment of choice in patients with PCNSL is systemic chemotherapy with high-dose methotrexate with or without whole-brain radiotherapy or intrathecal chemotherapy (3). Commonly, patients with PCNSL present with headache, seizure, vertigo, and mental/behavioral changes at the first visit (1). Focal neurological symptoms, cranial nerve palsy, cranial nerve symptoms, and neuropsychiatric symptoms are the other common presentations of PCNSL (1, 2). In this letter, we report a patient with large B-cell lymphoma, presenting with the manifestations of third nerve palsy.
A 29-year-old man referred with a headache, nausea/vomiting, diplopia, and left-sided ptosis two days before his admission to Namazi hospital affiliated to Shiraz University of Medical Sciences, Iran. He had a history of repeated nausea, vomiting, and weight loss for a year. The general physical examination was unremarkable, but he showed left-sided oculomotor nerve palsy in the neurological examination. The pupil size and reaction were normal. Other cranial nerves, mental status, sensorimotor and cerebellar functions, and meningeal signs were within normal limits.
Routine work-ups were unremarkable. Tumor markers were negative.
The laboratory tests for vasculitides were negative.
Anti-human immunodefeciency virus (HIV) antibody, HBs-antigen, and anti-hepatitis C virus (HCV) antibody were also negative. The serological assessment for the Epstein-Barr virus was negative, too. anti-acetylcholine receptor (anti-AchR) and anti-muscle specific kinase (anti-MuSK) antibodies were negative. The CSF analysis showed WBC 79/mm3 (polymorphonuclear 45% and lymphocyte 34%), glucose 20 mg/dL, protein 104 mg/dL, and LDH 90 U/L. The CSF culture and cytology were negative. Electromyography and repeated nerve stimulation tests were normal. Brain MRI showed a right-sided enhancing lesion adjacent to the pontine part of the fourth ventricle (Figure 1A), and thickening of the cisternal part of the left oculomotor nerve associated with contrast enhancement (Figure 1). Paranasal sinuses were normal in computerized tomography (CT). Brain CT angiography showed no aneurysm. Chest, abdominal, and pelvic CT scans were tumor-free. Ultimately, the patient was considered as a case of oculomotor neuroma and discharged with valproate, amitryptiline, and ondansetron.
A, Contrast-enhanced T1-images (TR/TE: 350-550/8.3-9.5 with 0.1 mmol/kg Gad) showing an enlarging lesion in the inferior aspect of the fourth ventricle in months 0; B and C, three; and D, five after developing third nerve palsy.
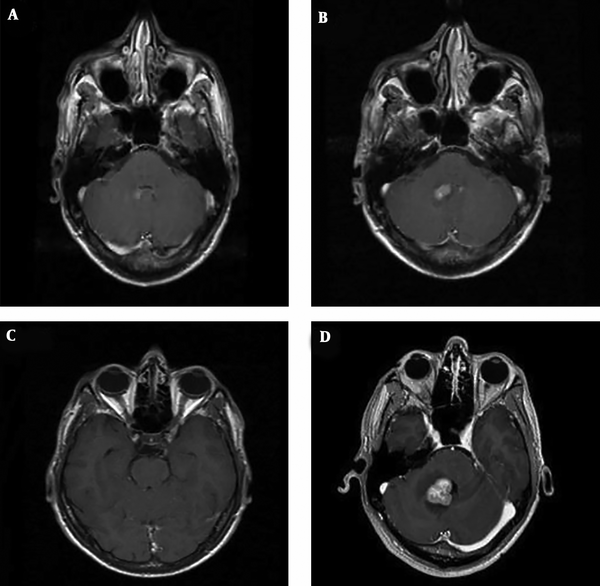
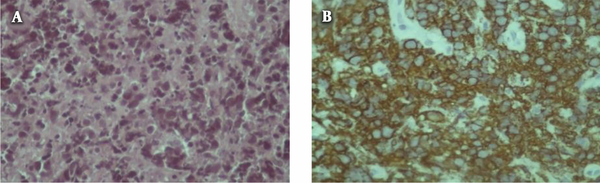
After discharge, he visited an infectious disease specialist and received rifampin, doxycycline, and prednisolone with the impression of Neuro-Brucellosis. His ptosis disappeared, but he developed vertigo three months later. He was re-admitted to the hospital due to refractory vertigo, headache, nausea, vomiting, and diplopia. New MRI revealed several new intraventricular enhancing nodules in the frontal horn of the left lateral ventricle and the superior aspect of the fourth ventricle. The previously mentioned right paraventricular lesions and left cisternal lesions were enlarged (Figure 1B and C). Another CSF study showed five cells (all lymphocyte), protein 81 mg/dL, glucose 4 mg/dL (concomitant blood sugar 119 mg/dL), lactate dehydrogenase 122 U/L, and lactate 65 mmol/L. The CSF polymerase chain reactions for tuberculosis and brucellosis were negative. Despite negative CSF cytology, carcinomatous meningitis was considered an ongoing diagnosis. A whole-body scan indicated two focal active bone lesions in the left frontal and right occipital bones, which were in favor of tumoral involvement. Two months later, the right-sided lesion adjacent to the fourth ventricle became large enough for MRI-guided stereotactic biopsy (Figure 1D). The biopsy showed CD20 positive atypical lymphoid cells indicating diffused large B-cell lymphoma (Figure 2A and B).
A, Infiltration of atypical lymphoid cells in the brain parenchyma (H & E, 40×); B, diffuse membranous and cytoplasmic positivity of infiltrating lymphocytes for CD20 (IHC, 40×)
Further investigations included CT of chest, abdomen, and pelvis, bone marrow aspiration, and biopsy, but the ophthalmic evaluation did not reveal lymphomatous involvement. After that, the patient received a combination of chemotherapy agents consisting of six 14-day cycles of R-MVP (rituximab, methotrexate, procarbazine, and vincristine). The patient completed all chemotherapy cycles without any major toxicity with complete resolution of symptoms. Since postchemotherapy brain MRI revealed partial response, the patient was sent for whole-brain radiotherapy, which showed the complete resolution of brain lesions. Then, the patient was sent to receive consolidation with high-dose chemotherapy, followed by autologous stem cell rescue.
Primary central nervous system lymphoma (PCNSL) is a rare form of non-Hodgkin lymphoma with a poor prognosis, which is confined to the CNS. Patients with PCNSL mostly complain of headaches, seizures, vertigo, and mental status changes. Focal neurological deficits, cranial nerve symptoms, and neuropsychiatric symptoms are the other presentations of PCNSL (1). Rarely, PCNSL presents systemic manifestations such as fever, weight loss, and night sweating. The most common lesion sites are deep gray nuclei, periventricular white matter, corpus callosum, and CSF spaces (4, 5). Less common sites include the brainstem, cranial nerves, cavernous sinuses, and pineal and pituitary glands. The pattern of the intracranial distribution of the lesion in our case was inconsistent with the tendency of PCNSL to involve basal ganglia and periventricular white matter. In this case, the lesion involved the intraventricular area of the fourth ventricle and the cisternal portion of the left third cranial nerve.
Oculomotor nerve palsy commonly occurs due to leptomeningeal lymphoma that compresses the oculomotor nerve. This nerve exits in the midbrain through the interpeduncular cistern. Irregular contrast enhancement in the interpeduncular cistern is evident in brain MRI of patients with oculomotor nerve compression. Although the involvement of cranial nerves and their leptomeninges is commonly reported in many cases, isolated oculomotor palsy is unusual as the initial presentation of PCNSL. There are only a few case reports of oculomotor nerve palsy as the presenting manifestation of lymphoma (6, 7). Taga et al. (8) considered some “red falgs” for suspecting to lymphoma as the cause of third nerve palsy. These red flags included young age, progressive course, good response to corticosteroids, and relapse after stopping corticosteroids. The definite diagnosis of PCNSL is based on the histopathological confirmation in the absence of systemic lymphoma. Prompt diagnosis and management of patients are required to improve the survival outcome of patients diagnosed with PCNSL. This case report reconfirms considering PCNSL in the differential diagnosis of third nerve palsy.
References
-
1.
Tan T, Rosa CSL, Han TF. Primary central nervous system lymphoma presenting as isolated oculomotor nerve palsy. Interdiscip Neurosurg. 2014;1(3):56-8. https://doi.org/10.1016/j.inat.2014.06.003.
-
2.
Bellinzona M, Roser F, Ostertag H, Gaab RM, Saini M. Surgical removal of primary central nervous system lymphomas (PCNSL) presenting as space occupying lesions: A series of 33 cases. Eur J Surg Oncol. 2005;31(1):100-5. [PubMed ID: 15642434]. https://doi.org/10.1016/j.ejso.2004.10.002.
-
3.
Grommes C, Rubenstein JL, DeAngelis LM, Ferreri AJM, Batchelor TT. Comprehensive approach to diagnosis and treatment of newly diagnosed primary CNS lymphoma. Neuro Oncol. 2019;21(3):296-305. [PubMed ID: 30418592]. [PubMed Central ID: PMC6380418]. https://doi.org/10.1093/neuonc/noy192.
-
4.
Mansour A, Qandeel M, Abdel-Razeq H, Abu Ali HA. MR imaging features of intracranial primary CNS lymphoma in immune competent patients. Cancer Imaging. 2014;14:22. [PubMed ID: 25608570]. [PubMed Central ID: PMC4331827]. https://doi.org/10.1186/1470-7330-14-22.
-
5.
Mohile NA, Abrey LE. Primary central nervous system lymphoma. Semin Radiat Oncol. 2007;17(3):223-9. [PubMed ID: 17591569]. https://doi.org/10.1016/j.semradonc.2007.02.008.
-
6.
Heckmann JG. Oculomotor nerve palsy and diffuse large B cell lymphoma. Acta Neurol Belg. 2017;117(3):743-4. [PubMed ID: 28220398]. https://doi.org/10.1007/s13760-017-0759-x.
-
7.
Tsai CH, Lee EJ, Liu YS, Chen YC, Shih YH, Chuang MT. Isolated oculomotor nerve palsy caused by diffuse large B cell lymphoma. Acta Neurol Belg. 2013;113(1):103-4. [PubMed ID: 22729834]. https://doi.org/10.1007/s13760-012-0100-7.
-
8.
Taga A, Russo M, Florindo I, Pavesi G. Isolated third cranial nerve palsy leading to the diagnosis of disseminated burkitt lymphoma: A CASE REPORT AND LITERATURE REVIEW. Neurologist. 2017;22(5):182-5. [PubMed ID: 28859023]. https://doi.org/10.1097/NRL.0000000000000130.