Abstract
Background:
Acute myeloid leukemia is a type of hematological malignancy. Chemotherapy is the first-line treatment for AML. The main aim of treatment is to achieve complete remission in patients. Although complete remission is achieved in most patients, still the rate of relapse remains high. Recent studies revealed that drug resistance is an important cause of treatment failure in AML patients. Autophagy as a conserved catabolic process has a significant role in drug resistance of AML. Autophagy can act as a chemo-resistance mechanism in response to chemotherapy in AML patients. However, the role of this pathway in response to treatment of AML patients is not yet fully clarified.Objectives:
The aim of this study was to investigate the effect of the BECN1 gene, as a key regulator of autophagy on remission and response to chemotherapy in AML patients.Methods:
The BECN1 gene expression was evaluated in 30 AML patients at diagnosis stage, on 18 patients with complete remission and 15 controls using qRT-PCR.Results:
The results showed that BECN1 gene expression level was significantly higher in AML patients than controls at the rate of 5/3 fold, P < 0.0001. We found that expression level of BECN1 was significantly reduced in patients with complete remission in comparison with newly diagnosed AML patients at the rate of 0.73 fold, P = 0.004.Conclusions:
Low expression of BECN1 gene might be associated to complete remission. Therefore, perhaps BECN1 gene can be used as a biomarker to assess remission status. Moreover, targeting BECN1 can be used as a potential strategy to improve treatment in AML patients.Keywords
1. Background
Acute myeloid leukemia (AML) is a hematological malignancy that is characterized by a clonal proliferation and differentiation arrest in myeloid progenitors. AML is the most common type of acute leukemia amongst adults (1, 2). Chemotherapy and bone marrow transplantation are used as effective therapies for AML patients. Chemotherapy consists of two phases: induction therapy and consolidation therapy. Patients receive a 7 + 3 standard regimen during induction therapy, which includes 3 days of an anthracycline (such as daunorubicin or idarubicin) and 7 days of cytarabine. This regimen is used for all subtypes of AML, except M3. All trans retinoic acid (ATRA) along with arsenic trioxide is commonly used for patients with AML-M3. The aim of this phase is to attain complete remission in patients. However, consolidation therapy is required to obtain permanent remission after the induction therapy (3, 4). Although most patients achieve complete remission (CR) after treatment, the rate of relapse is still high (5). Data have shown that drug resistance is one of the main causes of relapse in AML patients (6). Therefore, knowing the factors that affect chemotherapy response of AML patients can lead to progress in the treatment process.
Autophagy is known as a conserved catabolic process wherein the cytoplasmic components are packed in vesicles and degrade by lysosomes (7). In addition to being an essential protein for autophagy initiation and regulation, BECN1 also plays a significant role in apoptosis pathway (8). Autophagy has a double edged role in cancer, but its role in tumor initiation and development is still a controversy. Autophagy reduction can be linked to tumorigenesis. On the other hand, increased autophagy promotes tumor cell proliferation and survival in various stressors (9, 10).
The basal level of autophagy is low in the cells in normal circumstances, but it can be enhanced in response to starvation, oxidative stress, cytotoxic drugs, infections and DNA damage (11-13). Therefore, it can help cells to survive under adverse conditions. Several studies have shown that autophagy might be enhanced during chemotherapy, resulting in chemo-resistance in cancer cells. Moreover, autophagy activation by chemotherapy, decreases apoptosis and promotes survival in tumor cells (14-16). Thus, autophagy inhibition could be a therapeutic strategy in order to overcome chemo-resistance in cancers.
Impairment of autophagy might be involved in leukemia initiation and development. Autophagy can act as a chemo-resistance mechanism in response to chemotherapy in AML patients (17, 18). Recent studies have shown that inhibition of autophagy by genetic silencing or autophagy inhibitory drugs can lead to enhancement of cytarabine -induced cell death in AML cell lines (18, 19). However, the role of this pathway in response to treatment of AML patients is not yet fully clear.
2. Objectives
Given that autophagy can lead to chemo-resistance in AML patients, and the fact that drug resistance is one of the main causes of treatment failure in AML, the aim of this study was to investigate the effect of the BECN1 gene, as a key regulator of autophagy, on remission and response to chemotherapy in AML patients.
3. Methods
3.1. Samples and Patients
In this case-control study, whole blood samples were collected from 30 de novo AML patients at diagnosis stage. The patients were diagnosed according to FAB classification criteria and had not received any previous chemotherapy. We also used 15 healthy volunteers as control group that were matched with patients for age and gender, who did not have any hematological diseases. Patients received the following treatment protocol: induction therapy of 7 + 3 regimen (daunorubicin 45 mg/m2 on days 1 to 3 and cytarabine 100 - 200 mg/m2 on days 1 to 7) for all subtypes, except M3 and ATRA along with arsenic trioxide for M3 subtype. This study was approved by the local Ethics Committee of Shiraz University of Medical Sciences. After explaining the study objectives, written informed consent was obtained from all participants.
3.2. RNA Extraction and cDNA Synthesis
Total RNA was extracted from whole blood samples by TRIzol method (Invitrogen, Carlsbad, CA, USA) according to instructions. Subsequently, the concentration of the extracted RNAs were determined using NanoDrop instrument (Hellma, Denmark). Afterwards, 0.4 μg of RNA was transcribed into cDNA to a final volume of 10 μL, using Prime Script First Strand cDNA Synthesis kit (Takara, Shiga, Japan).
3.3. Quantitative Real-Time Polymerase Chain Reaction
Primers employed in this study were designed using AlleleID 7.0 and Gene Runner software. For BECN1 gene, the forward and reverse primer sequences were as follows: (5-TGGCACAATCAATAACTTC-3) and (5-GTAAGGAACAAGTCGGTAT-3), respectively. The β-actin primers were forward primer (5-ATCGTGCGTGACATTAAGGAG-3) and reverse primer (5-GAAGGAAGGCTGGAAGAGTG-3). B-actin was used as a reference gene and PCR normalization. Real time PCR was done using QIAGEN's real-time PCR cycler (Rotor gene, Germany) in order to quantify BECN1 gene expression. Each real-time PCR mixture consisted of 1 µL of cDNA, 10 µL of SYBR Green PCR Master Mix (SYBR Premix Ex TaqTMII, Tli RNaseH Plus Yektatajhiz, Iran) 8.2 µL of deionized water and 0.4 µL of each forward and reverse primer in a final reaction volume of 20 µL. The amplification profile was as follows: initial denaturation at 95˚C for 90 seconds followed by 40 cycles of subsequent denaturation at 95˚C for 5 seconds, annealing at 56˚C for 30 seconds and elongation at 72˚C for 30 seconds. The relative BECN1 mRNA expression (fold changes) in AML patients were calculated using 2-ΔΔCT method.
3.4. Statistical Analysis
Statistical analysis was performed using Graph pad Prism V. 8.0.2 software (Graph Pad Software Inc, San Diego, California, USA) and SPSS version 25.0 (SPSS IBM, Chicago, IL). N-fold changes were calculated, using the equation 2-ΔΔCT. BECN1 gene Expression was compared between each two groups using t-test. The correlation between BECN1 expression and clinical characteristics of patients was analyzed using the Pearson's correlation coefficient (r). P values < 0.05 were considered to be statistically significant.
4. Results
4.1. Analysis of BECN1 Gene Expression in AML Patients and Control Group
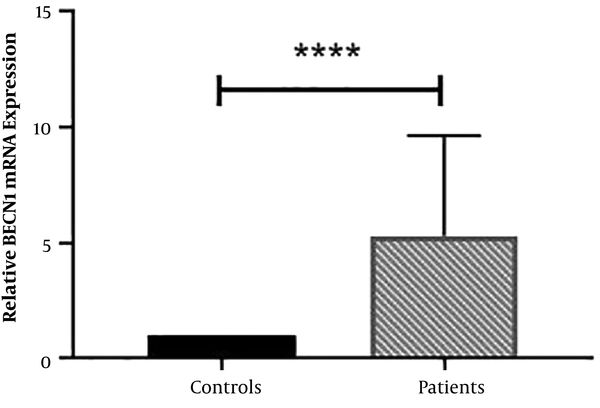
Expression of BECN1 gene in 30 newly diagnosed AML patients and 15 controls were evaluated and the results showed that BECN1 gene expression level was significantly higher in AML patients than controls at the rate of 5/3 fold (P < 0.0001). Fold changes of BECN1 mRNA expression in AML patients versus controls are shown in Figure 1.
Expression of BECN1 mRNA in newly diagnosed AML patients compared with controls. Fold changes of BECN1 mRNA expression was analyzed by using the equation 2-ΔΔCT (****, P < 0.0001).
4.2. The Correlation Between BECN1 Expression and Clinical Characteristics of Patients
Clinical characteristics of patients at diagnosis and complete remission phase are shown in Table 1. We evaluated BECN1 expression correlation with age, Hb, WBC count, PLT count and bone marrow blast percentage of patients. No significant differences were found between BECN1 expression in relation to age, Hb, PLT count and bone marrow blast (Tables 2 and 3). There was a positive and significant correlation between BECN1 expression and WBC count (r = 0.697, P < 0.0001) in newly diagnosed patients (Table 2). In fact, overexpression of BECN1 was associated with increased WBC count at diagnosis stage. However, we found no significant correlation between BECN1 expression and WBC count in patients with complete remission (Table 3).
Clinical Characteristics of AML Patients at Diagnosis and Complete Remission Phase
| Newly Diagnosed Patients | Patients with Complete Remission | |
|---|---|---|
| Sex, male/female | 14/16 | 8/10 |
| Age, median (range) | 52 (24 - 75) | 50 (24 - 75) |
| WBC (× 109/L), median (range) | 32.8 (0.5 - 166) | 2.6 (0.4 - 16.9) |
| PLT (× 109/L), median (range) | 65.8 (6 - 227) | 87.2 (8 - 230) |
| Hb (g/L), median (range) | 7.9 (4.4 - 11.2) | 8.3 (7.2 - 10.4) |
| BM blast %, median (range) | 73 (40 - 90) | < 5 (1 - 3) |
| Classification (AML M3/non-M3) | 5/25 | 3/15 |
Correlation Between BECN1 Expression Clinical Characteristics of Patients at Diagnosis Phase
| Parameters (BECN1) | r | P Value |
|---|---|---|
| Age | -0.041 | 0.82 |
| Sex | -0.064 | 0.72 |
| Hb | -0.046 | 0.8 |
| WBC count | 0.606** | < 0.0001**** |
| PLT count | -0.029 | 0.87 |
| Blast percentage | -0.005 | 0.98 |
Correlation Between BECN1 Expression Clinical Characteristics of Patients at Complete Remission Phase
| Parameters (BECN1) | r | P Value |
|---|---|---|
| Age | -0.307 | 0.21 |
| Sex | 0.054 | 0.83 |
| Hb | -0.312 | 0.22 |
| WBC count | -0.276 | 0.26 |
| PLT count | -0.187 | 0.18 |
4.3. BECN1 Gene Expression Level Was Significantly Lower in Patients with Complete Remission than Newly Diagnosed AML Patients
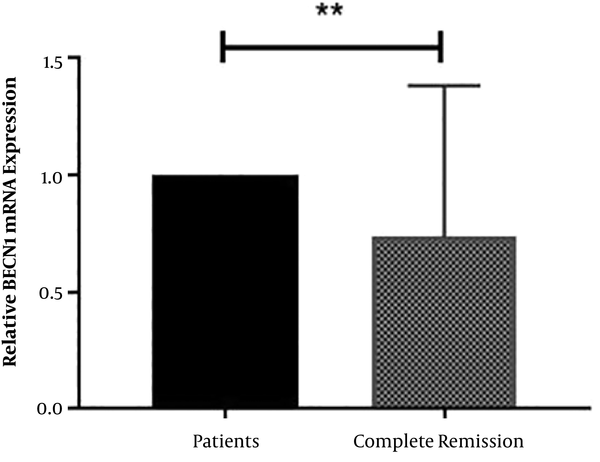
We investigated whether the expression of BECN1 was different in patients who achieved complete remission in comparison with newly diagnosed patients. After induction therapy, 18 patients achieved complete remission. Therefore, BECN1 gene expression was analyzed in 18 newly diagnosed patients and 18 patients with complete remission in the same cases. We found that the expression level of BECN1 was significantly reduced in patients with complete remission compared to newly diagnosed AML patients at a rate of 0.73 fold (P = 0.004). These results are shown in Figure 2.
The comparison of BECN1 mRNA expression in patients with complete remission compared to newly diagnosed AML patients. Results are given as fold change of BECN1 mRNA expression (**, P = 0.004).
5. Discussion
Chemotherapy is the first-line treatment of AML, and the aim is to achieve complete remission in patients. The rate of CR is 60% - 80% in young patient and 40% - 60% in elderly after standard induction therapy. However, > 85% of patients in response to chemotherapy fail and relapse rate is high (3, 5).
Recent studies have focused on drug resistance, which could be an important cause of treatment failure in AML patients. Some signaling pathways such as autophagy and PI3K/AKT are involved in drug resistance of AML (6, 20).
Autophagy is a conserved catabolic process, where damaged cellular components are degraded by lysosomes. BECN1 is an essential protein for autophagy initiation and regulation (7, 8). Several studies have proven that autophagy is induced during chemotherapy, and increased autophagy is associated with chemo-resistance in AML cells. Emerging data showed that autophagy inhibition by genetic silencing or autophagy inhibitory drugs has lead to increase in the cytotoxic effect of cytarabine in AML cell lines (17-19).
In this study, expression of BECN1 gene, as a major regulator of autophagy, was evaluated in AML patients at diagnosis and complete remission phase. The results revealed the significance of the BECN1 gene in pathogenesis, response to chemotherapy and remission of patients. Our results showed that BECN1 gene expression level was significantly higher (5.3 fold, P < 0.0001) in newly diagnosed AML patients than the control group (Figure 1) similar to a result in a study by Hu et al. that found expression level of BECN1 was higher in acute leukemia patients compared to normal controls (21). Thus, overexpression of BECN1 might be related to pathogenesis of AML. Keyvan et al. did not observe any significant difference in the expression of BECN1 between AML patients and control groups (22), which was probably due to differences in BECN1 expression of the studied population and/or different AML subtypes.
This study showed that increased BECN1 gene expression was associated with increase WBC count (r = 0.697, P < 0.0001) in newly diagnosed AML patients (Table 2). Previous studies found that autophagy can affect myeloid cell proliferation, differentiation and apoptosis (19, 23, 24). Thus in this study, the positive correlation between overexpression of BECN1 and increased WBC count might be due to the effect of increased autophagy on these cellular functions; however, more studies are warranted.
Palmeira dos Santos et al. showed that inhibition of autophagy in the initial stage could lead to increase cytarabine-induced cell death in AML cell lines (19). Lian et al. showed that increased BECN1 gene expression correlated with poor prognosis in AML patients (25). In the present study, BECN1 gene expression level was significantly lower (0.73 fold, P = 0.004) in patients with complete remission than the newly diagnosed AML patients (Figure 2). Hence, it seems that autophagy activity might be reduced in complete remission. The results of this study showed that BECN1 can possibly be a useful biomarker in assessing remission status. It is also speculated that autophagy inhibition by targeting BECN1 can be utilized as a new approach to improve treatment in relapsed or refractory AML patients. Further investigation is required to follow-up patients and confirm prognostic significance of BECN1 in AML patients. Furthermore, relationship between BECN1 gene with MRD (Minimal residual disease) can be evaluated in future studies. We had some limitation for BECN1 protein measurement; thus, we recommend future studies to examine BECN1 protein expression using western blotting in AML patients.
5.1. Conclusions
Our study showed that low expression of the BECN1 gene might be associated with complete remission. Therefore, it is likely that the BECN1 gene could be used as a potential biomarker to assess remission status. Moreover it seems that targeting BECN1 might be a potential strategy to improve treatment in AML patients.
Acknowledgements
References
-
1.
Saultz JN, Garzon R. Acute myeloid leukemia: A concise review. J Clin Med. 2016;5(3). [PubMed ID: 26959069]. [PubMed Central ID: PMC4810104]. https://doi.org/10.3390/jcm5030033.
-
2.
Shallis RM, Wang R, Davidoff A, Ma X, Zeidan AM. Epidemiology of acute myeloid leukemia: Recent progress and enduring challenges. Blood Rev. 2019;36:70-87. [PubMed ID: 31101526]. https://doi.org/10.1016/j.blre.2019.04.005.
-
3.
Estey EH. Treatment of acute myeloid leukemia. Haematologica. 2009;94(1):10-6. [PubMed ID: 19118375]. [PubMed Central ID: PMC2625419]. https://doi.org/10.3324/haematol.2008.001263.
-
4.
Cull EH, Altman JK. Contemporary treatment of APL. Curr Hematol Malig Rep. 2014;9(2):193-201. [PubMed ID: 24643310]. [PubMed Central ID: PMC4131433]. https://doi.org/10.1007/s11899-014-0205-6.
-
5.
Bryan JC, Jabbour EJ. Management of relapsed/refractory acute myeloid leukemia in the elderly: Current strategies and developments. Drugs Aging. 2015;32(8):623-37. [PubMed ID: 26286093]. https://doi.org/10.1007/s40266-015-0285-6.
-
6.
Zhang J, Gu Y, Chen B. Mechanisms of drug resistance in acute myeloid leukemia. Onco Targets Ther. 2019;12:1937-45. [PubMed ID: 30881045]. [PubMed Central ID: PMC6417008]. https://doi.org/10.2147/OTT.S191621.
-
7.
Badadani M. Autophagy mechanism, regulation, functions, and disorders. ISRN Cell Biol. 2012;2012:1-11. https://doi.org/10.5402/2012/927064.
-
8.
Kang R, Zeh HJ, Lotze MT, Tang D. The Beclin 1 network regulates autophagy and apoptosis. Cell Death Differ. 2011;18(4):571-80. [PubMed ID: 21311563]. [PubMed Central ID: PMC3131912]. https://doi.org/10.1038/cdd.2010.191.
-
9.
Chen N, Debnath J. Autophagy and tumorigenesis. FEBS Lett. 2010;584(7):1427-35. [PubMed ID: 20035753]. [PubMed Central ID: PMC2843775]. https://doi.org/10.1016/j.febslet.2009.12.034.
-
10.
Degenhardt K, Mathew R, Beaudoin B, Bray K, Anderson D, Chen G, et al. Autophagy promotes tumor cell survival and restricts necrosis, inflammation, and tumorigenesis. Cancer Cell. 2006;10(1):51-64. [PubMed ID: 16843265]. [PubMed Central ID: PMC2857533]. https://doi.org/10.1016/j.ccr.2006.06.001.
-
11.
Mei Y, Thompson MD, Cohen RA, Tong X. Autophagy and oxidative stress in cardiovascular diseases. Biochim Biophys Acta. 2015;1852(2):243-51. [PubMed ID: 24834848]. [PubMed Central ID: PMC4231019]. https://doi.org/10.1016/j.bbadis.2014.05.005.
-
12.
Li L, Chen Y, Gibson SB. Starvation-induced autophagy is regulated by mitochondrial reactive oxygen species leading to AMPK activation. Cell Signal. 2013;25(1):50-65. [PubMed ID: 23000343]. https://doi.org/10.1016/j.cellsig.2012.09.020.
-
13.
Fulda S. Autophagy in cancer therapy. Front Oncol. 2017;7:128. [PubMed ID: 28674677]. [PubMed Central ID: PMC5475391]. https://doi.org/10.3389/fonc.2017.00128.
-
14.
Yang ZJ, Chee CE, Huang S, Sinicrope FA. The role of autophagy in cancer: Therapeutic implications. Mol Cancer Ther. 2011;10(9):1533-41. [PubMed ID: 21878654]. [PubMed Central ID: PMC3170456]. https://doi.org/10.1158/1535-7163.MCT-11-0047.
-
15.
Bao L, Jaramillo MC, Zhang Z, Zheng Y, Yao M, Zhang DD, et al. Induction of autophagy contributes to cisplatin resistance in human ovarian cancer cells. Mol Med Rep. 2015;11(1):91-8. [PubMed ID: 25322694]. [PubMed Central ID: PMC4237096]. https://doi.org/10.3892/mmr.2014.2671.
-
16.
Liu D, Yang Y, Liu Q, Wang J. Inhibition of autophagy by 3-MA potentiates cisplatin-induced apoptosis in esophageal squamous cell carcinoma cells. Med Oncol. 2011;28(1):105-11. [PubMed ID: 20041317]. https://doi.org/10.1007/s12032-009-9397-3.
-
17.
Nourkeyhani H, Jason DHP, Scott P, Hanekamp D, Johnson M, Wang ES. Targeting autophagy as a therapeutic strategy in acute myeloid leukemia. Blood. 2016;128(22):3950. https://doi.org/10.1182/blood.V128.22.3950.3950.
-
18.
Piya S, Andreeff M, Borthakur G. Targeting autophagy to overcome chemoresistance in acute myleogenous leukemia. Autophagy. 2017;13(1):214-5. [PubMed ID: 27797294]. [PubMed Central ID: PMC5240828]. https://doi.org/10.1080/15548627.2016.1245263.
-
19.
Palmeira dos Santos C, Pereira GJ, Barbosa CM, Jurkiewicz A, Smaili SS, Bincoletto C. Comparative study of autophagy inhibition by 3MA and CQ on Cytarabineinduced death of leukaemia cells. J Cancer Res Clin Oncol. 2014;140(6):909-20. [PubMed ID: 24659340]. https://doi.org/10.1007/s00432-014-1640-4.
-
20.
Roszak J, Smok-Pieniazek A, Stepnik M. Transcriptomic analysis of the PI3K/Akt signaling pathway reveals the dual role of the c-Jun oncogene in cytotoxicity and the development of resistance in HL-60 leukemia cells in response to arsenic trioxide. Adv Clin Exp Med. 2017;26(9):1335-42. [PubMed ID: 29442453]. https://doi.org/10.17219/acem/65475.
-
21.
Hu XY, Bai H, Pan YZ, Wnag CB, Wu B, Zhao Q, et al. [Expression of autophagy related gene Beclin1 and MAPLC3 in bone marrow mononuclear cells isolated from acute leukemia patients and its significance]. Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2011;19(3):598-601. Chinease. [PubMed ID: 21729531].
-
22.
Keyvan L, Bidoki SK, Zare Abdollahi D, Mansouri N, Hashemi M, Mortazavi Tabatabaei S, et al. Lack of altered BECN1 gene expression in Iranian patients with acute myeloid leukemia. Asian Pac J Cancer Prev. 2016;17(12):5173-7. [PubMed ID: 28124883]. [PubMed Central ID: PMC5454654]. https://doi.org/10.22034/APJCP.2016.17.12.5173.
-
23.
Mourgues L, Imbert V, Nebout M, Colosetti P, Neffati Z, Lagadec P, et al. The BMI1 polycomb protein represses cyclin G2-induced autophagy to support proliferation in chronic myeloid leukemia cells. Leukemia. 2015;29(10):1993-2002. [PubMed ID: 25925206]. https://doi.org/10.1038/leu.2015.112.
-
24.
Rothe K, Lin H, Lin KB, Leung A, Wang HM, Malekesmaeili M, et al. The core autophagy protein ATG4B is a potential biomarker and therapeutic target in CML stem/progenitor cells. Blood. 2014;123(23):3622-34. [PubMed ID: 24755409]. https://doi.org/10.1182/blood-2013-07-516807.
-
25.
Lian Y, Xie Y, Hong M, Zhu Y, Zhao H, Zhao X, et al. Clinical significance of BECLIN1 and ATG5 expression in acute myeloid leukemia patients. Int J Clin Exp Pathol. 2018;11(3):1529-37. [PubMed ID: 31938250]. [PubMed Central ID: PMC6958170].