1. Background
The Demodex mite is the most common ectoparasite on human skin. Two common species of human Demodex are Demodex folliculorum, typically found in hair follicles, and Demodex brevis, mainly located in sebaceous glands (1). This mite is found in almost the entire human skin and to a greater extent in the facial area, including meibomian glands of lid margins and eyelash follicles. It's reported that Demodex can cause the development or aggravation of some inflammatory skin diseases such as pustular folliculitis, perioral dermatitis, and rosacea or rosacea-like dermatitis (2-5). The anatomical position of the eyes seems to reduce the reach of facial cleansing agents to eyelashes, even if regularly used, and makes the situation even more suitable for Demodex growth and augmentation in lid margins.
It’s a matter of debate whether this colonization should be an area of concern and can cause pathologic consequences or, in contrast, Demodex should merely be considered as an innocent saprophytic organism living on the skin. Several studies aimed to answer this question; however, the literature evidence is controversial. Some studies have pointed to Demodex as the possible cause of blepharitis by showing a high prevalence of concomitance of these two conditions (6), while others found no difference in Demodex prevalence between blepharitis and non-blepharitis cases (7-9).
Studies have postulated the pathogenic role of Demodex by various mechanisms, including mechanical blockage and reactive hyper keratinization, granulomatous reaction, delayed hypersensitivity, and vector role for bacteria (4). However, the presence of Demodex in many asymptomatic individuals with no sign of blepharitis remains irreconcilable and highlights the conflicts.
Demodex is also transmissible by direct contact with the infested skin of an infected person or dust containing eggs of the mite, mainly by using shared bed linen (8, 10). The importance of knowing the clinical significance of Demodex is to clarify the necessity of treatment as well as the need to pay attention to preventing transmission, especially in conditions and places with a higher probability of transmission such as dormitories.
2. Objectives
Previous studies mentioned age and gender as two factors that are related to Demodex prevalence as well as the presence of attributable symptoms and blepharitis (11-13). In the present study, we aimed to evaluate the prevalence of ocular Demodex infestation in a large population of individuals of the same gender and range of age, in whom we expected a high transmission rate due to environmental factors as well as close contacts. Besides, we evaluated the correlation between Demodex and ocular clinical manifestations, helping to elucidate whether to consider it as a troublesome pathogen or an asymptomatic saprophyte.
3. Methods
In this cross-sectional study, 903 soldiers living in a military base in Iran in the summer of 2020 are investigated. After obtaining signed informed consent, participants were enrolled consequently for taking a comprehensive history of demographic as well as medical and ocular related data. They were excluded from the study for any of the following conditions: administration of topical medications other than artificial tears in the last 3 months, use of contact lens, active ocular infection or inflammation (other than blepharitis), presence of special established ocular surface diseases including Stevens-Jhonson syndrome, ocular cicatricial pemphigoid, and chemical burn, eyelid disorders such as ectropion and entropion and any prior ocular trauma or surgery.
All participants completed a questionnaire assessing ocular symptoms in the recent 3 months, including sand sensation, itching, redness, tearing, burning, tired eye, and blurred vision. Thereafter, they went through a complete slit-lamp examination followed by eyelash epilation. Documented ocular examination findings included presence or absence of conjunctival injection, oily scales, telangiectasia, cylindrical dandruff, and expression of meibomian glands in lid margins, as well as chalazion, madarosis, poliosis, and trichiasis.
A total of 4 eyelashes, one from each quadrant, were intended to be epilated from superior and inferior eyelids of the eye of each individual. Before epilation with sterile forceps, eyelashes were rotated in clockwise and counterclockwise directions several times to stimulate Demodex mites, if present, to come out of eyelash follicles, get visible, or remain stuck to the shaft of sampled eyelash by a greater chance. This is why lash manipulation has even been suggested as an alternative to lash epilation for examining the presence of Demodex by direct visualization in clinical settings (14, 15). However, eyelash epilation and subsequent microscopic examination remain a recommended method of diagnosis (15, 16).
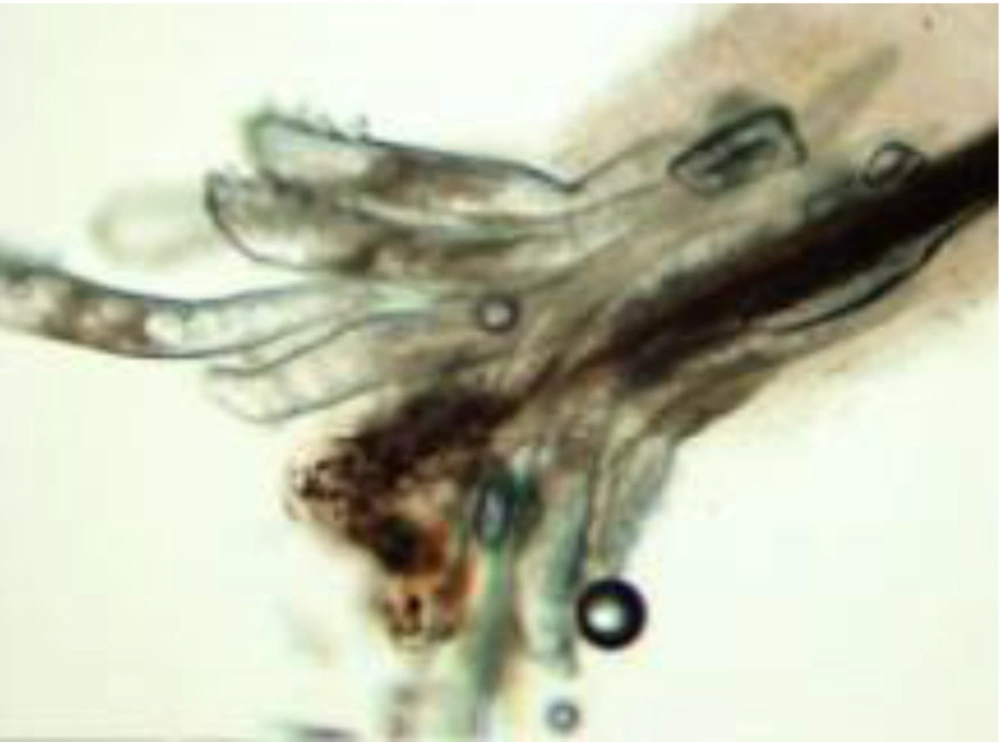
Each eyelash was placed on a sterile slide, and a drop of sterile immersion oil was put on the surface. Light microscopic evaluation was subsequently done at magnifications of ×40 and ×100, within 24 hours. Visualization of at least 1 mite in any of 4 eyelash samples taken from a single participant was considered as Demodex positive (Figure 1 and 2).
Data were analyzed to assess the overall prevalence of Demodex and identifying any significant correlation between signs, symptoms, and ocular demodicosis.
To present data, mean, standard deviation, frequency, and percent have been used. To evaluate the difference between the groups, the Chi-square test was employed. At the last step, we used binary logistic regression to assess the effects of signs and symptoms on Demodex. All statistical analyses were performed by SPSS (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.). Statistical significance was considered when P-value < 0.05.
4. Result
A total of 904 males with a mean age of 21 ± 2 years (ranging from 19 to 25 years) were included. The overall prevalence of Demodex infestation was 77.2% (86.8 and 26% in patients with and without blepharitis, respectively). Almost 50% of all cases showed at least one symptom related to eye discomfort, and 84.3% had at least a suggestive sign for blepharitis. Of 698 patients who were positive for Demodex, 58.6% reported eye discomfort, whereas it was experienced by 23.9% of Demodex negative participants, the difference was statistically significant (P-value < 0.001). Compared to Demodex's negative cases, all evaluated symptoms were found to have a higher prevalence in Demodex positive individuals; however, a significant association was only found with experiencing tired eye (P-value = 0.018). Comparative data of ocular symptoms in Demodex positive and negative groups are shown in Table 1 and 2.
aBased on t-test
bBased on Chi-square
| Demodex, No. (%) | OR | 95% CI | P-Value a | ||
|---|---|---|---|---|---|
| No | Yes | ||||
| Discomfort | |||||
| No | 156 (76.1) | 289 (41.4) | 1 | ||
| Yes | 49 (23.9) | 409 (58.6) | 3.145 | 1.724 - 5.736 | < 0.001 |
| Sand sensation | |||||
| No | 191 (93.2) | 506 (72.5) | 1 | ||
| Yes | 14 (6.8) | 192 (27.5) | 1.303 | 0.656 - 2.587 | 0.45 |
| Itching | |||||
| No | 177 (86.3) | 459 (65.8) | 1 | ||
| Yes | 28 (13.7) | 239 (34.2) | 0.806 | 0.441 - 1.472 | 0.482 |
| Redness | |||||
| No | 201 (98.0) | 565 (80.9) | 1 | ||
| Yes | 4 (2.0) | 133 (19.1) | 2.901 | 0.844 - 9.974 | 0.091 |
| Burning | |||||
| No | 187 (91.2) | 528 (75.6) | 1 | ||
| Yes | 18 (8.8) | 170 (24.4) | 0.707 | 0.37 - 1.352 | 0.294 |
| Tearing | |||||
| No | 193 (94.1) | 536 (76.8) | 1 | ||
| Yes | 12 (5.9) | 162 (23.2) | 1.464 | 0.724 - 2.958 | 0.288 |
| Crusting | |||||
| No | 198 (96.6) | 589 (84.4) | 1 | ||
| Yes | 7 (3.4) | 109 (15.6) | 1.403 | 0.58 - 3.394 | 0.452 |
| Tired_eye | |||||
| No | 199 (97.1) | 538 (77.1) | 1 | ||
| Yes | 6 (2.9) | 160 (22.9) | 3.216 | 1.225 - 8.446 | 0.018 |
| Blurred_vision | |||||
| No | 196 (95.6) | 593 (85.0) | 1 | ||
| Yes | 9 (4.4) | 105 (15.0) | 0.684 | 0.299 - 1.568 | 0.37 |
a Based on Chi-square
Prevalence of blepharitis was reported 94.7% and 48.8% in Demodex positive and Demodex negative groups, respectively. According to the chi-square test, blepharitis prevalence was significantly different between the two groups (P-value < 0.001); however, further regression analysis indicated a lower level of significance (P-value = 0.444, OR = 0.67). Among all related signs of blepharitis, conjunctival injection (P-value < 0.001, OR = 17) and corneal vascularization (P-value < 0.001, OR = 5.85) were significantly associated with Demodex presence. As shown in Table 3, the prevalence of all blepharitis related signs was higher in Demodex positive group. Besides, conjunctival injection, expression of Meibomian glands, and lid margin telangiectasia were the most prevalent signs in Demodex positive subjects.
| Demodex, No. (%) | OR | 95% CI | P-Value a | ||
|---|---|---|---|---|---|
| No | Yes | ||||
| Blepharitis | |||||
| No | 105 (51.2) | 37 (5.3) | 1 | ||
| Yes | 100 (48.8) | 661 (94.7) | 0.677 | 0.25 - 1.836 | 0.444 |
| Conj_inj | |||||
| No | 191 (93.2) | 70 (10.0) | 1 | ||
| Yes | 14 (6.8) | 628 (90.0) | 17.018 | 74.291 - 389.096 | 0 |
| Expression of the meibomian gland | |||||
| No | 124 (60.5) | 288 (41.3) | 1 | ||
| Yes | 81 (39.5) | 410 (58.7) | 1.243 | 0.521 - 2.967 | 0.624 |
| Oily_scales | |||||
| No | 189 (92.2) | 531 (76.1) | 1 | ||
| Yes | 16 (7.8) | 167 (23.9) | 0.809 | 0.29 - 2.26 | 0.686 |
| Lid margin telangiectasia | |||||
| No | 152 (74.1) | 471 (67.5) | 1 | ||
| Yes | 53 (25.9) | 227 (32.5) | 0.535 | 0.252 - 1.133 | 0.102 |
| Cylindrical_dandruf | |||||
| No | 159 (77.6) | 480 (68.8) | 1 | ||
| Yes | 46 (22.4) | 218 (31.2) | 0.955 | 0.411 - 2.223 | 0.915 |
| Corneal_vascularization | |||||
| No | 183 (89.3) | 498 (71.3) | 1 | ||
| Yes | 22 (10.7) | 200 (28.7) | 5.851 | 2.448 - 13.984 | 0 |
| Trichiasis | |||||
| No | 145 (70.7) | 473 (67.8) | 1 | ||
| Yes | 60 (29.3) | 225 (32.2) | 0.624 | 0.267 - 1.461 | 0.277 |
| Poliosis | |||||
| No | 199 (97.1) | 573 (82.1) | 1 | ||
| Yes | 6 (2.9) | 125 (17.9) | 1.598 | 0.42 - 6.077 | 0.491 |
| Madarosis | |||||
| No | 197 (96.1) | 600 (86.0) | 1 | ||
| Yes | 8 (3.9) | 98 (14.0) | 2.549 | 0.697 - 9.316 | 0.157 |
| Chalazion | |||||
| No | 200 (97.6) | 637 (91.3) | 1 | ||
| Yes | 5 (2.4) | 61 (8.7) | 0.478 | 0.07 - 3.257 | 0.451 |
a Based on Chi-square
5. Discussion
The main goal of the present survey was to reveal the overall prevalence of Demodex infestation among the studied population, which was reported to be 77.2%. This high prevalence is consistent with the results of studies by de Venecia et al. and Bhandari et al., who reported a prevalence of 73% and 68%, respectively, for Demodex (17, 18). However, some studies reported values as low as 41, 27.4, and 26.1% (7, 8, 19).
The high prevalence of this mite in the present study can be attributed to the large sample size as well as particular living conditions of participants and shared pillows and bedsheets in dormitories, which in turn made the mite transmission easier and more probable. We also found a remarkable, meaningful higher prevalence of parasite among subjects with symptoms of ocular discomfort compared to asymptomatic cases, whereas a noticeable higher prevalence of Demodex among patients with at least a sign of chronic blepharitis (86.8%) was not statistically significant.
Lopez et al. investigated patients with blepharitis and reported a prevalence of Demodex 83.7%, which is consistent with our findings (6). In the present study, 58.6% of infected patients complained of at least one ocular symptoms. Similarly, Sędzikowska et al. reported that 64% of Demodex positive patients were symptomatic (20). Kabatas et al. found that ocular redness, tearing, and foreign body sensation were not suggestive for Demodex infestation, while itching was the only symptom with meaningfully higher prevalence in Demodex positive individuals (21). In our study, although itching was the most common symptom in the Demodex positive group, most of the participants (65%) did not report this symptom, while a considerable number of Demodex negative cases (86%) reported experiencing this symptom. So, in contrast to the study by Kebatas et al., in the present study itching was not a strongly correlated symptom, while the tired eye was.
In the current study, the most prevalent sign reported by Demodex positive patients was conjunctival injection, followed by lid margin telangiectasia and cylindrical dandruff. Despite their high prevalence, lid margin telangiectasia and cylindrical dandruff did not seem to have a significant correlation with Demodex presence and, as shown in Table 3, a considerable number of patients without Demodex infestation also presented these signs. In ocular demodicosis, conjunctival injection is the result of conjunctival irritation, which is believed to occur secondary to Meibomian gland dysfunction (14), concomitant bacterial pathogens carried by Demodex, or delayed hypersensitivity reaction to mite proteins and debris (10, 22-25).
Corneal vascularization was another ocular sign that had a significant correlation with Demodex infection in the present study. In an interventional case series in patients with Demodex blepharitis who also exhibited corneal abnormalities, Kheirkhah et al. documented noticeable regression of corneal superficial vascularization after treatment for Demodex mite (26). Luo et al. also reported an early resolution of refractory keratitis and corneal vascularization after treating Demodex mite and suggested that this early response occurred before complete eradication of mite, indicates that corneal presentations related to Demodex infestation are mainly caused by immune response mechanisms (27). Based on our results, we suggest considering Demodex as a probable cause in eyes with evidence of corneal vascularization, especially in the absence of clear signs of blepharitis, as these eyes can be easily and mistakenly treated for other presumed pathogens for a long time. Therefore, eyelash sampling and looking for mites or considering mite treatment seem reasonable and are recommended in these cases.
The higher prevalence of all evaluated ocular signs and symptoms in Demodex positive participants, compared to Demodex negative group, indicates that these signs and symptoms may be common in clinical settings of ocular demodicosis, but further, they are not all highly suggestive for this mite and their absence should not be considered as a hint making Demodex diagnosis significantly less probable.
As a whole, our study demonstrates that Demodex infestation may be responsible, at least in some people, for ocular discomfort and especially tired eye sensation, but in general, is not necessarily correlated with blepharitis. Many individuals infested by this mite demonstrate no clinical sign, although they may experience several ocular symptoms.
This finding supports the notion that the number of mites may be of importance to play a role in manifesting clinical signs of blepharitis. In other words, a smaller number of mites may be enough to cause ocular discomfort, while ocular signs may present in a smaller number of patients who are infected by a larger number of mites. This issue highlights the importance of evaluating the cumulative effect of Demodex mite on ocular signs. This finding can also be attributed to the high probability of recent transmission among our studied population, which may lead to the early sensation of different feelings in eyelids, while it might take a longer time to cause changes in tissues, leading to the manifestation of visible signs of blepharitis in the same eye. This probability highlights the necessity of following up patients.
The positive aspects of this study include the large number as well as the narrow age range of evaluated subjects. To the best of our knowledge, such a large group of cases has not been investigated so far for the presence of Demodex blepharitis. Limitations include a lack of quantitative data regarding mite load in eyelashes and a lack of comparative data of blepharitis signs during the time. Further prospective, quantitative studies are needed for delighting the role of Demodex in ocular diseases.