Abstract
Context:
Transient ischemic dilatation (TID) of the left ventricle is a non-invasive marker of suspected or known Coronary Artery Disease (CAD), and is used for the prediction of prognosis. Because the value of TID has been emphasized by current publications in clinical nuclear cardiology field, the current review of the literature was conducted to present comprehensive overview on the findings in this field.Evidence Acquisition:
Relevant literature was obtained by searching online databases, including MEDLINE/PubMed, Google Scholar, and Science Direct using the following keywords: transient ischemic dilation, Single Photon Emission Computed Tomography Myocardial Perfusion Imaging (SPECT MPI), procedural guidelines for myocardial perfusion imaging, and coronary artery disease. Articles were inspected to obtain good agreement criteria pertinent to the objective of the study. Overall, 21 relevant articles were selected to be included in the review.Results:
Stress-induced subendocardial hypoperfusion, post-ischemic stunning, and impaired coronary flow reserve have been reported as common causes of TID. Transient Ischemic Dilatation can be easily measured by available automatic software on the market, including Emory Cardiac Toolbox, 4D-MSPECT, etc. A close correlation between TID and LV volume/function has been emphasized by previous researchers. Transient Ischemic Dilatation, in the setting of a cardiac SPECT MPI with abnormal findings, has been known to be a robust indicator of severe/extensive CAD and future cardiac events. However, only a limited number of publications are available for its probable use in the setting of normal MPI, especially based on patients at high-risk and those with TID.Conclusions:
By using an upper limit value of TID that is derived according to the optimum imaging procedure of a particular laboratory, routine reporting of TID measurement as part of conventional SPECT MPI analysis may be useful.Keywords
Coronary Artery Disease Myocardial Perfusion Imaging Myocardial Ischemia Dilatation Tomography Emission-Computed Single-Photon
1. Context
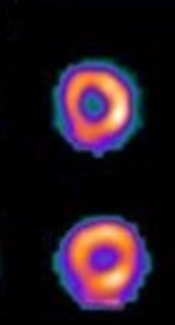
Cardiac single photon emission computed tomography myocardial perfusion imaging (SPECT MPI) is a useful non-invasive imaging test for evaluation of suspected or known coronary artery disease (CAD). It offers advantages to clinicians by combining evaluation of myocardial perfusion pattern and functional status of the left ventricle (LV). Additionally, stress-induced ischemic LV dysfunction may be demonstrated by transient ischemic dilatation (TID) of LV. It can be measured by dividing the volume of the endocardial surface of the LV cavity on cardiac images obtained at post-stress and rest conditions. Measurement of TID can be performed by commercially available software without additional cost burden and radiation risk for the patients. Currently, TID is recognized as one of the novel indicators of severe/extensive CAD and cardiac events (e.g., non-fatal myocardial infarction and cardiac death), as well as their prognosis (1-3). Several current reports have emphasized that TID could be used as a powerful marker even when cardiac MPI indicates the presence of a normal myocardial perfusion (4, 5).
2. Evidence Acquisition
In this review study, relevant literature was obtained by searching online databases, including MEDLINE/PubMed, Google Scholar, and Science Direct, using the following keywords, transient ischemic dilation, SPECT MPI, procedural guidelines for myocardial perfusion imaging, and coronary artery disease. Articles were inspected to obtain good agreement criteria pertinent to the objective of the study. Overall, 21 relevant articles were selected for the review.
3. Results
3.1. Mechanism of Transient Ischemic Dilatation
Normally, the size of left ventricular cavity on a rest perfusion imaging is larger than detected on stress perfusion imaging. In 1980, by a case series with 3 patients, Stolzenberg et al. described the dilation of left ventricular cavity on a thallium scan that was characterized by increased diameter of LV cavity at stress when compared to the rest condition (6). They interpreted that this finding could be useful to get rid of false negatives that cause balanced lesions. The definitive mechanism of formation of this phenomenon is still controversial. However, it seems to emerge as a result of various processes, which may be pathological and physiological. The most often-accused ones are absolute LV cavity dilatation and myocardial stunning, caused by ischemia, systolic LV dysfunction, stress-induced subendocardial hypoperfusion, and impaired coronary flow reserve (7, 8). In a study on the pathophysiology of TID performed by Emmett et al., they reported that a high TID ratio is associated with subendocardial hypoperfusion and/or impaired coronary flow reserve rather than chamber enlargement of the ventricle or myocardial stunning (7). In a series with 282 patients, Bestetti et al. reported that a post-stress, end-systolic ventricular dilation was detected on the SPECT MPI study, which was compatible with endocardial post-ischemic stunning, and these patients had more functional and anatomic abnormalities caused by CAD (8).
3.2. Measurement technique of Transient Ischemic Dilatation
TID defines the stress-rest LV volume ratio. Quantitative TID value is calculated traditionally on SPECT MPI from ungated SPECT stress and rest LV volumes. Borders of the endocardial surface are estimated by a proprietary edge detection algorithm, using the information from smoothed image. The algorithm segments the left ventricle, and determines the limits of the endocardial and epicardial areas for the images of stress and rest. It calculates the value of TID by dividing the volume of the endocardial surface of the LV cavity after stress, by the volume of the endocardial surface of the LV cavity at rest. There are a few commercially available software, including emory cardiac toolbox (9), Auto QUANT (10), and 4D-MSPECT (11, 12) with automatic measurement and display features.
3.3. Clinical Value of Transient Ischemic Dilatation
3.3.1. Correlation of Transient Ischemic Dilatation with volumetric Left Ventricle function
The relationship between the TID ratio and the volumetric measurements of the LV function has been evaluated by previous authors (7, 13-18). Emmett et al. (7) identified a good correlation between echocardiographic and gated SPECT MPI measurements for LV end-diastolic volume (LVEDV), LV end-systolic volume (LVESV) and LV ejection fraction (LVEF) values at rest. Although there was no a significant change in the functional and volumetric measurements obtained from the echocardiography (ECHO) for the TID negative group, a significant decrease in differential LVEF values obtained from SPECT MPI for the TID positive group was observed, yet, this was not detected in the concurrent ECHO measurements. Demir et al. (15) showed that transient left ventricular contractile dysfunction could develop during both exercise and pharmacological stress and they found a good relationship between TID ratios and LVEF values. A study by Del Val Gomez et al. (16) revealed that post-exercise LVEF values increased in patients with normal and fixed perfusion defects yet decreased in patients with reversible perfusion defect. Heston et al. (17) investigated the effect of relative contribution of LVEDV and LVESV ratios (post-stress to rest ratios) on TID value in a gated SPECT MPI. They found that there was better correlation for the LVEDV ratio than LVESV ratio and an optimized stress-induced volume ratio (LVESVx5.0 + LVEDV) was the most strongly correlated parameter. Hung et al. (18) showed that LVEDV and LVESV values were higher, yet, LVEF values and wall motions were lower with the post-stress condition than at rest in patients with high TID. They concluded that the enlargement of LVESV is the most potent effect on TID.
3.3.2. Role of Transient Ischemic Dilatation in known Coronary Artery Disease with Feasible Thresholds
An elevated TID ratio is closely associated with the presence of epicardial coronary stenosis and severe CAD, as a sensitive and specific quantitative indicator. Previous studies have clearly shown that the TID ratio can provide important predictive and prognostic information for identification of severe and extensive CAD as well as future cardiac events such as non-fatal myocardial infarction or cardiac death (5, 8-10, 19, 20). On the other hand, information on the use of TID ratio in patients undergoing CR is limited to a few studies. In the most notable, the authors (13) viewed the role of TID to determine presence of severe CAD and poor prognosis in patients with revascularization and without revascularization. They concluded that TID could be connected with high frequency of non-fatal MI and used as a predictor of multi-vessel CAD. They also suggested that it might be associated with a good clinical outcome in patients with CR. Some authors (16) have stated that patients with transient LV dysfunction might benefit from revascularization due to presence of reversibility.
Upper normal limit of TID was provided by several researchers to define significant CAD. However, range of normal limits and applicable threshold value can vary due to variables such as gender, type of the imaging protocol and automated software, characteristics of the patient cohort, etc. Abidov et al. (19) described that the TID ratio, measured automatically, is a good indicator of serious and widespread CAD. They found that a 1.36 threshold value for TID obtained from a stress SPECT MPI test in low risk patients had high sensitivity (73%) and specificity (88%) to demonstrate severe and common CAD. In addition, ratio of serious and common CAD in patients, who have no abnormal TID value and perfusion defects, was found to be low (1.3%), yet, otherwise it was significantly higher (65%). Mazzanti et al. (20) also defined TID as a clinical marker of serious and widespread CAD with a high sensitivity (74%) and specificity (95%). In this series, the best cut-off of TID was found to be 1.21. There was also a strong correlation between the size of perfusion defects and the TID measurement levels. Another study (21) was performed on 547 patients with suspected and known CAD, using 99mTc-MIBI rest/stress protocol to determine normal limit values of TID. For a group of patients with low-risk, the upper limit value of TID was calculated as 1.19 for an ungated study and 1.23 for a gated study. They found that the incidence of high TID value was 2% in normal patients, yet, increased to 36% in patients with severe CAD. A 1.19 threshold value was also determined by Kakhki et al. (9), using the Emory Cardiac Toolbox to be the upper normal limit of TID ratio in a 2-day dipyridamole stress/rest SPECT MPI test using 99mTc-MIBI. They reported that higher TID ratios were measured in cases with partial reversible defects or multi-vessel disease or perfusion abnormalities on the LAD artery territory. A high TID ratio was found to be an independent predictor of ischemia and territory perfusion abnormality. Duarte et al. (10) measured TID values of the LV on the stress/rest 99mTc-MIBI SPECT MPIs, using Auto QUANT software in patients with low probability and significant transient defect. The TID limits were between 0.13 and 1.01 for low-risk patients and between 0.17 and 1.18 for patients with significant transient defect. However, the highest positive predictive value to detect the widespread myocardial ischemia was obtained when the TID ratio was more than 1.25. Azambuja et al. (11) evaluated the difference for the average TID values between exercise stress testing and pharmacologic stress testing by the 4D-MSPECT software. In this study, 200 patients were studied in 2 groups of patients having similar properties. Mean values of TID were calculated to be 1.06 ± 0.23 for exercise stress testing and 1.10 ± 0.22 for dipyridamole stress testing and there was no a statistically significant difference between the values. In the current study (12), the usefulness of TID to determine significant obstructive of CAD in patients with prior coronary revascularization was evaluated. It was found that a 1.20 threshold of TID was a robust indicator of restenosis and had an accuracy of 87%.
3.3.3. Role of Transient Ischemic Dilatation in Coronary Artery Disease Patients with Normal Myocardial Perfusion
Literal information on the clinical significance of TID in patients with a normal MPI study is limited. According to the proposals of these few studies, TID value in the patients without apparent risk or an otherwise normal SPECT MPI test could give prognostic information for future cardiac events, if found higher than the defined threshold of TID (4, 5). In a study performed on 1560 patients, who had the MPS stress test in normal limits, the prognostic value of TID to predict hard and soft cardiac events were evaluated (4). This study showed that an entirely normal MPI test finding was not always consistent with an excellent prognosis, and TID had independent and incremental prognostic value to suggest the risk of total cardiac events in this patient population. They offered to be appropriate for patients with TID in the presence of typical angina, the elderly, and patients with diabetes. Another study of 1236 patients with normal myocardial perfusion, LV volume, and function revealed similar findings for prognostic value of TID (5). However, they found that incidence of TID was high in high-risk populations with diabetes and significant CAD.
4. Conclusions
Transient ischemic dilatation is an important marker of severe/extensive CAD and has prognostic value to predict the risk of cardiac events. By using an upper limit value of TID that was derived according to the optimum imaging procedure of a particular laboratory, routine reporting of TID measurement as part of conventional SPECT MPI analysis may be useful.
References
-
1.
Hesse B, Tagil K, Cuocolo A, Anagnostopoulos C, Bardies M, Bax J, et al. EANM/ESC procedural guidelines for myocardial perfusion imaging in nuclear cardiology. Eur J Nucl Med Mol Imaging. 2005;32(7):855-97. [PubMed ID: 15909197]. https://doi.org/10.1007/s00259-005-1779-y.
-
2.
Strauss HW, Miller DD, Wittry MD, Cerqueira MD, Garcia EV, Iskandrian AS, et al. Procedure guideline for myocardial perfusion imaging 3.3. J Nucl Med Technol. 2008;36(3):155-61. [PubMed ID: 18703619]. https://doi.org/10.2967/jnmt.108.056465.
-
3.
McLaughlin MG, Danias PG. Transient ischemic dilation: a powerful diagnostic and prognostic finding of stress myocardial perfusion imaging. J Nucl Cardiol. 2002;9(6):663-7. [PubMed ID: 12466791]. https://doi.org/10.1067/mnc.2002.124979.
-
4.
Abidov A, Bax JJ, Hayes SW, Hachamovitch R, Cohen I, Gerlach J, et al. Transient ischemic dilation ratio of the left ventricle is a significant predictor of future cardiac events in patients with otherwise normal myocardial perfusion SPECT. J Am Coll Cardiol. 2003;42(10):1818-25. [PubMed ID: 14642694].
-
5.
Doukky R, Frogge N, Bayissa YA, Balakrishnan G, Skelton JM, Confer K, et al. The prognostic value of transient ischemic dilatation with otherwise normal SPECT myocardial perfusion imaging: a cautionary note in patients with diabetes and coronary artery disease. J Nucl Cardiol. 2013;20(5):774-84. [PubMed ID: 23929206]. https://doi.org/10.1007/s12350-013-9765-4.
-
6.
Stolzenberg J. Dilatation of left ventricular cavity on stress thallium scan as an indicator of ischemic disease. Clin Nucl Med. 1980;5(7):289-91. [PubMed ID: 7389226].
-
7.
Emmett L, Ng A, Ha L, Russo R, Mansberg R, Zhao W, et al. Comparative assessment of rest and post-stress left ventricular volumes and left ventricular ejection fraction on gated myocardial perfusion imaging (MPI) and echocardiography in patients with transient ischaemic dilation on adenosine MPI: myocardial stunning or subendocardial hypoperfusion? J Nucl Cardiol. 2012;19(4):735-42. [PubMed ID: 22565241]. https://doi.org/10.1007/s12350-012-9571-4.
-
8.
Bestetti A, Di Leo C, Alessi A, Triulzi A, Tagliabue L, Tarolo GL. Post-stress end-systolic left ventricular dilation: a marker of endocardial post-ischemic stunning. Nucl Med Commun. 2001;22(6):685-93. [PubMed ID: 11403181].
-
9.
Kakhki VR, Sadeghi R, Zakavi SR. Assessment of transient left ventricular dilation ratio via 2-day dipyridamole Tc-99m sestamibi nongated myocardial perfusion imaging. J Nucl Cardiol. 2007;14(4):529-36. [PubMed ID: 17679061]. https://doi.org/10.1016/j.nuclcard.2007.03.002.
-
10.
Duarte PS, Smanio PE, Oliveira CA, Martins LR, Mastrocolla LE, Pereira JC. Clinical significance of transient left ventricular dilation assessed during myocardial Tc-99m sestamibi scintigraphy. Arq Bras Cardiol. 2003;81(5):474-82. [PubMed ID: 14666268].
-
11.
Azambuja Gonzalez MB, Azambuja RA, Bodanese LC. Quantification of left ventricular dilatation in myocardial perfusion scintigraphy. Arq Bras Cardiol. 2011;96(5):363-8. [PubMed ID: 21503392].
-
12.
Gultekin SS, Sadic M, Bilgin M, Koca G, Acikel S, Yeter E, et al. The value of transient ischemic dilation for detecting restenosis after coronary artery revascularization. J Nucl Cardiol. 2016. [PubMed ID: 27663249]. https://doi.org/10.1007/s12350-016-0607-z.
-
13.
uz Zaman M, Fatima N, Samad A, Ishaq M, Wali A, Rehman K, et al. Predictive and prognostic values of transient ischemic dilatation of left ventricular cavity for coronary artery disease and impact of various managements on clinical outcome using technetium-99m sestamibi gated myocardial perfusion imaging. Ann Nucl Med. 2011;25(8):566-70. [PubMed ID: 21629988]. https://doi.org/10.1007/s12149-011-0500-4.
-
14.
Xu Y, Arsanjani R, Clond M, Hyun M, Lemley MJ, Fish M, et al. Transient ischemic dilation for coronary artery disease in quantitative analysis of same-day sestamibi myocardial perfusion SPECT. J Nucl Cardiol. 2012;19(3):465-73. [PubMed ID: 22399366]. https://doi.org/10.1007/s12350-012-9527-8.
-
15.
Demir H, Tan YZ, Isgoren S, Gorur GD, Kozdag G, Ural E, et al. Comparison of exercise and pharmacological stress gated SPECT in detecting transient left ventricular dysfunction. Ann Nucl Med. 2008;22(5):403-9. [PubMed ID: 18600418]. https://doi.org/10.1007/s12149-008-0119-2.
-
16.
del Val Gomez M, Gallardo FG, San Martin MA, Garcia A, Terol I. Ischaemic related transitory left ventricular dysfunction in 201Tl gated SPECT. Nucl Med Commun. 2005;26(7):601-5. [PubMed ID: 15942480].
-
17.
Heston TF, Sigg DM. Quantifying transient ischemic dilation using gated SPECT. J Nucl Med. 2005;46(12):1990-6. [PubMed ID: 16330561].
-
18.
Hung GU, Lee KW, Chen CP, Lin WY, Yang KT. Relationship of transient ischemic dilation in dipyridamole myocardial perfusion imaging and stress-induced changes of functional parameters evaluated by Tl-201 gated SPECT. J Nucl Cardiol. 2005;12(3):268-75. [PubMed ID: 15944531].
-
19.
Abidov A, Bax JJ, Hayes SW, Cohen I, Nishina H, Yoda S, et al. Integration of automatically measured transient ischemic dilation ratio into interpretation of adenosine stress myocardial perfusion SPECT for detection of severe and extensive CAD. J Nucl Med. 2004;45(12):1999-2007. [PubMed ID: 15585473].
-
20.
Mazzanti M, Germano G, Kiat H, Kavanagh PB, Alexanderson E, Friedman JD, et al. Identification of severe and extensive coronary artery disease by automatic measurement of transient ischemic dilation of the left ventricle in dual-isotope myocardial perfusion SPECT. J Am Coll Cardiol. 1996;27(7):1612-20. [PubMed ID: 8636545].
-
21.
Xu Y, Arsanjani R, Clond M, Hyun M, Lemley MJ, Fish M. Transient ischemic dilation for coronary artery disease in quantitative analysis of same-day sestamibi myocardial perfusion SPECT. J Nucl Cardiol. 2012;19:465-73.