1. Background
TOF is the most common cyanotic congenital heart disease, occurring in 7% to 10% of all congenital cardiac malformations.
It can be more complicated if it coincides with the coronary tree anomalies, like a single coronary ostium, left anterior descending coronary artery (LAD) arising from the right coronary artery (RCA), origin of a circumflex artery from the RCA, origin of the RCA from the LAD and a large conus artery or large anterior ventricular branch crossing the RVOT, double LAD (1).
The definite treatment of these patients is open heart surgery with or without trans-annular patch dilation of the right ventricular outflow tract, which might be complicated by crossing of a coronary artery across the RVOT. Diagnosis of abnormal coronary course can lead to total surgical correction by homograft technique. Therefore, determination of coronary artery anatomy is a crucial issue before any surgical correction in these patients.
In a normal coronary anatomy, which is the most common type in TOF, no significant coronary branches cross the RVOT. The common coronary artery variations in TOF are LAD arising from the RCA or a single coronary artery coming from either the right or left sinus. In these two variations, the LAD or the other major branches might pass across the RVOT and complicate the surgical correction of TOF (1-4).
The best method for detection of coronary artery anatomies, anomalies and particularly courses in preoperational evaluation of TOF is still a challenging issue and has evolved during the last years, and coronary angiography, CT angiography or echocardiography are performed by congenital cardiology centers as mandatory workups to assess the coronary artery anomalies and courses before total surgical correction (2, 5-7). Most surgeons and cardiologists prefer angiography and catheterization for intracardiac and extracardiac evaluations and coronary anatomy assessment, pressure determination, and possible need of intervention (6).
On the other hand, cardiac angiography and catheterization produce hazardous X-ray radiation, and decreasing the radiation dose in angiography requires knowledge of the best and least views for detection of coronary anomaly to avoid unnecessary cineangiography and fluoroscopies (8).
2. Objectives
The present study was conducted on a large number of patients to explore the most accurate angiography view for diagnosis of the coronary artery anatomy and courses to prevent unnecessary radiation.
3. Methods
This retrospective study investigated the patients older than 3 months of age with TOF who underwent cardiac catheterization and then total surgical correction at our tertiary heart center affiliated to Shiraz University of Medical Sciences, from March 2005 to July 2018. The patients with complex TOF physiology together with other disorders, including pulmonary atresia, complete atrioventricular canal defect, double-outlet right ventricle, absent pulmonary valve syndrome, or aortopulmonary window were excluded from the study.
Baseline characteristics including age, gender, weight at the time of surgery and past medical history of cardiac interventions were recorded. All our patients had preoperational angiography evaluation. The findings of angiography including coronary artery anomalies, and the angiographic views of all patients were extracted from our angiography database. According to our policy, non-selective coronary angiography was done in the aortic root to diagnose coronary abnormalities.
The patients were stratified into two groups: group one from 2005 to 2015 whose aortic root angiographies were done in LAO/CRA view (35° - 40°/20° - 25°), and group two, from 2015 onward, who underwent aortic root angiography in both LAO/CRA and LAO/CAU (10° - 15°/40° - 45°) views (9, 10). Thus, all the patients had LAO/CRA view, but LAO/CAU view was only performed in group 2 in addition to LAO/CRA view.
Both LAO/CRA and LAO/CAU were separately reviewed and reported, and then we analyzed the rate of abnormality detection in each view. Operation notes of the patients were reviewed for any coronary anatomy variation at the time of surgery, and the result recorded. We tried to separate the process of data gathering from angiographic reports and operational notes to avoid possible biased. The data of surgical reports were considered as a gold standard to evaluate the accuracy of the angiography reports.
Experience of a cardiologist might interfere with the interpretation of angiography records, and we tried to decrease this effect to accurately determine eligibility of these two views for detection of coronary artery anomalies and courses. Thus, the cineangiograms of the 8 patients who had abnormal coronary artery at the surgery time were reviewed blindly by an expert pediatric cardiologist with more than 10 years of congenital cardiac catheterization experience.
3.1. Statistical Analysis
All the statistical analyses were performed using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA). Values are expressed as mean ± standard deviation for the quantitative variables and percentages for the categorical variables. Data were compared using the paired t-test for the continuous variables and the chi-square test (or Fisher’s exact test if required) for the categorical variables. To report the sensitivity and specificity, we used MedCalc, version 14.8.1. This study was conducted with the power of 80% and P values of 0.05 or less were considered statistically significant.
4. Results
Four hundred and fifty one patients with TOF who underwent surgery for total correction were included in this study. The patients’ age was from 3 months to 432 months with a median of 28 months. Among them, 254 patients were male and 197 female (M/F ratio: 1.2). All patients had LAO/CRA view and 199 patients had both LAO/CAU and LAO/CRA views (group 2). The percentage of the coronary abnormality in the operation notes was 8% (36 cases) (Table 1 and 2).
| Angiography Finding | Total | Surgery Finding (Gold Standard) | |
|---|---|---|---|
| Normal Coronary Artery | Coronary Artery Anomaly | ||
| Normal coronary arteries | 422 (93.6) | 413 (91.6) | 9 (2) |
| Coronary artery anomaly | 29 (6.4) | 2 (0.4) | 27 (6) |
| Total | 451 (100) | 415 (92) | 36 (8) |
aValues are expressed as No. (%).
bPearson chi-square = 305.73 and P = 0.001.
| Angiography Finding | Total | Surgery Finding (Gold Standard) | |
|---|---|---|---|
| Normal Coronary Artery | Coronary Artery Anomaly | ||
| Normal coronary arteries | 189 (94) | 189 (100) | 0 (0) |
| Coronary artery anomaly | 10 (6) | 0 (0) | 10 (5) |
| Total | 199 (10) | 189 (95) | 10 (5) |
aValues are expressed as No. (%).
bPearson chi-square = 312.4 and P = 0.003.
Nine patients had coronary artery anomalies in the operation note that were not reported in angiography, and were considered false negative angiographies, while all were amongst the group one view.
The angiographic data in 2 patients indicated coronary abnormalities that were not confirmed during the operation, considering false positive of the angiography. Both of these cases were amongst the group one patients with LAO view.
Data for sensitivity and specificity of these two groups for diagnosis of abnormal course of coronary arteries are presented in Table 3. It clearly shows rising of the sensitivity and specificity to 100% when we included the caudal view.
| Values, % | |
|---|---|
| In All cases (group 1 included 451 patients) | |
| Sensitivity | 75.00 |
| Specificity | 99.52 |
| Positive predictive value | 93.10 |
| Negative predictive value | 97.87 |
| Area under the curve | 0.87 |
| CAU view (in 199 patients) | |
| Sensitivity | 100 |
| Specificity | 100 |
| Positive predictive value | 100 |
| Negative predictive value | 100 |
| Area under the curve | 0.98 |
According to the surgery reports, the LAD from RCA was the most common abnormality (4.4%), and both large conus branch and LAD passing across the RVOT were seen in 2 patients. Table 4 shows different coronary artery abnormalities and their sex distribution based on surgery reports. There was no significant difference between male and female patients regarding the anomalies (Table 4 and Figures 1-3).
| Normal | LAD From RCA | P Value | RCA From LAD Passing the RVOT | P Value | Branch of LAD Passing the RVOT | P Value | Conus Branch Passing the RVOT | P Value | Total | |
|---|---|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||||
| Male | 232 (56.2) | 13 (65) | 0.6 | 2 (66.7) | 0.65 | 4 (50) | 1 | 3 (42.9) | 0.7 | 254 (56.3) |
| Female | 181 (43.8) | 7 (35) | 1 (33.3) | 4 (50) | 4 (57.1) | 197 (43.7) | ||||
| Total | 413 (91.6) | 20 (4.4) | 3 (0.7) | 8 (1.8) | 7 (1.5) | 451 (100) |
Abbreviations: LAD, left anterior descending; LCA, left coronary artery; RCA, right coronary artery; RVOT, right ventricle outflow tract.
aValues are expressed as No. (%).
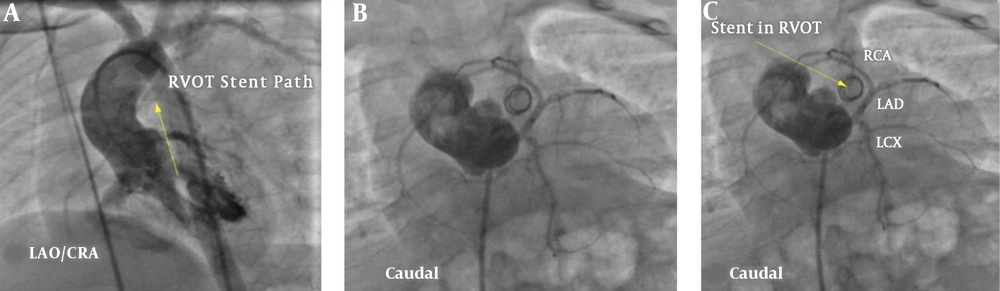
A 12-month old infant with TOF and previous RVOT stenting. A, In LAO/CRA view interpreting of the RCA course is very difficult in this single origin coronary artery case; B and C, caudal view clearly showed RCA from LAD that passed anterior to the RVOT stent. The surgeons need to approach from anterior of the RVOT stent which is in the superior part of the snapshot image to release the RVOT stenosis. LAD, left anterior descending; RCA, right coronary artery; RVOT, right ventricle outflow tract; LCA, left coronary artery.
As mentioned in the method section, the cineangiogram of the 8 patients with abnormal coronary artery in operation were reviewed blindly by an experienced pediatric cardiologist to compare the sensitivity of the two angiographic views. As Table 5 shows, the accuracy of caudal view was significantly higher than that of LAO view and all cases were detected in caudal views. The LAO view might misdiagnose many cases.
| Value | |
|---|---|
| Diagnosis in LAO/CRA view | 2 |
| Diagnosis in CAU view | 8 |
| Diagnose in both LAO/CRA and LAO/CAU views | 2 |
Abbreviations: LAO/CAU, left anterior oblique/caudal; LAO/CRA, left anterior oblique/cranial.
5. Discussion
Detection of coronary artery anomalies before surgery is necessary to determine the surgical technique and to provide homografts or other tube grafts for total correction of these patients (3, 8, 11-13). At the present time, either preoperational coronary angiography or coronary CT angiography can be used, although the selection is mainly influenced by the availability of suitable CT angiography device. Most of the recent articles are in favor of less invasive methods, CT angiography, especially when fast dual CT angiography is available (2, 3, 9, 14). On the other hand, when CT angiography is not available, the accuracy of cardiac angiography and the best view of root aortogram to detect coronary anomaly is an open issue. We tried to investigate these subjects in our study by retrospective comparison of angiographic and surgical reports in large number of TOF patients.
According to the results of present study, 36 of 451 patients (8%) had coronary artery anomalies that was in concordance with results of other studies, although previous studies have wide range of reports from 2% to more than 30 percent (1, 4, 15). Fellow and colleagues in a retrospective study reported 8% coronary arteries anomalies (9). In another study, Shrivastava et al reviewed coronary angiograms of 296 cases with TOF, and reported 11.8% coronary artery anomalies (16). A similar study in Iranian population also reports 5.9% coronary artery anomalies among 135 patients (17). The incidence of coronary anomalies in TOF varies widely regarding the method of detection.
Postmortem studies demonstrate a higher incidence of 5 - 9 percent, which is probably due to greater possibility of careful examination of the coronary arteries (18), and the overestimation bias can occur due to increased surgical mortality rate related with coronary artery anomalies. Some older studies surprisingly reported a very higher rate of anomaly and even high rate of coronary fistula in TOF patients that are poorly consistent with other researchs (1, 2, 4, 15).
In agreement with the dominant reports, our study confirmed that the most common coronary anomaly was the origin of LAD from RCA which was seen in 20 cases (4.4%), and single origin coronary artery was the second most common anomaly. RCA origin from LAD or left main coronary artery had the lowest frequency in our population that was in agreement with other studies (4, 15, 17).
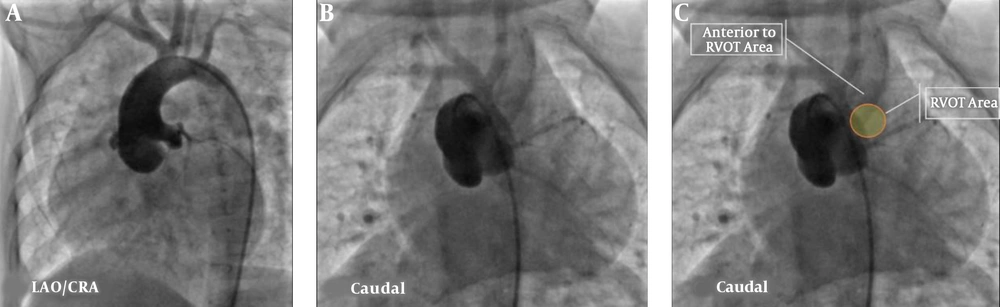
Sensitivity of an angiography report depends on the experience of operators, quality of images, and the most important factor, i.e., image views. In our study, the specificity of angiographies to detect coronary anomaly was high (99%), but the sensitivity was dependent on the angiographic views, which ranged from 75% for LAO/CRA view to 100% for LAO/CAU view. In this study, most abnormal coronary anatomy and courses were detected in the LAO/CAU view, and LAO/CRA view missed a significant portion of the coronary anomalies. Extreme caudal view (45°) had excellent sensitivity and specificity for detection of the anomalies in angiographic evaluation.
A few studies have compared coronary anomalies in the angiography with surgical reports and we could not find a sensitivity report for angiography in similar studies (19). Li et al. (8) studied a limited number of TOF patients and reported coronary artery anomaly in 14% of the cases, while two of them were misdiagnosed in the pre-operational caudal angiography view. One of their cases died due to transection of an undiagnosed coronary anomaly during repair. Compared to that study, we had more misdiagnosis in group 1 that can be related to the lesser usage of caudal view among this group, while we had not any misdiagnosed case among group 2. Carvalho et al. (10) also emphasized on caudal view and labeled it as an excellent view to detect coronary arteries that are passing the RVOT, and they asserted that the lateral view was also needed to differentiate the anterior or posterior position of the crossing artery in the laid-back view; it was indicated that this view may decrease some false positive cases in the caudal view. However, we have not any misunderstanding in the caudal view, and lateral view might not be necessary, so elimination of this view can reduce the X-ray radiation.
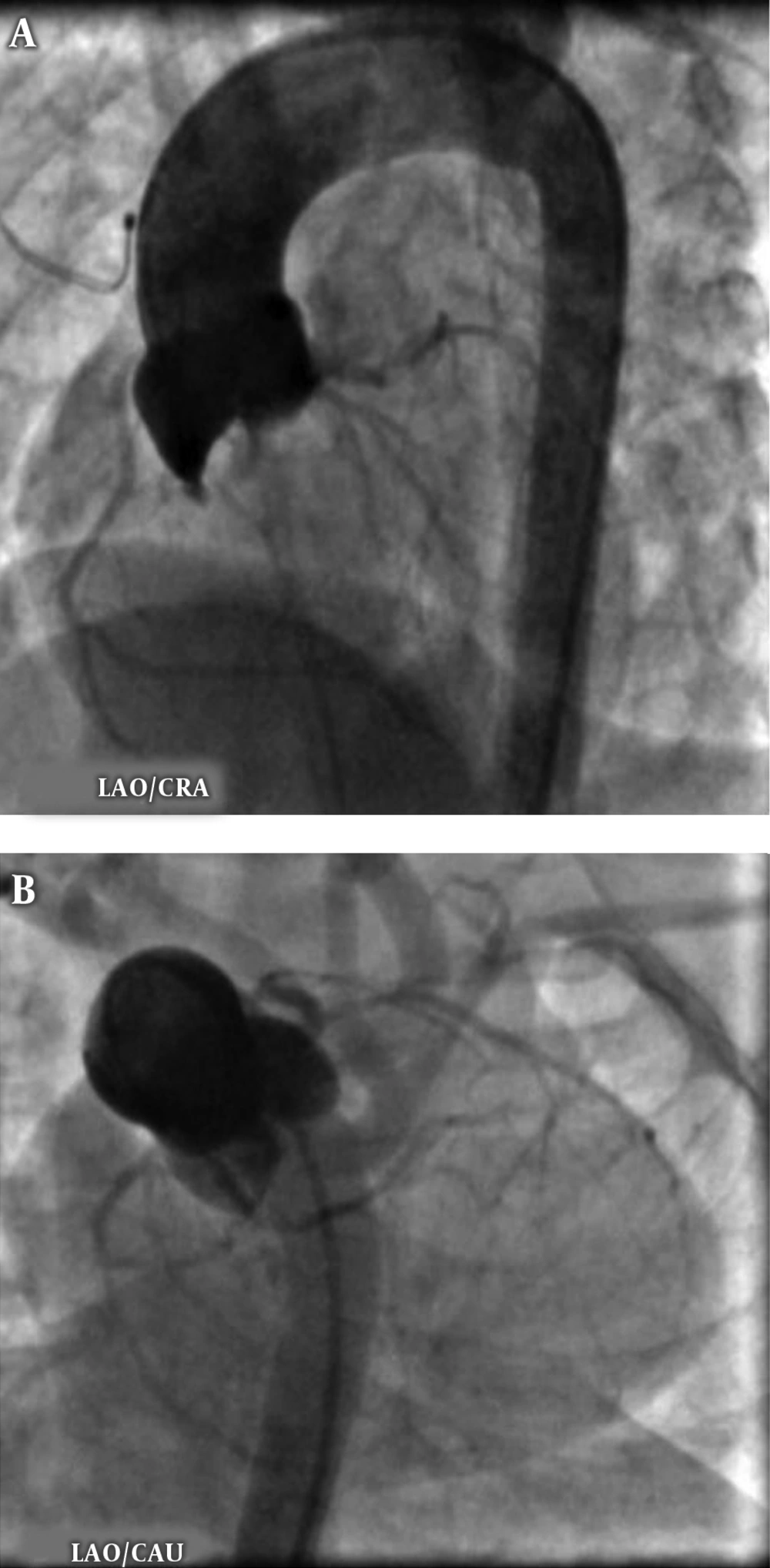
It seems that the key view in interpreting TOF coronary anatomy is caudal view. The Caudal view illustrated in Figures 1 and 2 from our patients clearly show an abnormal course of coronary arteries crossing RVOT, while none of them had a significant finding in the LAO/CRA view.
Cineangiograms of the 8 proven abnormal coronaries that were reviewed by an expert pediatric cardiologist also showed the weakness of LAO/CRA view to detect coronary artery anomaly with only 25% definite detection of abnormal coronary course passing across the RVOT. In the LAO/CRA view, interpretation of the anterior-posterior relationship of RVOT and LVOT is difficult and may lead to high rate of misdiagnosis of clinically significant abnormal coronary courses.
Compared to CT scan, our data showed excellent sensitivity for angiographic detection of coronary anomaly crossing RVOT if the caudal view is used, but clearly the LAO/CRA view had less sensitivity. New dual source CT scan can accurately explore coronary anatomy with no need to the heart rate modification even in infants, with no usual cardiac catheterization risk. In multiple studies, more than 95% sensitivity and specificity were reported to detect coronary artery anomalies that is excellent result with less radiation in comparison to angiography (2, 4, 15). This modality may replace cardiac catheterization in future.
5.1. Conclusions
In conclusion, performing LAO/CAU root angiography seems essential for evaluation of coronary anatomy in TOF patients, and lateral view might not be necessary if caudal is used. Also, LAO/CRA view for interpreting coronary anatomy course seems to lead to misdiagnosis in coronary artery branch anomalies that pass across the RVOT.