1. Introduction
Oropharyngeal squamous cell carcinoma (OPSCC) is a relatively rare disease that is affected by alcohol and tobacco use (1). Along with conventional treatments for cancer, alcohol use control can increase survival rates in these patients. In the first months of absenteeism, alcohol-dependent patients often show sleep disorders, irritability, and depression, which indicate chronic activity of the stress-related pathways (2). In addition, losing self-confidence in interpersonal interactions leads to social deprivation and reduced willingness to participate in therapeutic programs.
Oxytocin hormone affects the transmission of physical signals, and due to its potential in craving modulation has been suggested as an alternative therapy for alcohol abuse disorders (3). From the neurobiological point of view, it has been suggested that the oxytocin social hormone can be effective on addictive behaviors such as alcohol use through the promotion of social interactions and the improvement of psychological indices (4). Oxytocin acts by inhibiting the effects of corticotropin-releasing hormone (CRH) on GABAergic interneuron in amygdala and hypothalamic nuclei (2). Studies have shown that heavy alcohol consumption is associated with lower levels of oxytocin in the brain, and this process is referred to as a mechanism for changes in social behavior, response to stress, and increasing alcohol abuse (5). Because oxytocin is a peptide, a delivery from intranasal pathway is a preferred method in clinical studies (6).
Studies have shown that intranasal oxytocin reduces the amount of neuronal cue reactivity in brain networks, which can be associated with reduced alcohol use (7). In preclinical and clinical studies, oxytocin has been successful in reducing the consumption of ethanol, cocaine, and methamphetamine (8).
Although studies have been conducted on the effectiveness of oxytocin on reducing alcohol use, this intervention has not been evaluated in patients with cancer. Therefore, the aim of this study was to investigate two hypotheses of the effectiveness of intranasal oxytocin on the reduction of alcohol consumption and its related problems and depression syndrome in a patient with oropharyngeal squamous cell carcinoma.
2. Case Presentation
The present study was a reverse A1B1A2B2C1 design with a multiple baseline and a six-month follow-up (clinical trial registration code: TCTR20180417001) that was carried out between January 2014 and May 2015. The patient is a 67-year-old married man having a child who has had heavy episodic alcohol consumption for about 20 years and was selected through a respondent-driven sampling method (9). Consumption of at least 24 standard drinks per week was considered as the criterion for heavy alcohol consumption. The patient about a year ago after the diagnosis of cell carcinoma by punch biopsy underwent radical resection of a squamous cell carcinoma of the oropharynx (in accordance with the Union for International Cancer Control’s [UICC] criteria: stage pT2, pN1), then, received adjuvant radiotherapy and cisplatin. Five months ago, computed tomography (CT) scan confirmed bone and lung metastases.
The patient was entered treatment process with an alcohol abuse complaint in the form of heavy episodic alcohol consumption and dysthymia. Based on the international classification of diseases, ninth revision (ICD-9) and the diagnostic and statistical manual of mental disorders (DSM), the patient was diagnosed as alcohol use disorder (ICD-code: 303). Also, after a structured clinical interview for DSM-5 disorders (SCID), diagnosis of dysthymia was confirmed.
During January 2014 and May 2015, we used a reverse A1B1A2B2C1 design with a multiple baseline and a six-month follow-up, that A was the baseline stage and B was the intervention phase, and C was considered as follow-up stage. Preliminary evaluation of the 28 days prior to the registration of the baseline included an electrocardiogram examination, blood, and urine tests by a team consisting of a psychiatrist, two clinical psychologists, and a nurse.
In A1 and A2 baselines (4 weeks, 8 evaluations), only evaluation was done and no intervention was made. In phase B1 (6 weeks, 12 evaluations) and B2 (6 weeks, 12 evaluations), an intranasal oxytocin was presented to the patient. In order to reduce the level of oxytocin plasma for evaluation as the second baseline, the interval between two phases of B1 and A2 was considered as 2 months. The entire study period was 14 months and 44 evaluations were carried out. Also, the sustainability of changes was evaluated in the form of a six-month follow-up (C1, 4 weeks, 4 evaluations).
Oxytocin intranasal spray (Syntocinon®; Novartis, Basel, Switzerland) included oxytocin plus glycerol, sorbitol, benzyl alcohol, and distilled water, that contained an amber 7 mL glass nasal spray with a metered pump. Placebo sprays had the same combination, but did not contain oxytocin. Each pump spray delivered 50 μL of Oxytocin (9 IU) or placebo. All sprays were safely kept at a cool temperature (4°C). The patient was provided with necessary instruction for proper use of nasal spray as well as recording the doses in a notebook and a timer was used as reminder. The bottles were collected at the end to assess the total amount and estimate the used dose. The medication was received by the patient on all the days (except for the first day that applied by the therapist) at two meals before breakfast (about 10 A.M.) and before afternoon snack (about 3 P.M.) each time with 18 IU doses (9 IUs puffs per each hole).
In this study, SCID-5, Beck depression inventory (BDI) and alcohol use disorders identification test (AUDIT) were used. All interviews were digitally recorded and copied from the words and coded. All the data of this study were collected after agreement with the patient, and informed consent was received before the intervention and publication, and all stages of the study were based on the latest version of the Declaration of Helsinki (DoH). The data were analyzed, using the generalized estimation equation (GEE) (10), a generalized linear mixed models (GLMM, random effects models) with repeated measures, and repeated measures correlation (rmcorr) (11).
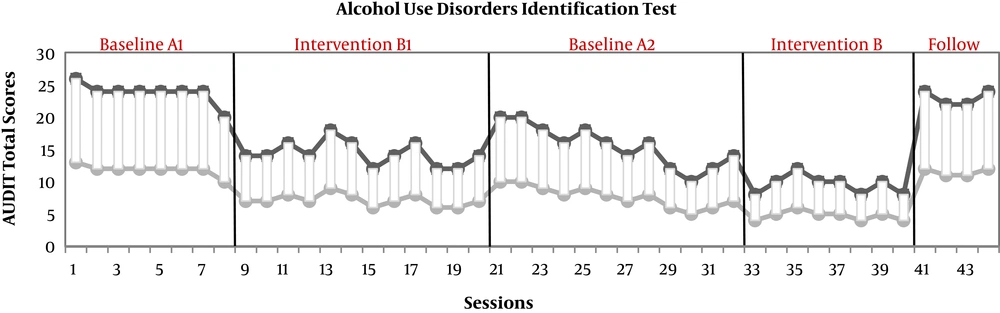
The scores of the subject in the variable of total score of AUDIT during 14 months and in the form of 44 evaluations are presented in Figure 1.
As it could be seen, the results of the GEE test show that there were significant decreases in the two stages of intervention (B1 and B2) (P < 0.02). This improvement was not maintained in the follow-up stage (P < 0.05).
GLMM showed that the decrease in alcohol consumption and its related problems in interaction with the depression index was significant (P < 0.03).
Correlation test with repeated measures showed that there is a significant relationship between two indices of consumption rate and depression (P < 0.008).
3. Discussion
This study was conducted with the aim of evaluating the effectiveness of oxytocin on reducing alcohol consumption and improving mood. Primary outcome showed that oxytocin reduced alcohol consumption and its related problems, as well as depression syndrome. The secondary outcome revealed a reverse relationship between alcohol consumption and its related problems with depression. In this regard and in line with the primary outcome of the present study, the results of the study conducted by Faehrmann et al. (2) show that oxytocin by reducing the anxiety and depression, can reduce the mechanism of craving in alcohol dependent people and help the patient in the abstinent phase.
Contrary to our results, the results of a study carried out by Betka et al. (3) showed that despite the effectiveness of oxytocin on interoceptive accuracy, this drug is not effective in reducing alcohol consumption. However, studies show that defect in interoceptive function can explain depression syndrome (12).
Another part of findings of this study showed that oxytocin is effective in reducing depression syndromes. In accordance with our findings, the results of study performed by Love et al. (4) show that oxytocin, by increasing social participation and improving mental health, improves psychological indices such as depression in alcohol users. The findings of a study conducted by Faehrmann et al. (2) suggest the moderator role of oxytocin on stress-related pathways in alcohol dependent individuals, which can be used in treatment.
The secondary outcome showed that there is a significant direct relationship between dysthymic syndrome and alcohol abuse. In line with these results, Carton et al. (13) showed that subjects with major depressive disorder (MDD)-alcohol use disorder (AUD) in terms of symptomatology and comorbidity had a more consistent profile than the subject with MDD only. Ethanol consumption decreases the activity of the hypothalamic pituitary adrenal (HPA) axis, which can affect respond to stress with the mediator of serotonergic system and affect mood parameters (14). In line with the results of this study, the results of a study carried out by Pirnia et al. (15) also showed that there is a significant relationship between changes in the function of HPA axis and depression syndrome in the drug abusers.
According to the single case nature of this study, the effects of intranasal oxytocin on alcohol consumption and depression need to be repeated in a larger study. Another limitation in this study was the use of self-report scales of depression and alcohol consumption that could have been associated with bias. It is suggested that in future studies, biological evaluations should be used to investigate the variables. The implementation of a randomized controlled trials (RCTs) on the effectiveness of oxytocin in individuals diagnosed with alcohol use disorder can be a good route for future studies.