1. Background
One type of abortion is therapeutic abortion, which is called medical or surgical pregnancy termination before the fetus reaches a viable stage or before the 20th week of pregnancy and weighs less than 500 g (1, 2). It is estimated that approximately 40 million abortions occur each year, whether legally or illegally, resulting in a reported abortion rate of 3.5% (3). Techniques used to evacuate the uterus in the second trimester (from fourteen to twenty-two weeks) include surgical and medical procedures as taking medications (1). Surgical methods include dilation and evacuation, suction, curettage, laparotomy, and hysterotomy (4). But in the medical method, there are many treatments such as topical administration of hypertonic saline or urea, administration of systemic medications such as oxytocin, misoprostol (Miso) of the vaginal type, sublingual administration, cervical or a combination of Miso and mifepristone, carboprost, and others methods (5-7). It has been shown that in recent years, medical methods have been mostly used for abortions because this method is safer and more acceptable than surgical methods (8, 9).
One of the medical and medicinal approaches involves the use of prostaglandins, both alone and in combination with other medications (10, 11). Miso is an analog of prostaglandin E1, which is prescribed for the prevention and treatment of gastric and duodenal ulcers (12, 13). This substance is also used in obstetrics and gynecology to induce labor, prepare the cervix, treat postpartum hemorrhage (primary and secondary PPH), and induce abortion. It has also been shown that, unlike other prostaglandins, Miso selectively affects the uterus and cervix and has no adverse effects on the bronchi and blood vessels (14, 15).
In medical methods, in addition to the use of systemic and topical drugs, mechanical methods are also used to prepare the cervix. This procedure is performed using hygroscopic dilators. Thus, by inserting it in the cervix, it draws water from the tissues of the cervix and, as it expands, causes the gradual dilation of the cervix (16). The most common types of hygroscopic dilators are Laminaria digitata and Laminaria japonica, which are made from brown seaweed and inserted inside the cervix to induce labor. The stem of this algae is shaped after cutting and peeling its skin, dried and sterilized, and packed according to its size (17). Laminaria (Lam) most likely acts by absorbing water from proteoglycan complexes, and by breaking down these complexes, it softens and dilates the cervix. Also, since Lam is extracted from natural sources, it has few complications (18).
2. Objectives
According to the above, this study aimed to investigate the effect of vaginal Miso simultaneously with Lam in comparison with vaginal Miso alone in terminating the second trimester of pregnancy (14 to 20 weeks) in patients admitted to the hospital maternity ward of Ali-Ibn Abitaleb Hospital in Zahedan.
3. Methods
3.1. Selection of Patients
In this randomized controlled clinical trial study, pregnant women between 14 and 20 weeks of gestation who were admitted to Ali-Ibn Abitaleb Hospital in Zahedan from early July 2019 to the end of September 2020 and were candidates for pregnancy termination due to severe anomalies or were fetal deaths were investigated. Inclusion criteria were patients with conditions of singleton, parity 1 to 3, no pain, and uterine infection. Exclusion criteria were drug allergy, intrauterine device (IUD), severe anemia, anticoagulant use, active liver disease, cardiovascular disease, uncontrolled seizures, corticosteroids, and history of cesarean section and previous uterine incision, parity more than three, placenta previa, and contraindications to prostaglandin administration, including hypersensitivity to prostaglandins, asthma, glaucoma, and previous heart disease, were determined. Accordingly, and based on the formula for calculating the sample size, 90 women (45 women in each group) were included in the study.
n = [(Z1 – α/2 + Z1 – β)2 (p1 (1 - p1)) + (p2 (1 - p2))]/(p1 – p2)2 = [(1.96 + 1.64)2 (0.45 × 0.54 + 0.12 × 0.88)]/ (0.45 - 0.12)2 = 45
Furthermore, the present study was initially approved by the Ethics Committee of Zahedan University (code: IR.ZAUMS.REC.1398.078) and registered on the IRCT site (code: IRCT20190529043759N1). Then, the objectives, nature, and process of the research were explained to the sample, and consent to participate in the research was obtained from them. The sample was assured that the information would remain confidential and reminded that the results of the study would be made available to them if they wished. Patients also had the address and contact number of the researcher in case they had any specific questions or problems while receiving free medication and full care until discharge.
3.2. Methodology
In this study, patients were randomly divided into two groups of 45. The first group, or the control group, was administered vaginal Miso alone for therapeutic abortion, and the second group, in addition to vaginal Miso, Lam was administered simultaneously. Choosing to use which method for which patient was based on randomized blocking based on ten blocks, each containing five cards from the group alone and five cards from the group of Miso along with Lam, which were placed in a random permutation. In our study, before prescribing the medications, the patients were given sufficient information about the treatment method, drug complications, and benefits.
The method of treatment was that at the beginning of treatment in the first group or control group, 400 μg Miso suppository (made by Samisaz Company, Iran) was inserted into the posterior vagina of the patient every eight hours, and a vaginal examination was performed regularly every eight hours. This process continued up to six doses and if there was no expulsion by then, surgery was used to terminate the pregnancy. In the second group, the patient’s vagina was first flushed with betadine, and after speculum was inserted, the anterior lip of the cervix was grasped with a tenaculum, and a five mm lam (made by Cooper Surgical, USA) was inserted into the cervix, according to its size so that the tip was placed near the inner opening of the cervix. Then, 400 μg Miso suppository was simultaneously inserted in the posterior fornix of the vagina, and the patient was examined regularly every eight hours. If the fetus was not expelled after eight hours, the vaginal Miso was repeated. This process continued up to six doses, and if there was no expulsion by then, surgery was used to terminate the pregnancy.
In this study, information on both groups, including patient age, body mass index (BMI), gestational age (GA) based on ultrasound or date of last menstruation, number of hospitalization days (from the first day of treatment to the end of pregnancy), need for curettage (in case of remaining placenta and pregnancy remnants based on ultrasound or doctor’s diagnosis), the need for blood transfusions, the need for analgesics, and the symptoms and complications of medications (nausea, vomiting, rash, diarrhea, fever, and chills), was examined.
3.3. Statistical Analysis
The data were statistically analyzed using SPSS software version 25, after determining the descriptive central and dispersion indices using independent sample t-test and chi-square tests. A P-value of less than 0.05 was also considered significant.
4. Results
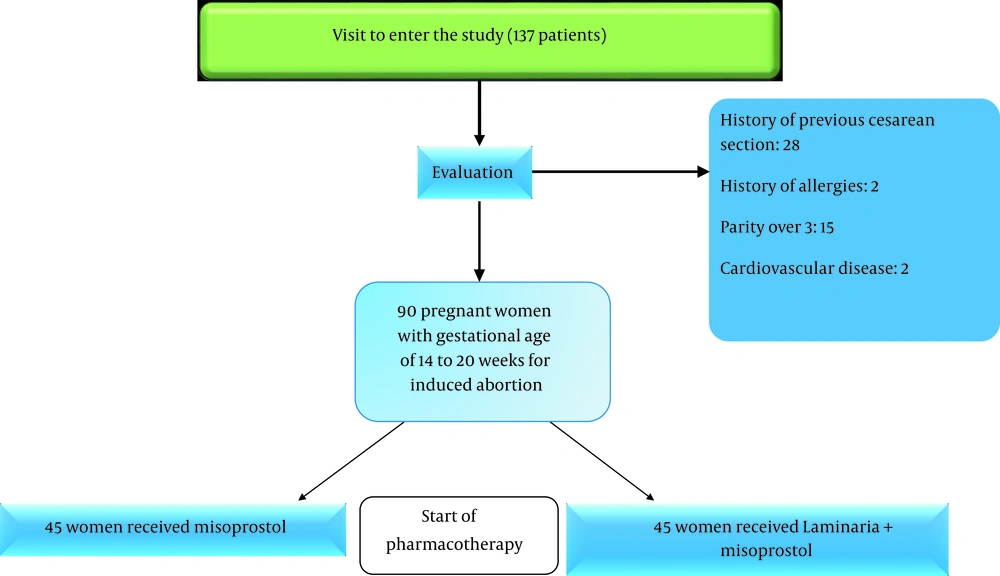
According to schematic Figure 1, 137 patients were included in the study, and after applying the inclusion and exclusion criteria, 90 people were investigated.
The mean age of patients in the two groups was not statistically significant (P = 0.31, Table 1). Also, the minimum and maximum age of participants in the Lam + Miso group were 18 and 40 years, respectively, and the minimum and maximum age of participants in the Miso group were 18 and 42 years, respectively. The study of GA also showed that in both groups, the minimum and maximum GA were 15 and 20 weeks, respectively. Also, according to Table 1, there was no significant difference in the GA of patients at the time of admission between the two groups (P = 0.11). Furthermore, there was no statistically significant difference between the two groups in terms of BMI (P = 0.09). The lowest and highest BMI were 19 and 35 kg/m2 in the Lam + Miso group and 18 and 35 kg/m2 in the Miso group, respectively.
| Variables | Misoprostol + Laminaria | Misoprostol | P-Value |
|---|---|---|---|
| Age (y) | 26.4 ± 40.97 | 27.04 ± 36.77 | 0.31 |
| Gestational age (week) | 17.88 ± 2.64 | 17.51 ± 2.11 | 0.11 |
| Body mass index (kg/m2) | 23.95 ± 21.13 | 23.44 ± 18.43 | 0.09 |
a Values are expressed as mean ± SD.
According to the results of the present study, none of the two groups required surgery and blood transfusion, and the number in both groups was zero. However, seven cases in the Miso + Lam group and 12 cases in the Miso group required curettage (Table 2). Our results showed that there was a statistically significant difference between the two groups and that the Miso + Lam group had better results than the group of Miso alone (P = 0.05). Also, there was a significant difference between the two groups in terms of mean hospital stay (P = 0.003) and labor duration (P = 0.04), and Lam, along with Miso, was able to show better results than the group of Miso alone.
| Type of Treatment/Type of Complication | Fever and Chills | Diarrhea | Headache |
|---|---|---|---|
| Misoprostol + laminaria | 3 | 2 | 1 |
| Misoprostol | 4 | 3 | 1 |
In addition, the complications observed in the two study groups are reported in Table 3, which were resolved quickly with simple care treatments, and there were no acute cases or lack of response to the treatment.
| Variables | Misoprostol + Laminaria | Misoprostol | P-Value |
|---|---|---|---|
| Requiring curettage | 0.20 ± 0.16 | 0.33 ± 0.22 | 0.05 |
| Duration of hospitalization (in days) | 1.30 ± 0.07 | 1.50 ± 0.11 | 0.003 |
| Duration of labor (in hours) | 9.51 ± 10.21 | 10.84 ± 11.72 | 0.04 |
a Values are expressed as mean ± SD.
5. Discussion
With the spread of prenatal diagnoses, termination of the second trimester of pregnancy is a very important issue in the treatment of patients. Termination of pregnancy is faster with surgery but is associated with more complications such as rupture and perforation of the uterus, intrauterine or intra-abdominal adhesions, cervical insufficiency in subsequent pregnancies, and severe bleeding (8, 19). Using the medical method is both less costly and decreases surgical complications such as bleeding and infection, as well as patients’ stress (20). Therefore, the present study aimed to compare the effects of Miso alone or in combination with Lam.
The results of our study showed that the factors of age, GA, and BMI of patients were not significantly different in the two groups, and all patients were studied on equal means in terms of statistical data. In the study of Behrashi et al., similar to the results of our study, which compared the effect of laminaria with misoprostol, the mean age of patients was 25.4 ± 3.09 in the laminaria group and 26.4 ± 3.05 in the misoprostol group (21). Also, in the study of Allameh et al., there was no significant relationship between the group receiving Miso and the group receiving Miso + letrozole (11).
Also, based on the results of our study, the need for surgery and blood transfusion was zero in both groups. However, the number of cases requiring curettage, the mean length of hospital stay, and the duration of labor were statistically significant in the two groups, and the Miso + Lam group showed better results than the group of Miso alone. In a similar study to ours, Salari et al. reported that the cases requiring curettage during treatment, and the mean length of hospital stay was lower in the Miso + Lam group than in the group of Miso alone, and the difference was statistically significant (22). The number of curettages in the Miso + Lam group was 47.5% of the total 40 patients, and it was 12.5% of the total 40 patients in the group of Miso alone. Also, the duration of hospitalization of patients in the group receiving Miso + Lam was 1.48 ± 0.59 days and 1.63 ± 0.49 days in the group receiving Miso. Therefore, they stated that adding Lam to Miso to induce abortion in the second trimester of pregnancy not only reduces the time interval between the start of treatment and fetal expulsion but also reduces the need for curettage during treatment and also reduces treatment costs by decreasing the required Miso dose and the number of days hospitalized (22). On the other hand, in terms of the duration of patients’ stay in labor, the results of Paz et al. were similar to the present study, and the duration of labor in the group receiving Lam was shorter than in the group receiving Miso alone (23). While in a study comparing the effects of Lam and Miso alone in the second trimester of pregnancy, Sagiv et al. showed that Lam could not make a shorter time in labor compared to the group of misoprostol alone and that the labor time was shorter in the Miso group (24).
In addition, previous researches have revealed different results after vaginal consumption of Miso alone or in combination with other drugs. For instance, a study indicated 56.3% complete abortion after the first vaginal injection of 800 μg Miso, and 92.4% after the second dose (1600 μg) (25). Torky et al. demonstrated a complete abortion rate of 78% after 10 mg of letrozole administration twice a day for three days, followed by 800 μg of vaginal misoprostol administration in comparison to a rate of 39% after the misoprostol administration alone (26). Also, in Edelman et al.’s study, adding Lam to Miso at 19 weeks or more of GA exacerbated the effects of Miso, whereas these effects were not seen at GA s less than 19 weeks (27).
According to the results of our study, there was no significant complication in the patients, and there were several cases of fever and chills, diarrhea, and headache, which were resolved quickly. In the study by Salari et al., only one patient needed analgesics to control the side effects of the drug, which was in the group of Miso alone (22). In the study by Borgatta et al., adding Lam to Miso increased the use of analgesics (28). Also in our study, no patient required blood transfusion and surgery during treatment, which to other studies (22, 23, 27).
In general, according to the results of the present study, the simultaneous use of Miso and Lam is strongly recommended for abortion in the second trimester, and obstetricians can use a combination of these two drugs so that in addition to enjoying their beneficial effects, they can decrease the treatment costs of patients and save time. Furthermore, the present study had limitations, including the long time to obtain a sufficient sample size and excluding people with any underlying disease or risk factor led to bleeding and reduced the sample size. Therefore, to achieve more definite results, it is recommended to conduct similar studies in this field in larger sample sizes and consider the age and gender of the fetus (due to hormonal effects).
5.1. Conclusions
Our results showed that curettage cases, labor duration, and length of hospital stay decreased in the Miso + Lam group. Therefore, it can be concluded that adding Lam to the process of therapeutic abortion can help reduce labor time, duration of hospitalization, and the need for curettage.