Abstract
Background:
In the health services, financial resources are limited. An important way to save and prevent resources from going to waste is to use clinical guidelines.Objectives:
The objective of this study was to estimate the wasted cost as a result of ignoring clinical guidelines for a typical disease.Methods:
This cross-sectional study was performed in Fars province. 392 physicians were enrolled in this study and were asked to write a prescription for a hypothetical patient with streptococcal sore throat. Prescriptions were priced and compared to standard treatment costs and analyzed by SPSS software.Results:
Mean, median and mode of prescribed drugs in each prescription was 3.1, 3.0 and 3.0, respectively. Only 8.4% of the prescriptions were in accordance with the clinical guidelines, and 12% had led to mistreatment. Usually, physicians with more experience prescribed more expensive medications, and 45.5% of the total medication cost had gone to waste. About 5% of household drugs are waste. Due to mistreatment, 2 patients developed acute rheumatic fever.Conclusions:
Waste of recourses and patients out of pocket payment was high, which reduces patient’s ability for obtain other necessary healthcare services. Hence, training the physicians and developing clinical guidelines is an urgent necessity to prevent resources from being wasted.Keywords
1. Background
In the health services, resources (especially financial resources) are limited, and health policy makers have to prioritize their needs (1). The World Health Organization reported that in some countries 20% - 40% of healthcare expenditure is waste (2). The Organization of Economic Cooperation and Development (OECD) has also reported that one-fifth of the cost spen (3, 4). Wasting resources can be divided into three areas: resource waste in the administrative sector, in the operational domain and in the clinical domain. In the last domain one major source of waste is over medication (5).
Cost of drug is a concerning issue for both consumers and governments. On the other hand, the National Health Accounts (NHA) showed that a significant portion of these resources is for medical costs, varying between 12% - 20% over the years, depending on a country’s economic condition (6).
Surveys in various European, American and Asian countries showed that due to inflation rate, the cost of medication has increased over the years, and therefore the share of medicines from GDP has also increased. These countries are struggling with strategies, such as insurance coverage, changing drug usage behavior, changing the cost of medication based on prescription medications (changing prescribing practices), changing insurance coverage based on prescription drugs, use of Computerized Physician Order Entry and other methods (7, 8). Amongst these countries, drug costs in the United States had increased during the years 2000 to 2010, but it decreased from 17.8% to 15.2% between 2007 – 2016 (9). Research also showed that the largest portion of treatment cost in Iran is related to the cost of medicine, and people are most likely to use medicinal products when they become sick (10).
Logical drug prescribing is defined as “patients receiving medicine according to their clinical needs, in doses that meet their own individual requirements for a specific period of time, at the lowest cost for them and their community” (11).
Streptococcal sore throat is one of the most common illnesses that affects approximately 2% - 10% of people annually, which requires medical attention and use of medication (12) . Failure to treat or mistreat can lead to rheumatic fever and other complications that can result in high medical cost and problems for patients as well as the healthcare system (13, 14).
Due to high prevalence of this disease, the use of expensive medication, the prescription of additional medication, and ultimately inaccurate prescription, could in turn put a heavy burden of cost on the country’s healthcare system as well as the patient.
The clinical guidelines help therapists to provide the most effective and accessible treatment. The most effective treatment at the lowest cost for each disease should be selected and used uniformly. Alternative therapies are also included in these guidelines to help patients with difficulty or sensitivity to a specific medication.
Investigation various studies showed that 37% of those who had referred to a doctor with a sore throat had streptococcal sore throat (13). The statistics show that on average, every Iranian catch cold or sore throat 3 - 6 times annually, of which 37% are streptococcal sore throats, with an incidence of 1 - 2 times per year per each person (15).
With respect to the population of Iran, if proper medication is not prescribed, the imposed cost on the healthcare system will be high.
2. Objectives
This study was designed to evaluate the waste of cost for treating streptococcal sore throat in Fars province.
3. Methods
3.1. Study Design
This cross-sectional study was performed in Fars province. Sample size was calculated at 392, based on the number of general physicians, specialists and sub-specialists who work in Fars province (based on the data published from Shiraz University of Medical Sciences in 2016 – 2564 person) and a 90% confidence interval. We did not use informed consent.
3.1.2. Inclusion Criteria
General physician, specialist or sub-specialist who worked in medical filed in Fars providence by excluding gender differences and work experience. Participation in this project was voluntarily.
3.1.3. Exclusion Criteria
Not willing to write any prescription
3.2. Case Presentation
The status of a patient who visit a physician by describing his/her disease in detail. Finally, with the diagnosis of streptococcal sore throat, the doctor was asked to write a prescription for the patient. The design and presentation of the disease was done base on Nelson textbook of pediatrics in collaboration with several faculty members of Shiraz University of Medical Sciences. Standard treatment of the disease was also determined based on Nelson textbook of pediatrics (3).
After collecting all the prescriptions, they were appraised and summarized, and herbal, injectable, and non-injectable items were identified. The correctness or incorrectness of the prescribed drugs was also determined by comparing them with the standard treatment of the disease. All data were analyzed by SPSS version 21.
4. Results
In this study, 285 general physicians, 85 specialists and 22 subspecialists participated. The mean and median of their work experience were 12.4 and 12 years with standard deviation 8.8 years, respectively. The min and max work experience were 0.5 and 35 years. The physician status is presented in Table 1. The first three specialties that participated in this study were Anesthesiology, internal medicine and pediatrician.
The Sectors that Physician Who Worked in It
| Sector | Frequency | Percent | Valid Percent | Cumulative Percent |
|---|---|---|---|---|
| Governmental | 150 | 38.3 | 41.8 | 41.8 |
| Private | 129 | 32.9 | 35.9 | 77.7 |
| Both | 80 | 20.4 | 22.3 | 100.0 |
| Not answer | 33 | 8.4 | - | - |
| Total | 392 | 100.0 | - | - |
Based on standard treatment protocol, prescriptions were appraised and compared with standard treatment costs and if the proposed drugs were different from the protocol, but reached the therapeutic goal, they were considered to be the correct treatment.
The mean, median, mode and number of prescribed drugs in each prescription was 3.1, 3.0 and 3.0, respectively with SD equal to 0.91.
The minimum number of prescribed drug was 1 and maximum was 6 items. The frequency of prescription base on number of prescribed drugs is shown in Tables 2 and 3.
The Frequency of Prescription Base on Number of Prescribed Drugs
| No. of Items (Drugs) | Frequency | Percent | Valid Percent | Cumulative Percent |
|---|---|---|---|---|
| 1.00 | 18 | 4.6 | 4.6 | 4.6 |
| 2.00 | 71 | 18.1 | 18.1 | 22.7 |
| 3.00 | 189 | 48.2 | 48.2 | 70.9 |
| 4.00 | 91 | 23.2 | 23.2 | 94.1 |
| 5.00 | 19 | 4.8 | 4.8 | 99.0 |
| 6.00 | 4 | 1.0 | 1.0 | 100.0 |
| Total | 392 | 100.0 | 100.0 |
The Frequency of Prescribed Drugs Based on Rout of Administration
| Number of Drug | Dosage Form, No. (%) | ||||
|---|---|---|---|---|---|
| Prescriptions with Inj. | Prescriptions with Tab/ Capsules | Prescriptions with Syrup | Prescriptions with Herbal Medicine | Prescriptions with Other Dosage Form | |
| 0 | 83 (21.2) | 38 (9.7) | 119 (30.4) | 368 (93.9) | 364 (92.9) |
| 1 | 291 (74.2) | 209 (53.3) | 242 (61.7) | 24 (6.1) | 26 (6.6) |
| 2 | 18 (4.6) | 117 (29.8) | 29 (7.4) | 0 (0.0) | 2 (0.5) |
| 3 | 0 (0.0) | 26 (6.6) | 2 (0.5) | 0 (0.0) | 0 (0.0) |
| 4 | 0 (0.0) | 2 (0.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
The standard prescription cost for the hypothetical patients is about 60,200- 65,000 Rials, according to the 2016 currency rate (1$ US = 39000 IRR). Our result showed that the minimum cost of a prescription was 27,700 IRR (0.71$ US) and maximum cost was 1,187,000 IRR (30.43$ US). The mean, median and mode of prescription cost was 114,905 IRR (3.02$ US), 94,350 IRR (2.42$ US) and 49,700 IRR (1.27$ UD) with SD = 120,077 IRR (3.08$ US). The quartile division of prescriptions is shown in Table 4.
Quartile Deviation of Prescriptions
| Quartile | Cost (IRR) |
|---|---|
| 25 | 66,175 |
| 50 | 94,350 |
| 75 | 122,700 |
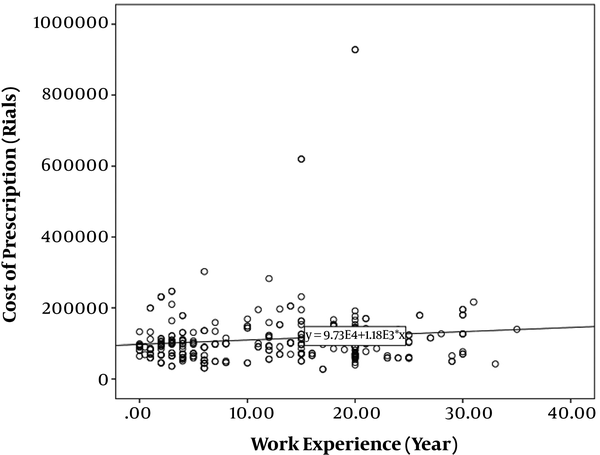
Our results showed that with increasing physician’s work experience, the cost of each prescription rose (Figure 1), but it did not significantly correlate with the number of prescribed drugs.
Correlation between work experience and cost of prescriptions by the physicians
The rate of incorrect treatment was significantly higher amongst physicians with less work experience.
The cost of prescribed drugs and the correct administration of drugs in the governmental and private sectors did not significantly differ.
We did not find any relationship between the cost of medication and other factors. (Such as work experience, spatiality and sectors)
Studies showed that each Iranian catches sore throat 3 - 6 times a year, of which 37% are streptococcal sore throat. Consequently, our estimate is as follows:
Mean of sore throat for Fars province population per year:
4,851,274 * (3 + 6/2) = 21,830,733
Number of streptococcal sore throat for Fars province population per year:
21,830,733 * 0.37 = 8,077,371
Cost of standard streptococcal sore throat treatment:
8,077,371 * (60200 + 65000/2) = 505,643,424,600 IRR (12.965.216$ US)
The amount of treatment cost based on the study results:
8,077,371 * 114,905 = 928,130,314,755 IRR (23.798.213$ US)
Waste of resources in Fars Province:
928,130,314,755 - 505,643,424,000 = 422,480,890,155 IRR (10.832.843$ US)
Household Budget Survey in Urban Areas of Iran in 2016 showed each person pays 7,050,972 IRR (181$ US) for his pharmaceutical expenses per year.
The household size in Fars province is 3.33, hence:
Per capita drug cost per person in Fars province is:
7,050,972/3.3 = 2,136,658 IRR (55$ US) per year
On the other hand, 12.0% of the prescription drugs were incorrect. In this groups, all the cost had gone to waste; thus, the cost of complications must be add to other unnecessary costs.
(12.0% * 8,077,371) * 114,905 = 111,375,637,771 IRR (2.855.785$ US)
Total waste cost was equal to:
111,375,637,771 + 422,480,890,155 = 533,856,527,926 IRR (13.688.628$ US)
The amount of money wasted per person in Fars province per year:
533,856,527,926/4,851,274 = 110,045 IRR (2.82$ US)
Percentage of waste cost per person in Fars province from household drug cost:
(110,045/2,136,658) * 100 ≈ 5.2%
Also:
Sum of 392 prescription price: 45,042,710 IRR (1386$ US)
The standard cost of 392 prescription price: 24,539,200 IRR (629.2$ US)
Differences = 45,042,710 - 24,539,200 = 20,503,510 IRR (525.7$ US)
Percent of cost waste = (20503510/45042710) * 100 = 45.5%
5. Discussion
The resource limitations forces the governments to save and reduce their costs. Since many treatment costs are indispensable and non-removable, some drugs are not covered by insurance systems (16), the best solution is to avoid losing the resources. The use of clinical guidelines as an appropriate way to prevent mistreatment and costly treatment can significantly prevent such events.
However, according to the results of this study, only 8.4% of prescriptions were in accordance with the clinical guidelines, and 12% were incorrect. In other cases, although the prescriptions were not in accordance with the clinical guidelines, it was able to treat the disease, but the prescribed medication price was far more than the standard version. Carol et al. showed 9.6% of the prescriptions to be inappropriate (17), and this difference can be related to the study method. In their retrospective study, much of the data was not available, and the diagnosis of the disease and the person who had written the prescription was only one person; hence, there was the possibility of a misdiagnosis. On the contrary, in this study we described a hypothetical patient with a single and straightforward diagnosis, which seems to be more realistic.
In this study, the mean, median and mode of prescribed drugs in each prescription was 3.1, 3.0 and 3.0,respectively. Heng Wang et al. showed the mean of prescribed drug to be 3.52, and in Rezazadeh et al. study it was 3.64 (18, 19). Since the average number of prescription drugs depend on the type of disease and season; hence, in the aforementioned studies, the total number of patients was reviewed, so that this difference could be due to the mentioned issues.
The increase in doctors’ work experience was directly associated with an increase in drug cost, but did not correlate with the number of drug items. The result of Murshid and Mohaidin’s studies confirm our finding (18, 20).
However, the most important issue in our study was the cost of streptococcal sort throat treatment. The average cost of treatment in Fars province is almost twice as much as the average standard treatment.
The result showed that 75% of prescriptions were above 25% of quartile with cost equal to 661,75 IRR. Albejaidi and Nair showed that 20% - 40% of healthcare cost goes to waste. In our study about 45.5% of medications were wasted, but could have been prevented.
On the other hand, other cost analysis showed that about 5.2% of family medicine goes to waste, but we could not find any study in this respect.
Additionally, incomplete and incorrect treatment will place a heavy burden of costs on the healthcare system of a country. The risk of developing ARF due to inaccurate or untreated patients with streptococcal pharyngitis is about 3% (21). Based on the results, the percentage of inaccurate treatment was 12. With 3% inaccurate treatment about 2 patients will develop acute rheumatic fever. Although the cost of rheumatic fever treatment was not estimated, a study in New Zealand estimated the cost to be about 40,842$ per case. It is about 1,170,286,668 IRR (30007.9$ UD) that has to be added to other costs.
One of the limitations of this study is hypothetical patient use. It is better to use a real patient if possible.
In conclusion, treatment without clinical guidelines in Iran is not efficient. In this case the waste of resources is high and due to low insurance coverage, patients out of pocket payment is also high. Increased wastage of household drug cost will lead to patient’s inability to use the necessary healthcare services. Consequently, training the physicians as well as developing clinical guidelines, public education, implementation of Computerized Physician Order Entry and strengthening supervisioning systems are urgent requirements of the country’s healthcare system to prevent waste of resources.
Acknowledgements
References
-
1.
Harrison KL, Taylor HA. Healthcare resource allocation decisions affecting uninsured services. Journal of health organization and management. 2016;30(8):1162-82. [PubMed ID: 27934550]. https://doi.org/10.1108/JHOM-01-2016-0003.
-
2.
Singh PK, Travis P. Universal health coverage in the World Health Organization South-East Asia Region: how can we make it "business unusual"? WHO South East Asia J Public Health. 2018;7(1):1-4. [PubMed ID: 29582842]. https://doi.org/10.4103/2224-3151.228420.
-
3.
Kliegman R, Stanton B, St. Geme JW, Schor NF, Behrman RE, Nelson WE. Nelson textbook of pediatrics. W. B. Saunders; 2016.
-
4.
Mueller M, Hagenaars L, Morgan D. Administrative spending in OECD health care systems: Where is the fat and can it be trimmed? OECD. 2017. https://doi.org/10.1787/9789264266414-9-en.
-
5.
Stanek JJ, Renslow MA, Kalliainen LK. The Effect of an Educational Program on Opioid Prescription Patterns in Hand Surgery: A Quality Improvement Program. The Journal of Hand Surgery. 2015;40(2):341-6. https://doi.org/10.1016/j.jhsa.2014.10.054.
-
6.
Farhadi J, Framarzi A. [Investigation of National Health Accounts in Iran between 2001-2013]. Bi-Mounthly Scientific-Research Statistics journal. 2016;4(4):9-13. Persian.
-
7.
Hossein Z, Gerard A. Trends in cost sharing among selected high income countries--2000-2010. Health Policy. 2013;112(1-2):35-44. [PubMed ID: 23809913]. https://doi.org/10.1016/j.healthpol.2013.05.020.
-
8.
Heydari MR, Mirahmadizadeh AR, Kadivar MR, Hashempour T, Arbabisarjou A, Joulaei H. Study causes of illegible handwriting prescription as a barrier for the right treatment: A cross-sectional study in Southern Iran. Drug Invention Today. 2019;11(8).
-
9.
Nekoeimoghadam M, Esfandiari A, Ramezani F, Amiresmaili M. Informal payments in healthcare: a case study of kerman province in iran. Int J Health Policy Manag. 2013;1(2):157-62. [PubMed ID: 24596856]. [PubMed Central ID: PMC3937917]. https://doi.org/10.15171/ijhpm.2013.28.
-
10.
Amery H, Jafari A, Panahi M. Determining the rate of Catastrophic Health Expenditure and its influential factors on families in Yazd Province. Journal of Health Administration (JHA). 2013;16(52).
-
11.
Aravamuthan A, Arputhavanan M, Subramaniam K, Udaya Chander J. Assessment of current prescribing practices using World Health Organization core drug use and complementary indicators in selected rural community pharmacies in Southern India. J Pharm Policy Pract. 2017;10. [PubMed ID: 27446591]. [PubMed Central ID: PMC4955117]. https://doi.org/10.1186/s40545-016-0074-6.
-
12.
Gunnarsson MS, Sundvall PD, Gunnarsson R. In primary health care, never prescribe antibiotics to patients suspected of having an uncomplicated sore throat caused by group A beta-haemolytic streptococci without first confirming the presence of this bacterium. Scand J Infect Dis. 2012;44(12):915-21. [PubMed ID: 22830425]. https://doi.org/10.3109/00365548.2012.700768.
-
13.
Shaikh N, Leonard E, Martin JM. Prevalence of streptococcal pharyngitis and streptococcal carriage in children: a meta-analysis. Pediatrics. 2010;126(3):e557-64. [PubMed ID: 20696723]. https://doi.org/10.1542/peds.2009-2648.
-
14.
Atif M, Azeem M, Rehan Sarwar M, Malik I, Ahmad W, Hassan F, et al. Evaluation of prescription errors and prescribing indicators in the private practices in Bahawalpur, Pakistan. J Chin Med Assoc. 2018;81(5):444-9. [PubMed ID: 29548936]. https://doi.org/10.1016/j.jcma.2017.12.002.
-
15.
Cohen JF, Cohen R, Levy C, Thollot F, Benani M, Bidet P, et al. Selective testing strategies for diagnosing group A streptococcal infection in children with pharyngitis: a systematic review and prospective multicentre external validation study. Cmaj. 2015;187(1):23-32.
-
16.
Joulaei H HM. Elimination of Over-the-Counter Medicines from the Health Insurance Coverage: A Right or Wrong Decision. IJPH. 2019;48(8):1553-4.
-
17.
Renom-Guiteras A, Meyer G, Thürmann PA. The EU(7)-PIM list: a list of potentially inappropriate medications for older people consented by experts from seven European countries. European Journal of Clinical Pharmacology. 2015;71(7):861-75. https://doi.org/10.1007/s00228-015-1860-9.
-
18.
Rezazadeh A, Abrishami R. Evaluation of Prescribing Indicators if General Practitioners in a Military Hospital in Tehran. Journal of Police Medicine. 2017;6(1):13-20.
-
19.
Rancourt C, Moisan J, Baillargeon L, Verreault R, Laurin D, Grégoire J. Potentially inappropriate prescriptions for older patients in long-term care. BMC Geriatrics. 2004;4(1). https://doi.org/10.1186/1471-2318-4-9.
-
20.
Murshid MA, Mohaidin Z. Models and theories of prescribing decisions: A review and suggested a new model. Pharm Pract (Granada). 2017;15(2):990. [PubMed ID: 28690701]. [PubMed Central ID: PMC5499356]. https://doi.org/10.18549/PharmPract.2017.02.990.
-
21.
Irlam J, Mayosi BM, Engel M, Gaziano TA. Primary prevention of acute rheumatic fever and rheumatic heart disease with penicillin in South African children with pharyngitis: a cost-effectiveness analysis. Circ Cardiovasc Qual Outcomes. 2013;6(3):343-51. [PubMed ID: 23652737]. https://doi.org/10.1161/CIRCOUTCOMES.111.000032.