Abstract
Background:
Informal payments, as one of the components of out-of-pocket (OOP) payments, are often a form of corruption and outside the official bill. The purpose of the present study was to investigate the frequency of informal payments for inpatient services and its related factors in Tehran, Iran.Methods:
In this cross-sectional study, the samples included 450 patients who were admitted to hospital’s clinics affiliated to Shahid Beheshti University of Medical Sciences in Tehran, to receive follow-up and post-surgical care. After obtaining patient consent, data were collected via a 28-item questionnaire included two parts of patient’s demographic characteristics and informal payments experience that it’s validity and reliability were confirmed. Data were analyzed using descriptive statistics and regression analyses in SPSS 16 software.Results:
The findings showed 21.1% of the patients had informal payments, paid voluntarily, mostly in cash, for service’s staff, in public hospitals, after discharge and, due to the employees' proper behavior and attention. The average informal payments per patient were 5,304,630 IRR (175.4 USD). There was no significant relationship between the informal payment behavior and the patient demographics characteristics (P > 0.05).Conclusions:
Despite the efforts made in the HTP to eliminate informal payments in inpatient services, the goal has not been fully realized. A part of the payments was paid at the provider's request and before the patient's admission that these compulsory informal payments are illegal and unethical and therefore, must be controlled and eradicated. Policymakers can take steps to reduce informal payments by improving the healthcare quality, supervision, setting salary and benefits, enforcing laws, and increasing staff incentives.Keywords
1. Background
Out-of-pocket (OOP) payments are one of the most common sources of health systems financing around the world, in which the patient pays the cost of purchasing and consuming services and goods in cash. OOPs are not reimbursable by insurers or third parties (1) and include official co-payments, payments for “bought and brought goods” (e.g., for pharmaceuticals bought in the pharmacy and brought to the hospital) and informal payments (2).
Informal payments are illegal and often a form of corruption (2, 3). Patients or their relatives make these payments to health care providers out of the official bills (4). Informal payments have the following characteristics: a) not registered; b) not necessarily related to treatment; c) paid before, during, and after the treatment process; and d) may be initiated by the hospital staff or patient (2). In addition, these payments are made in cash or non-cash form (5).
Informal patient payments for health services are common in many health systems, especially in developing countries (6). Evidence indicates that these payments occur in at least 22 African, Asian and European countries (7). Information on the extent of informal payments is negligible due to their illegal nature, but studies have shown that between 10% and 45% of total health expenditures in some low-income countries relates to this type of payment (8). Previous studies in Iran have reported different frequency of informal payments in the health system where amounts of informal payments ranged from 5.93% to 63.8%. (6, 7, 9-13). Recently, the findings of a systematic review showed that the amount of informal payments was around 35% (14). Lack of public resources to finance health services, lack of adequate monitoring and supervision, poor complaints handling, low salaries and benefits to health care providers, poor management, delay of insurance companies in reimbursing costs, unreliability of tariffs and socio-cultural characteristics are among the factors contributing to informal payments (5, 10).
Evidence suggests that informal payments have a negative impact on access and use of health care, equity, efficiency, quality, and patient-doctor relationship (15). These payments increase the cost of care for patients, especially the poor people, and cause some people to discontinue using health services or treatment process (16).
There are several strategies to decrease negative outcomes of informal payments, such as to increase rewards to providers, to increase the government’s share of health expenditures, to put emphasis on the rules and punishment for flouting them, as well as behavior change (17). In Iran, the Ministry of Health and Medical Education began a series of reforms under the ‘Health Transformation Plan’ (HTP) since 2014 with a particular focus on financial protection. This plan consists of 8 service packages (18) and one of it’s goals is to reduce and eliminate informal payments in health system (19). In this regard, the government is committed to reducing informal payments by increasing medical tariffs, increasing its own share in health system financing and expanding insurance coverage (13).
It was expected that the implementation of this reform would reduce the frequency of informal payments. Progress in implementing reforms and the extent to which the goals have been achieved should be monitored and evaluated regularly. Considering the lack of official statistics, this study was conducted to investigate the frequency of informal payments in hospital services two years after the implementation of the HTP in order to provide feedbacks to the policy makers and managers of the country’s health system.
2. Methods
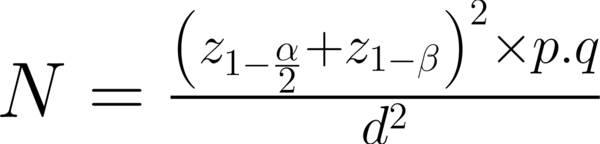
This cross-sectional study was carried out in four public hospitals affiliated to Shahid Beheshti University of Medical Sciences in Tehran in 2016. Due to the higher frequency of informal payments in surgical services (7, 11, 12), the study population comprised all patients who had been referred to the hospital clinics for follow-up and post-surgical care. According to studies conducted in Iran, the frequency of informal payments was reported to be 30% on an average (6, 10, 13). Thus, according to the following formula (P = 0.3, q = 0.7, d = 0.07), the number of study samples was estimated as 450 patients with the confidence level of 95% and an error of less than 5%.
Among the total number of 450 patients, 155 were from Hospital A, 120 from Hospital B, 90 from Hospital C, and 85 from Hospital D, which were selected on the basis of the number of outpatients in each hospital. The samples were selected using convenience sampling method. After receiving consent from the patients older than 18 years to participate in the study, they were asked questions using an interview method. The patient interview was conducted in the clinic waiting room. In the case of disabled people and children, the interview was conducted with their attendants.
Data were collected using a questionnaire. The questionnaire included two parts. The first section contained questions about the patient’s demographic information and the second was related to informal payments experience during the last 12 months prior the survey. This part had 16 questions such as the amount, place, time, and type of informal payment. The study instrument was designed based on the previous studies (11, 20-22).
To determine the content validity of the designed tool, the comments of 15 experts (in the fields of health service management and medical ethics) were received and necessary corrections were made based on these. The test-retest and Cronbach’s alpha was used to determine the reliability of the instrument and the internal consistency. The test-retest of the questionnaire with ICC (0.805) showed a significant correlation. The internal consistency coefficient of the questions was 0.736 (Cronbach’s alpha coefficient ≥ 0.7), from which it can be concluded that the study questionnaire had a satisfactory reliability.
The data were analyzed using descriptive statistics, simple logistic regression analysis and multiple logistic regression analysis in SPSS 16 software. Logistic regression analysis was used to describe the effect of each predictor (demographic variables) of payment behavior in the model. The Rial to US dollar exchange rate in the year of the study was 1.00 USD = 30,240 IRR (23). This study was approved by the Research Ethics Committee of Shahid Beheshti University of Medical Sciences.
3. Results
Most of the patients who participated in this study were female (57.6 %) and urban residents (94 %). Most of them (31.1 %) were in the age group of 30 - 40 years and had a basic level of education (35.8 %). In addition, 91% of patients were insured.
Patient experience of informal payments is shown in Table 1. Of the 450 patients, 21.1% (N = 95) had made informal payments, mostly (64.4%) at public hospitals. The most common form of informal payments was cash (52.4%) and most of the patients (66.3%) paid after discharge from hospital. Physicians received about 30% of the payments and other hospital personnel, such as nurses and administrative and service staff, about 70%. Most of the payments (83.5%) were made voluntarily. In 20 cases, payments were made at the request of the care providers, mostly to the patients themselves. Among the patients who did not pay informally (N = 355), 17 people had also encountered requests for informal payments which they had turned down. Moral and legal beliefs and financial inability were the most important reasons for non-payment.
Patients’ Experiences of Informal Payments (N = 95)a
| Patient Experience | No. (%) | Total Payments |
|---|---|---|
| Place of payment | 104 | |
| Physician’s office | 20 (19.2) | |
| Public Hospital | 67 (64.4) | |
| Private Hospital | 10 (9.7) | |
| Clinic | 5 (4.8) | |
| Others | 2 (2.0) | |
| Payment forms | 105 | |
| In-cash | 55 (52.4) | |
| Goods | 31 (29.6) | |
| Commitment to work | 2 (1.9) | |
| Others | 17 (16.2) | |
| Payment time | 101 | |
| Before admission | 15 (14.9) | |
| During hospitalization | 19 (18.9) | |
| After discharge | 67 (66.3) | |
| Who receive? | 111 | |
| Physician | 33 (29.8) | |
| Nurse | 23 (20.8) | |
| Administrative Staff | 15 (13.5) | |
| Service staff | 40 (36.0) | |
| How to pay? | 97 | |
| Voluntary | 81 (83.5) | |
| Request of the provider | 16 (16.5) | |
| How did the provider request? | 20 | |
| Direct payment request | 10 (50.0) | |
| Different and unfriendly request | 4 (20.0) | |
| Keep waiting or delay in care | 5 (25) | |
| Order to buy medicine by the patient | 1 (5.0) | |
| Reasons for not paying | 31 | |
| Lack of need because of the quantity and quality of service | 1 (3.2) | |
| Dissatisfaction with the service | 2 (6.4) | |
| Lack of need for additional services | 1 (3.2) | |
| Lack of financial capability | 10 (32.2) | |
| Lack of moral and legal belief in these payments | 16 (51.6) | |
| Lack of familiarity with this payment | 1 (3.2) |
Table 2 shows the reasons for making informal payments from the patients’ perspective. The most important reasons for informal payments were to ensure proper behavior and attention of hospital staff (40.9%), followed by thanking the doctors and medical staff for satisfactory treatment (24%).
Reasons for Paying Informal Payments (N = 95)a
| Reasons | No. (%) |
|---|---|
| Having enough money | 1 (0.5) |
| Low salaries of employees | 2 (1.0) |
| Because everyone does it | 4 (2.0) |
| Reduce waiting time from referral to hospitalization | 11 (5.8) |
| Response to a doctor or medical staff request for informal payments | 12 (6.2) |
| To receive more quality services and access to better equipment or drugs | 17 (8.9) |
| Fear of providing below standard care | 20 (10.5) |
| Thanks to the doctor and medical staff for the satisfaction of the treatment | 46 (24.0) |
| Proper employees’ behavior and attention | 78 (40.9) |
The total monetary value of informal payments was 286,450,000 IRR (9,472 USD). The average informal payment for each patient was approximately 5,304,630 IRR (175 USD). The minimum and maximum amounts of informal payments were 100,000 IRR (3.3 USD) and 40,000,000 IRR (1,323 USD), respectively. It was found that only 50% of the patients were aware of their hospital costs prior to admission.
To investigate the effect of demographic variables on payment behavior, simple logistic regression was used, for which the dependent variable was paying behavior (yes/no). The results of the logistic regression analysis showed that none of the variables had an effect on the payment behavior (P > 0.05) (Table 3).
The Impact of Demographic Variables on Payment Behavior
| Variable | OR | SE | Sig |
|---|---|---|---|
| Hospital | 0.228 | ||
| A | 1.724 | 0.296 | |
| B | 1.443 | 0.327 | |
| C | 1.016 | 0.355 | |
| D | - | - | |
| Gender | 0.587 | ||
| Female | 1.136 | 0.235 | |
| Male | - | - | |
| Marital status | 0.103 | ||
| Single | 1.534 | 0.263 | |
| Married | - | - | |
| Job status | 0.835 | ||
| Employed | 1.050 | 0.233 | |
| Unemployed | - | - | |
| Age group | 0.835 | ||
| < 40 | 1.022 | 0.233 | |
| > 40 | - | - | |
| Level of Education | 0.327 | ||
| Non-academic | 1.294 | 0.263 | |
| Academic | - | - | |
| Residence area | 0.091 | ||
| Urban | 3.523 | 0.744 | |
| Rural | - | - | |
| Insurance coverage | 0.731 | ||
| Yes | 1.152 | 0.411 | |
| No | - | - | |
| Type of insurance | 0.992 | ||
| Health insurance | 0.984 | 0.260 | |
| Relief Committee | 0.00 | 20096.5 | |
| Armed Forces | 0.907 | 0.664 | |
| Other insurance | 1.815 | 1.234 | |
| Social Security | - | - | |
| Income level, IRR | 0.161 | ||
| > 20,000,000 | 1.437 | 0.258 | |
| < 20,000,000 | - | - |
The simultaneous effect of demographic variables on the payment behavior was investigated using multiple logistic regression analysis. In this analysis, variables with significant levels of less than 0.2 were entered into the model. No significant relationship was found between the behavior of informal payments and marital status, place of residence, and income level of patients (P > 0.05) (Table 4).
The Simultaneous Effect of Demographic Variables on the Payment Behavior
| Variable | OR | SE | Sig | |
|---|---|---|---|---|
| Marital status | Single | 1.456 | 0.265 | 0.155 |
| Married | - | - | ||
| Residence area | Urban | 3.187 | 0.747 | 0.121 |
| Rural | - | - | ||
| Income level, IRR | > 20,000,000 | 1.338 | 0.261 | 0.264 |
| < 20,000,000 | - | - |
4. Discussion
The study aimed at investigating the frequency of informal payments in hospital services and it’s findings showed that 21.1% of the patients had made informal payments. Investigating the informal payments in Iran’s health system over the last decade has been a topic of interest to researchers and various studies have reported that these payments ranged from 6% to 64% (6, 9-13). Differences in frequency rates can be attributed to the study environment (hospital or physician’s office), hospital ownership (public or private), survey level (individual or household), survey time (during or after hospitalization), estimation method, and the type of service. Despite the implementation of the HTP and the dramatic increase in medical tariffs, there are still informal payments in the health system, indicating that the HTP has not achieved the goal of eliminating these payments.
The frequency of informal payment was also reported in studies conducted in Turkey (29%) (24), Greece (32.4%) (25), Bulgaria (33%) (26), Lithuania (50%) (27), and Moldova (82%) (28), that were higher than our study.
The highest number of patients were exposed to informal payments in public hospitals (64.4%), which is consistent with the findings of previous studies (24, 29, 30). This can be attributed to the pattern of referrals and more utilization of public hospital services that increases the probability of frequency of informal payments. According to our findings, most patients were from the middle income group of the community, which is an important factor for the use of public hospital services (9).
The most common form of informal payments was in cash, which is in line with the findings of previous studies (6, 9, 10, 24, 31-33). In some studies, most of the informal payments have been made in the form of non-monetary gifts (28, 34, 35). It can be concluded that the cultural, economic, and social status of the regions affect the forms of informal payments.
In this study, most payments occurred after the discharge. Studies conducted in Turkey (24) and Lithuania (27) are consistent with our findings. Most payments were voluntary (83.5%) and the most important reasons for payment were thanking the doctors and hospitals for their services and ensuring proper behavior of the staff. Society and culture also have an impact on this matter. Iranians always like to appreciate someone who has done a service to them.
In this study, most of the informal payments were found to be received by service personnel (36.03%) and physicians (29.8%). Similar results have been reported in other various studies (9, 10, 36, 37). Most of the patients believed that the salaries of the service personnel would not be enough for their lives; therefore, they voluntarily gave money to help them. However, some physicians asked patients with severe problems to pay informally before undertaking treatment and patients were forced to accept this request for health reasons although sometimes they were opposed it.
This study found that 16.5% of the payments were made at the request of the care providers. The study of Vian et al. is consistent with the findings of this study (28). These forms of payments (requested by the care provider) can limit access of patients to appropriate services because not all of them are able to pay. Applying stricter rules and regulations can prevent a direct request from the care provider.
The research findings showed that only 50% of patients were informed of their hospital costs before using the services. The lack of familiarity with health care costs would provide opportunities for care providers to gain further benefits. Due to the bureaucracy governing the health care system, it is not always possible for the patients to distinguish informal payments from the official ones. Therefore, if patients are aware of the services and the prices associated with them at the health centers, they will be faced with very little informal payments at the centers.
There was no significant relationship between demographic variables and payment behavior. Some studies have reported a meaningful relationship between informal payment behavior with gender, age, educational level, place of residence, health insurance coverage and household economic status (6, 13, 22, 38-42). This discrepancy in the results can be attributed to the study setting (hospital or household), the type of surveyed patients, country of study, and the data analysis methods.
This study had some limitations. Due to the sensitive nature of the issue, some patients were conservative in narrating their experiences of informal payments. Due to the study design, patients needed to recall their experience from a recent year. Therefore, there may be a recall bias. Although informal payment is not a recurring experience for patients, it can be said that the recall bias has not been very serious.
4.1. Conclusions
Despite the efforts made in the HTP to eliminate informal payments in inpatient services, the goals have not been fully realized. Voluntarily payments, mostly due to staff appreciation, are not unethical; however, a part of the payments was paid at the provider’s request and before the patient's admission. These compulsory informal payments are illegal and unethical and therefore, must be controlled and eradicated. Policymakers can take steps to reduce informal payments by improving the healthcare quality, supervision, setting salary and benefits, enforcing laws, and increasing staff incentives.
Acknowledgements
References
-
1.
Piroozi B, Rashidian A, Moradi G, Takian A, Ghasri H, Ghadimi T. Out-of-Pocket and Informal Payment Before and After the Health Transformation Plan in Iran: Evidence from Hospitals Located in Kurdistan, Iran. Int J Health Policy Manag. 2017;6(10):573-86. [PubMed ID: 28949473]. https://doi.org/10.15171/ijhpm.2017.16.
-
2.
Arsenijevic J, Pavlova M, Groot W. Out-of-pocket payments for health care in Serbia. Health Policy. 2015;119(10):1366-74. [PubMed ID: 26298693]. https://doi.org/10.1016/j.healthpol.2015.07.005.
-
3.
World Health Organization. Health systems financing: the path to universal coverage. 2016.
-
4.
Chereches RM, Ungureanu MI, Sandu P, Rus IA. Defining informal payments in healthcare: a systematic review. Health Policy. 2013;110(2-3):105-14. [PubMed ID: 23410757]. https://doi.org/10.1016/j.healthpol.2013.01.010.
-
5.
European Commission. Study on Corruption in the Healthcare Sector: Office of the European Union. 2013. Available from: http://europa.eu.
-
6.
Jafari A, Ravangard R, Heidari F, Roshani M, Hadian M, Mohammadi M. Informal payment in health settings: a survey of teaching hospitals. Int J Hospital Res. 2015;4(2):83-8.
-
7.
Parsa M, Aramesh K, Nedjat S, Kandi MJ, Larijani B. Informal Payments for Health Care in Iran: Results of a Qualitative Study. Iran J Public Health. 2015;44(1):79-88. [PubMed ID: 26060779].
-
8.
Nekoeimoghadam M, Esfandiari A, Ramezani F, Amiresmaili M. Informal payments in healthcare: a case study of kerman province in iran. Int J Health Policy Manag. 2013;1(2):157-62. [PubMed ID: 24596856]. https://doi.org/10.15171/ijhpm.2013.28.
-
9.
Vafaei Najar A, Ebrahimipour H, Pourtaleb A, Esmaily H, Jafari M, Nejatzadegan Z, et al. At first glance, informal payments experience on track: why accept or refuse? Patients' perceive in cardiac surgery department of public hospitals, northeast of Iran 2013. BMC Health Serv Res. 2017;17(1):205. [PubMed ID: 28292289]. https://doi.org/10.1186/s12913-017-2108-4.
-
10.
Aboutorabi A, Ghiasipour M, Rezapour A, Pourreza A, Sarabi Asiabar A, Tanoomand A. Factors affecting the informal payments in public and teaching hospitals. Med J Islam Repub Iran. 2016;30:315. [PubMed ID: 27390685].
-
11.
Ghiasipour M, Poorreza A, Arab M, Mahmoodi M, Abutorabi A. The analysis of informal payments among hospitals covered under Tehran University of Medical Sciences (TUMS) 2009. Hospital. 2011;10(3).
-
12.
Khodamoradi A, Rashidian A, Aghlmand S, Arab M, Moini M. Informal payments and its related factors in Urmia hospitals. Hakim Health Sys Res. 2015;17(4):313-21.
-
13.
Meskarpour-Amiri M, Arani AA, Sadeghi H, Agheli-Kohnehshahri L. Socioeconomic factors affecting informal payments in the health sector. Transylvanian Rev Administ Sci. 2016;12(47):116-28.
-
14.
Mirabedini SA, Fazl Hashemi SME, Sarabi Asiabar A, Rezapour A, Azami-Aghdash S, Hosseini Amnab H. Out-of-pocket and informal payments in Iran's health care system: A systematic review and meta-analysis. Med J Islam Repub Iran. 2017;31:70. [PubMed ID: 29445699]. https://doi.org/10.14196/mjiri.31.70.
-
15.
Hasanpoor E, Janati A, Salehi A, Sokhanvar M, Ebrahimzadeh J. Under the table in health care system: A case report in Iran. Int J Hospital Res. 2014;3(3):155-8.
-
16.
Vian T, Burak LJ. Beliefs about informal payments in Albania. Health Policy Plan. 2006;21(5):392-40.
-
17.
Miller K, Vian T. Strategies for reducing informal payments. Sterling: Kumarian Press; 2010.
-
18.
Ferdosi M, Kabiri S, Keyvanara M, Yarmohammadian MH. Challenges of Iran Health Transformation Plan about Inpatients Payment: Viewpoint of Experts. Health Scope. 2017;6(3).
-
19.
Moradi-Lakeh M, Vosoogh-Moghaddam A. Health Sector Evolution Plan in Iran; Equity and Sustainability Concerns. Int J Health Policy Manag. 2015;4(10):637-40. [PubMed ID: 26673172]. https://doi.org/10.15171/ijhpm.2015.160.
-
20.
Stepurko T, Pavlova M, Gryga I, Groot W. To pay or not to pay? A multicountry study on informal payments for health-care services and consumers' perceptions. Health Expect. 2015;18(6):2978-93. [PubMed ID: 25292329]. https://doi.org/10.1111/hex.12281.
-
21.
Stepurko T, Pavlova M, Gryga I, Groot W. Informal payments for health care services – Corruption or gratitude? A study on public attitudes, perceptions and opinions in six Central and Eastern European countries. Commun Post Commun Stud. 2013;46(4):419-31. https://doi.org/10.1016/j.postcomstud.2013.08.004.
-
22.
Baji P, Pavlova M, Gulacsi L, Groot W. Exploring consumers' attitudes towards informal patient payments using the combined method of cluster and multinomial regression analysis--the case of Hungary. BMC Health Serv Res. 2013;13:62. [PubMed ID: 23414488]. https://doi.org/10.1186/1472-6963-13-62.
-
23.
Central bank of Islamic Republic of Iran. Exchange Rate Iran. 2015. Available from: http://www.cbi.ir/exrates/rates_fa.aspx.
-
24.
Tengilimoglu D, Guzel A, Toygar A, Akinci F, Dziegielewski SF. Informal Payments in Health Systems: Purpose and Occurrences in Turkey. J Soc Serv Res. 2015;41(5):684-96. https://doi.org/10.1080/01488376.2015.1058880.
-
25.
Souliotis K, Golna C, Tountas Y, Siskou O, Kaitelidou D, Liaropoulos L. Informal payments in the Greek health sector amid the financial crisis: old habits die last. Eur J Health Econ. 2016;17(2):159-70. [PubMed ID: 25644967]. https://doi.org/10.1007/s10198-015-0666-0.
-
26.
Atanasova E, Pavlova M, Moutafova E, Rechel B, Groot W. Informal payments for health services: the experience of Bulgaria after 10 years of formal co-payments. Eur J Public Health. 2014;24(5):733-9. [PubMed ID: 24192398]. https://doi.org/10.1093/eurpub/ckt165.
-
27.
Riklikiene O, Jarasiunaite G, Starkiene L. Informal patient payments in publicly financed healthcare facilities in Lithuania. Scand J Public Health. 2014;42(6):488-96. [PubMed ID: 24906553]. https://doi.org/10.1177/1403494814538125.
-
28.
Vian T, Feeley FG, Domente S, Negruta A, Matei A, Habicht J. Barriers to universal health coverage in Republic of Moldova: a policy analysis of formal and informal out-of-pocket payments. BMC Health Serv Res. 2015;15:319. [PubMed ID: 26260324]. https://doi.org/10.1186/s12913-015-0984-z.
-
29.
Kaitelidou D, Tsirona CS, Galanis PA, Siskou O, Mladovsky P, Kouli EG, et al. Informal payments for maternity health services in public hospitals in Greece. Health Policy. 2013;109(1):23-30. [PubMed ID: 23153567]. https://doi.org/10.1016/j.healthpol.2012.10.012.
-
30.
Pavel MS, Chakrabarty S, Gow J. Cost of illness for outpatients attending public and private hospitals in Bangladesh. Int J Equity Health. 2016;15(1):167. [PubMed ID: 27724955]. https://doi.org/10.1186/s12939-016-0458-x.
-
31.
Ungureanu MI, Litan CM, Rus IA, Chereches RM. A brief insight into the study of informal health care payments in Romania. Transylvanian Rev Administ Sci. 2013;9(39):212-9.
-
32.
Gordeev VS, Pavlova M, Groot W. Informal payments for health care services in Russia: old issue in new realities. Health Econ Policy Law. 2014;9(1):25-48. [PubMed ID: 23688590]. https://doi.org/10.1017/S1744133113000212.
-
33.
Syhakhang L, Soukaloun D, Tomson G, Petzold M, Rehnberg C, Wahlstrom R. Provider performance in treating poor patients--factors influencing prescribing practices in lao PDR: a cross-sectional study. BMC Health Serv Res. 2011;11:3. [PubMed ID: 21210989]. https://doi.org/10.1186/1472-6963-11-3.
-
34.
Stepurko T, Pavlova M, Gryga I, Murauskiene L, Groot W. Informal payments for health care services: The case of Lithuania, Poland and Ukraine. J Eurasian Stud. 2015;6(1):46-58. https://doi.org/10.1016/j.euras.2014.11.002.
-
35.
Atanasova E. Formal and informal patient payments for public health care services in Bulgaria. Maastricht University; 2014.
-
36.
Moldovan A, Van de Walle S. Gifts or bribes? Attitudes on informal payments in Romanian health care. Public Integr. 2013;15(4):385-402.
-
37.
Maini R, Hotchkiss DR, Borghi J. A cross-sectional study of the income sources of primary care health workers in the Democratic Republic of Congo. Hum Resour Health. 2017;15(1):17. [PubMed ID: 28219445]. https://doi.org/10.1186/s12960-017-0185-4.
-
38.
Tomini S, Maarse H. How do patient characteristics influence informal payments for inpatient and outpatient health care in Albania: results of logit and OLS models using Albanian LSMS 2005. BMC Public Health. 2011;11:375. [PubMed ID: 21605459]. https://doi.org/10.1186/1471-2458-11-375.
-
39.
Habibov N, Cheung A. Revisiting informal payments in 29 transitional countries: The scale and socio-economic correlates. Soc Sci Med. 2017;178:28-37. [PubMed ID: 28192744]. https://doi.org/10.1016/j.socscimed.2017.02.003.
-
40.
Ozgen H, Sahin B, Belli P, Tatar M, Berman P. Predictors of informal health payments: the example from Turkey. J Med Syst. 2010;34(3):387-96. [PubMed ID: 20503624].
-
41.
Danyliv A, Pavlova M, Gryga I, Groot W. Preferences for physician services in Ukraine: a discrete choice experiment. Int J Health Plann Manage. 2015;30(4):346-65. [PubMed ID: 24399636]. https://doi.org/10.1002/hpm.2239.
-
42.
Baji P, Pavlova M, Gulacsi L, Farkas M, Groot W. The link between past informal payments and willingness of the Hungarian population to pay formal fees for health care services: results from a contingent valuation study. Eur J Health Econ. 2014;15(8):853-67. [PubMed ID: 23989982]. https://doi.org/10.1007/s10198-013-0531-y.
