Abstract
Background:
Different automated systems have been developed to improve the maintenance of target range of arterial oxygen saturation (SPO2) in premature infants with respiratory distress.Objectives:
This study aimed to develop a remote closed-loop automatic oxygen control (RCLAC) as an efficient monitoring device. Then the means of the fraction of inspired oxygen (FIO2) and SPO2 by routine manual control (RMC) and RCLAC were compared.Methods:
A developmental-descriptive study was carried out in an Iranian hospital (Tehran, Iran; 2015 - 2017). Twenty-two preterm infants with gestational age 24 - 28 weeks entered the study. A database was prepared based on pulse oximeter parameters. A Wi-Fi module was implemented to receive data from a pulse oximeter and send inputs to the user’s mobile. Vibrate alarm was implemented for high or low FIO2. After receiving notifications associated with an increase or decrease of FIO2 levels and user’s confirmation; the alterations were applied on the ventilator.Results:
The mean FIO2 in the RMC system was significantly higher than the RCLAC system (98.1 ± 2.67 vs 79.5 ± 16.03; P = 0.0001). According to the results, when the SPO2 reached close to target SPO2 range and consequently FIO2 changed (decreased or increased based on target SPO2), heart rate showed a regular beating with a decrease in the numbers.Conclusions:
Remote closed-loop automatic oxygen control system as a simple device could prevent preterm neonates from sustained hypo-hyperoxemic and arrhythmia episodes. Moreover, by using RCLAC, there was no need for continuous monitoring that may reduce the workload of NICU medical staff. Collecting reliable data and recording information in digital forms were also other benefits. Further studies with larger sample size are strongly suggested.Keywords
Remote Closed-Loop Automatic Oxygen Control Infant Premature Arterial Oxygen Saturation Fraction of Inspired Oxygen
1. Background
Oxygen therapy for premature infants with respiratory distress is a critical subject. Hypoxemia can lead to permanent nervous system damage or organ failure resulting in high morbidity and mortality rates. On the other hand, hyperoxemia in some cases may lead to heart, lungs, brain, retina and hearing system damages. Maintenance of adequate blood oxygen concentration to minimize the risks of both hypoxemia and hyperoxemia are the main goal related to mechanical ventilation in hospitalized premature infants (1-4).
Maintenance of oxygen saturation target is monitored by a pulse oximetry which detects arterial oxygen saturation (SPO2) and fraction of inspired oxygen (FIO2) indices. Adjustment of respiratory support within the clinically intended range of SPO2 is affected by some factors like routine manual control (RMC) by clinical staff and their responses to SPO2 frequent fluctuations. It is clear that a higher nurse-to-patient ratio can improve the achievement of oxygenation targets by preventing neonates from spending a long time above the clinically intended range of SPO2 (1, 5).
Different automated systems have been developed to improve maintenance of the target range of SPO2 and a decrease of limitations related to routine manual control. Kwok et al. (6) extracted basic rules to improve control respiratory devices by using an adaptive neuro-fuzzy inference system (ANFIS) with multilayer perceptron (MLP) and the FAVeM algorithms. They could reduce the workload of physician resulting in better decision making (6). Another control system was developed to automatically adjust the frequency of breaths and tidal volume of lungs. Proportional-integral-derivative (PID) control algorithm, feedback data from devices, and some physiological data were used to reduce fluctuations of arterial oxygen (7). An AUTOPILOT-BT control ventilator system was also designed based on a set of fuzzy controllers combined with explicit physiological modeling and a neural network. This model could enhance mechanical ventilation therapy and decrease the workload of intensivists (8). Another investigation demonstrated that a closed-loop automatic control (CLAC) could improve oxygen administration to preterm infants while reduced workload related to RMC (2).
Recently, several studies focused on mobile health (m-Health) as help in collecting more and easier information, constant monitoring, and reducing unnecessary medical interventions. Over 3.1 billion mobiles around the world have the ability to connect wirelessly. This intended software algorithm with multi-services providers may influence sooner clinical diagnosis and better medical management with lower costs and less time consuming (9-11).
Keeping arterial oxygen saturation (SPO2) in a standard range for premature infants is of importance. On the other hand, continuous monitoring constrains extra workload for NICUs medical staff especially in crowded wards with undeveloped medical infrastructures. It is supposed that a closed-loop automatic oxygen control system conducting a remote monitoring device may facilitate managing target SPO2 with features such as acoustic, exhibition and vibrating alert. Moreover, the collection of reliable data in digital form may reduce the staff’s workload.
2. Objectives
This study aimed to develop a remote closed-loop automatic oxygen control (RCLAC) as a quick and efficient monitoring device. Then the mean of FIO2 and SPO2 by RMC and RCLAC were compared.
3. Methods
3.1. Study Design
This developmental-descriptive study was carried out in the NICU of Yas Women’s Hospital affiliated to Tehran University of Medical Sciences in collaboration with School of Allied Medical Science and Saadat Co. (Tehran, Iran) from October 2015 to July 2017. Twenty-two preterm infants with gestational age 24 - 28 weeks entered the study. Congenital diaphragmatic hernia, cyanotic heart disease, severe apnea, perfusion index (PI) < 0.4 and any medical condition with deviation from the usual SPO2 target range was considered as exclusion criterion.
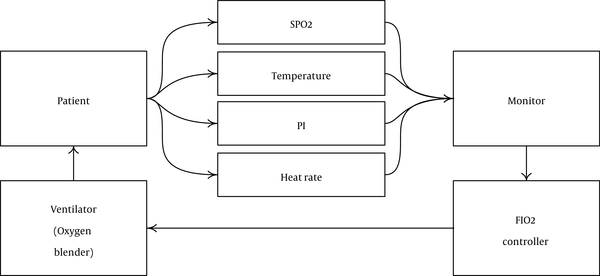
Firstly, a checklist was prepared according to the literature review to define some important demographic and physiologic parameters related maintaining of PaO2 in a target range (gestational age, sex, temperature, heart rate, results of arterial blood gas test, FIO2, SPO2, PI, pH, pCO2, pO2, Hct, …). In the next step, eight expert neonatologists and pediatric intensivists were asked to prioritize these parameters by score 1 to 10. Of 19 variables, 4 criteria had the greatest scores. The efficiency index (from 1 to 5) was calculated for each important criterion (Table 1). Hence, alterations of these important variables had to be constantly considered and all decisions made based on them. After determining the significant variables associated with arterial oxygen status, physicians were asked to design a medical algorithm (Figure 1).
Scoring of Important Variables by Physicians
| Variables | Physicians Scores (N = 8) | Mean Scores | Efficiency Index | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| FIO2 | 10 | 9 | 9 | 9 | 10 | 9 | 9 | 9 | 9.2 | 4.6 |
| SPO2 | 9 | 9 | 8 | 10 | 10 | 8 | 9 | 10 | 9.1 | 4.8 |
| Temperature | 8 | 6 | 9 | 7 | 9 | 9 | 7 | 8 | 7.8 | 2.6 |
| Perfusion index | 7 | 8 | 6 | 9 | 9 | 6 | 7 | 8 | 7.5 | 4.7 |
| Heart rate | 4 | 3 | 2 | 3 | 3 | 4 | 5 | 7 | 3.8 | 3.6 |
Flow chart of clinical approach to treatment. A, Heart rate drops in deep sleep. So, heart rate 80 bpm was considered as the default; B and C, in cases of body temperature (arms or legs) < 36°C or PI < 2, a mistake might have been happened in pulse oximetry measures (12). So, the accuracy of pulse oximetry signals should be considered in doubt; C, in PI values lower than 2, we could not count on SPO2 signals from pulse oximetry. In practice, this value for infants was 0.7, so PI < 0.4 was not considered. However, system user could define minimum heart rate, minimum temperature and minimum PI depending on patient’s condition; D, preventing neonate from sudden fluctuations in oxygen status, 10 units were considered for checking FIO2 alterations and SPO2 feedbacks. Increase of FIO2 after a block in airway or FIO2 decreasing without any changes in SPO2 value could indicate a trap in the system. In such situations, an alarm should be sent to the user. There were also other options; first, neonatologist could change FIO2 based on patient’s condition. Second, system warned following sudden rise or drop (± 10%) of SPO2 values in less than 40 seconds; E, separating probe from patient’s body, monitor sent values regarding SPO2 and heart rate while system displayed an alarm to warn neonatologist; F, G, considering feedback of FIO2 from pulse oximeter, different opinions from 20 seconds to 5 minutes have been reported (2, 7, 13). So, the minimum time was considered to add one unit per 20 seconds. Moreover, a time near median (between 2 to 5 minutes) was considered to reduce one unit per 3 minutes. Regarding part F, there were 3 reasons to reduce FIO2. First, neonate should be able to breathe normally (21% oxygen). Second, hyperoxia should be prevented because of its side effects. Third, according to oxyhemoglobin dissociation curve, there is a nonlinear association between SPO2 and PaO2 in PaO2 levels more than 98%, the accurate SPO2 values could not be calculated in these ranges; H, five hours after stabilizing patient's condition, final decision was made by neonatologist to change approach to the treatment.

3.2. Development and Implementation of Devices
After algorithm design, database software was prepared based on pulse oximeter parameters. A Wi-Fi module (designed by Saadat Co.) was implemented to receive data from a pulse oximeter and send inputs to user’s mobile. Moreover, a mobile application was also developed with a particular service for reading input data from the module. Different mobile alerting approaches including text message, sound alarm and vibrating alarm detected different variables; vibrate alarm was implemented for high or low FIO2 and a sound-vibrate alarm was designed for demonstrating heart rate, temperature, PI, sudden fluctuations or device disconnection from the patient. It should be noted that all of these alarm types were optional for staff to set for each patient’s events based on the importance of the events.
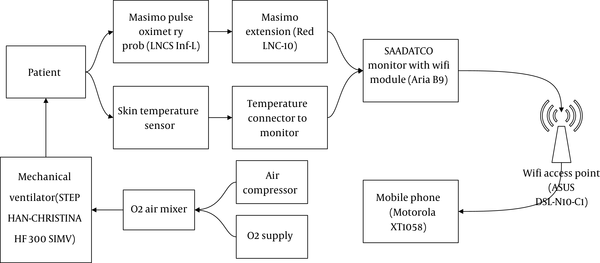
The mobile phone was connected through Wi-Fi network. The user (neonatologist or NICU nurse) could receive information related to the patient’s situation to perform or order the necessary care. Using this new algorithm could provide a controlling system to change FIO2 under the direct supervision of a medical specialist. After receiving notifications, associated increase or decrease of FIO2 levels and user’s confirmation, the alterations were applied on the ventilator. If this alarm was not confirmed by a user, the alterations were not applied as well (Figures 2 and 3).
General algorithm
Equipment setup
3.3. Sample Size
First, a pilot experimental study was carried out on 10 participants to compare FIO2 between RMC and RCLAC groups. A significant difference was observed between groups regarding FIO2 (in RMC group = 97.4 ± 3.2 vs in RCLAC group = 74.1 ± 19; P = 0.0001). Then, based on using compare means formula; with the proposed sample size of 18, the study had a power of 90% and an alpha error of 0.05. Finally, according to an investigation by Hallenberger et al. (2), 22 subjects entered the study for better data analysis with appropriate power.
3.4. Protocol
In the present study, two approaches (RMC and RCLAC) in twenty-four-hour periods were compared. Normal FIO2 was considered as the least amount of FIO2 that SPO2 was maintained in a target range. This range regarding SPO2 had been determined by neonatologist based on the patient’s situation. Nurses were asked to pay special attention to signs and warnings. With software alerts due to drop or increase of SPO2 from the target range, the nurse had to increase or decrease the amount of FIO2. After nurse confirmation, the alerts were applied on the ventilator. If the alarm was not confirmed by a nurse, alerts would not be applied on the ventilator. Similarly, the software did not change the amount of FIO2. The nurse-patient ratio at NICU was 1:2 to 1:3.
3.5. Primary/Secondary Outcomes
The FIO2 algorithm was tested and compared among premature neonates with RMC and RCLAC to keep SPO2 in the target range as the primary outcomes. Heart rate alterations following the decrease or increase of SPO2 and FIO2 were also assessed as our secondary outcomes.
3.6. Ethical Considerations
The present study was taken from a student’s thesis with ID; IR290-441. Ethics approval was obtained from the institutional review board of Tehran University of Medical Sciences according to Helsinki Declaration (no.: IR.TUMS.SPH.REC.1395.1537). All participants’ parents gave written consent before enrollment. All gathered data were considered confidential and no extra cost was imposed on our participants.
3.7. Data Acquisition and Analysis
RCLAC software had the ability to record and save data correlated demographic characteristics, respiratory or heart co-morbidities, FIO2, SPO2, PI, temperature, and ABG results on the mobile phone. Moreover, this database had the potential to be connected to the central database. Local database from the mobile phone was transferred to a PC-computer. Then information was extracted from the database with SQL query. All data were classified by patients’ file numbers. Recorded data were analyzed to compare the FIO2 between RMC and RCLAC groups. All statistical analyses were conducted using SPSS 19. Data were presented as mean ± standard deviation for continuous variables and No. (%) for categorical variables. Kolmogorov-Smirnov test and t-test were used for analyzing the relationships between variables.
4. Results
After storing information in the database, reliable and classified data had been available. Table 2 presents a summary of the patient’s demographic characteristics. Twenty-two preterm infants with gestational age 24 - 28 weeks entered the study. Of all, 4 neonates with severe apnea or PI < 0.4 were excluded. Eighteen neonates (10 males and 8 females) with the mean birth weight 865 ± 241 g were included. The Kolmogorov-Smirnov test showed normal distributions in all variables including birth weight (P = 0.9), gestational age (P = 0.9), age (P = 0.9), RMC FIO2 (P = 0.08), RCLAC FiO2 (P = 0.123) and PI (P = 0.4).
| Variables | Values |
|---|---|
| Gender | |
| Male | 10 (55.6) |
| Female | 8 (44.4) |
| Mean birth weight, g | 865±125 |
| Mean gestational age, wk | 27.3±2.4 |
| FIO at study entry | 98 (80 - 100) |
| FIO2 in RMC group | 98.11 ± 2.67 |
| FIO2 in RCLAC group | 79.50 ± 16.03 |
| Ventilation mode | |
| Mechanical ventilation | 12 (66.66) |
| CPAPb | 6 (33.33) |
| Surfactant treatment | |
| No | 7 (38.8) |
| Yes | 11 (61.2) |
| History of multiple gestations | |
| No | 14 (77.77) |
| Yes | 4 (22.22) |
| PIc | 0.78 (0.3 - 1.9) |
| Age, d | 27 (1 - 51) |
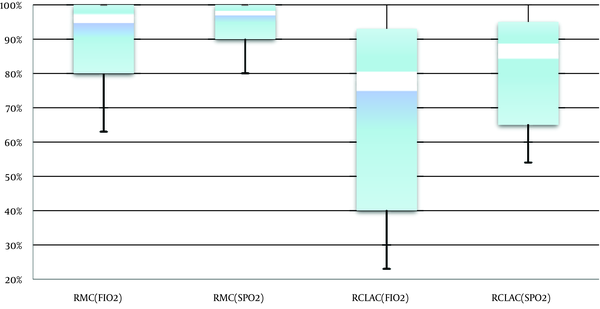
The t-test analysis showed that the mean FIO2 in RMC system was significantly higher than RCLAC system (98.1 ± 2.67 vs 79.5 ± 16.03; P = 0.0001).
Comparing FIO2 and target SPO2 in RCLAC and RMC systems, a box and whisker plot demonstrates (Figure 4) a fall in FIO2 level based on target SPO2 by applying RCLAC. The mean of FIO2 value decreased from 97% to 79%. Moreover, regarding SPO2 setting by physician’s recommendations, the mean of SPO2 level dropped from about 98% to approximately 88%.
Box and whisker plot comparing FIO2 and target SPO2 in the RCLAC and RMC systems
According to the results, when the SPO2 reached close to target SPO2 range and consequently FIO2 changed (decreased or increased based on target SPO2), heart rate showed a regular beating with decrease in the numbers. As detailed data are shown in Figure 5, after setting the target SPO2 on 93%, FIO2 dropped from 100% to 82% at 1:52 PM and heart rate decreased undergoing to 90 bpm.
Example of RCLAC control of process-target SPO2 (93%)
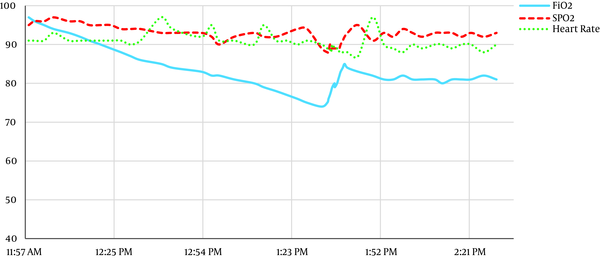
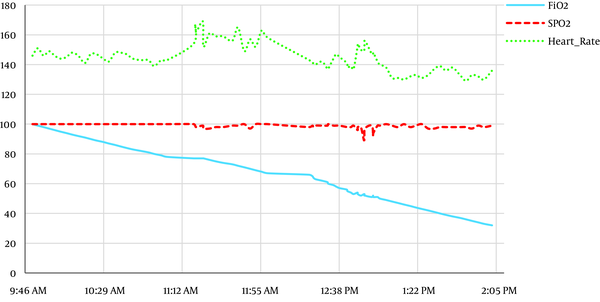
Figure 6 indicates when the target SPO2 was set on 90% (after 1:49 PM), the FIO2 decreased to below 60% and the SPO2 value reached close to 90%. After reaching to desirable SPO2 level, the chart showed a decrease in heartrate fluctuation with regular rhythms. At that time the heart rate was close to 140 bpm.
Example of RCLAC treatment process-target SPO2 (90%)
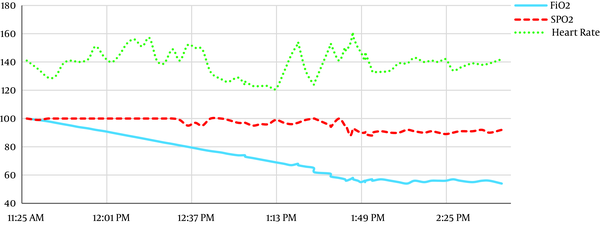
Figure 7 shows that the lungs were able to supply oxygen and the patient did not need any supplementary oxygen. Decreasing FIO2 from 100 to below 80% caused no SPO2 alterations from the target range. Slight fluctuations in heart rate and SPO2 were observed with reducing FIO2 to about 50%. This trend continued until the natural environment (21% oxygen) was achieved. However, after 1:04 PM, the heart rate was regular and its rate reduced to below 140 bpm.
Example of RCLAC treatment process-target SPO2 (95%)
5. Discussion
In the present study, we designed a remote closed-loop automatic oxygen control system as a simple device to keep arterial oxygen saturation (SPO2) in a standard range for premature infants without the danger of hypo/hyperoxemia. Moreover, by using RCLAC besides managing target SPO2, there was no need for continuous monitoring that might reduce the workload of Neonatal Intensive Care units (NICU) medical staff. Collecting reliable data and recording information in digital forms were additional benefits. The strength of our study was the consideration of neonate’s heart rate during FIO2-SPO2 controlling.
According to the results, by implementing the RCLAC system, the mean FIO2 (considering target SPO2) was kept in a lower range compared with the RMC system. Using such an adaptive model could be responsible for setting the minimum FIO2 for the target SPO2 keeping preterm neonates from high O2 exposure, sustained hyperoxemic episodes or fluctuations in SPO2 levels resulting in enhanced outcomes. Compatible to our finding, Hallenberger et al. (2) designed a closed-loop automatic oxygen control system (CLAC) using a laptop computer executing the FIO2 software connected to pulse oximeter and ventilator. They demonstrated that by implementation of the system, oxygen administration to preterm infants was improved and optimized. The percentage of time spent within the SPO2 target range (target %) in the CLAC group was significantly higher in comparison with the RMC group. They concluded that by using such systems, unnecessarily high or low O2 exposure could be prevented (2). Claure et al. (3) have also pointed to some studies showing that for maintaining the neonates’ oxygenation targets, automated FIO2 control system would be more efficient and practicable compared to manual FIO2 control system. Based on their results, the factor defined as % time within oxygenation target by automated control system was higher than this factor by routine manual modes (3). Another investigation by Morozoff et al. (14) have indicated that using automated closed loop control system instead of manual system could enhance oxygen therapy by increasing normoxemia periods in infants.
Another point associated with RCLAC system in comparison with RMC system was maximum and minimum feedback times for inhaling oxygen. The results of the present study have shown that the maximum time to reduce FIO2 was 3 minutes and the mean of 20 seconds was needed to increase FIO2 levels. Morozoff et al. (14) have illustrated that by using adaptive control modes, within two or five minute periods, the controller could adjust the FiO2-SPO2 relationship resulting in normoxemia (14). Tehrani et al. (13) demonstrated that the time less than 20 seconds was required for returning the arterial oxygen saturation to the normal safe range by the implementation of their proposed closed-loop automatic control system.
Based on the results, after adjusting desirable FIO2-SPO2 levels by our proposed controller system, a decrease and regularity in the heart rate chart were notable. Decrease in heart rate fluctuation with regular rhythms not only protect neonate from arrhythmia and its related adverse outcome but also can decrease the NICU staff’s stress. Moreover, this benefit could prevent the patient from more medical interventions that may affect respiratory function. Upon our knowledge, our study was the only investigation that evaluated participants’ heart rates during maintenance of FiO2-SPO2 in the normal ranges.
Former studies have confirmed that manually administering oxygen therapy is difficult and time-consuming (1-3, 13, 14). Results of the present study demonstrated that by using the RCLAC system, the workload of the staff related to full FIO2 control was reduced. Furthermore, with the systematization of daily reports related to RCLAC system, clinical staff did not waste lots of time on completing patient’s medical records. RCLAC software had the ability to record and save all demographic characteristics data. This database had the potential to be connected to the central database that facilitated the availability of data for medical staff. By adjusting FIO2, the patient and NICU’s stresses could be alleviated that may influence the prognosis of the disease and personnel efficiency. Finally, the RCLAC system as an easily applicable and not-complex system was designed to warn NICU nurses based on patients’ condition. Staff by alarms related to the patients’ status was being promptly informed.
5.1. Strengths and Limitation of the Study
The previous studies have shown some risks related to the development of mechanized control systems in oxygen therapy for respiratory complicated patients (1, 3, 5). Therefore, a system was designed and implemented that could easily and promptly warn nurses based on patients’ condition. Besides that, this system would be helpful for staff; they were informed by alarms related to the patients’ status instead of full control monitoring.
Our study had some limitations. Our sample size was small. Such studies with larger sample size are recommended. We did not design the sensors controlling PEEP and PIP under Wi-Fi network. Therefore, the data associated sensors detecting increase or decrease of FIO2 were not considered. Use of PEEP and PIP control sensors was strongly suggested in subsequent studies.
5.2. Conclusions
Remote closed-loop automatic oxygen control system as a simple device could keep preterm neonates from sustained hypo-hyperoxemic and arrhythmia episodes. Moreover, by using RCLAC, there was no need for continuous monitoring that may reduce the workload of NICUs medical staff. Collecting reliable data and recording information in digital forms were also other benefits.
References
-
1.
Claure N, Bancalari E. Automated closed loop control of inspired oxygen concentration. Respir Care. 2013;58(1):151-61. [PubMed ID: 23271825]. https://doi.org/10.4187/respcare.01955.
-
2.
Hallenberger A, Poets CF, Horn W, Seyfang A, Urschitz MS, Clac Study Group. Closed-loop automatic oxygen control (CLAC) in preterm infants: A randomized controlled trial. Pediatrics. 2014;133(2):e379-85. [PubMed ID: 24470641]. https://doi.org/10.1542/peds.2013-1834.
-
3.
Claure N, Bancalari E. Oxygen saturation targeting by automatic control of inspired oxygen in premature infants. NeoReviews. 2015;16(7):e406-12. https://doi.org/10.1542/neo.16-7-e406.
-
4.
Bancalari E, Claure N. Respiratory instability and hypoxemia episodes in preterm infants. Am J Perinatol. 2018;35(6):534-6. [PubMed ID: 29694990]. https://doi.org/10.1055/s-0038-1637760.
-
5.
Claure N, Bancalari E. Role of automation in neonatal respiratory support. J Perinat Med. 2013;41(1):115-8. [PubMed ID: 23093255]. https://doi.org/10.1515/jpm-2012-0031.
-
6.
Kwok HF, Linkens DA, Mahfouf M, Mills GH. Rule-base derivation for intensive care ventilator control using ANFIS. Artif Intell Med. 2003;29(3):185-201. [PubMed ID: 14656486]. https://doi.org/10.1016/s0933-3657(02)00074-x.
-
7.
Tehrani F, Rogers M, Lo T, Malinowski T, Afuwape S, Lum M, et al. A dual closed-loop control system for mechanical ventilation. J Clin Monit Comput. 2004;18(2):111-29. [PubMed ID: 15362273]. https://doi.org/10.1023/b:jocm.0000032744.99885.38.
-
8.
Zhu H, Moller K, editors. Ventilator control based on a fuzzy-neural network approach. Bioinformatics and Biomedical Engineering. The 2nd International Conference. IEEE; 2008.
-
9.
Cortez NG, Cohen IG, Kesselheim AS. FDA regulation of mobile health technologies. N Engl J Med. 2014;371(4):372-9. [PubMed ID: 25054722]. https://doi.org/10.1056/NEJMhle1403384.
-
10.
Steinhubl SR, Muse ED, Topol EJ. Can mobile health technologies transform health care? JAMA. 2013;310(22):2395-6. [PubMed ID: 24158428]. https://doi.org/10.1001/jama.2013.281078.
-
11.
Shortliffe EH, Cimino JJ. Biomedical informatics. Germany: Springer Science & Business Media; 2013. https://doi.org/10.1007/978-1-4471-4474-8.
-
12.
WHO. Pulse oximetry training manual. Geneva, Switzerland: WHO Press; 2011.
-
13.
Tehrani F, Rogers M, Lo T, Malinowski T, Afuwape S, Lum M, et al. Closed-loop control if the inspired fraction of oxygen in mechanical ventilation. J Clin Monit Comput. 2002;17(6):367-76. [PubMed ID: 12885181]. https://doi.org/10.1023/a:1024261021473.
-
14.
Morozoff EP, Smyth JA. Evaluation of three automatic oxygen therapy control algorithms on ventilated low birth weight neonates. Conf Proc IEEE Eng Med Biol Soc. 2009;2009:3079-82. [PubMed ID: 19963561]. https://doi.org/10.1109/IEMBS.2009.5332532.