1. Background
Chest X-ray (CXR) is known as the most common radiography used for adult and pediatric patients worldwide since it is a simple, low-cost, and accessible imaging examination procedure that can show a wide range of diseases in the lung parenchyma, the pleural cavity, and the thoracic skeleton as well as some mediastinal disorders if it has enough quality (1, 2).
Factors affecting image quality include: proper exposure techniques, correct patient positioning, patient cooperation in maintaining his/her position, and accurate field collimation (3-5). However, neonatal and pediatric patients have different conditions for imaging. That is, they are restless during this procedure and are not often expected to be cooperative, which may lead to repetition of radiographs because of their poor quality (6).
Patient radiation dose is another important issue about pediatric CXR. Some researchers believe that radiation dose of this radiography is low and there is no point to worry about it (3, 7). Nevertheless, there are some significant points about neonatal and pediatric dose. First of all, infants are much higher sensitive to radiation so that cancer risk for a given dose is 10-15 times more than a person aged 50 years old. Secondly, patients may be examined several times all through their hospitalization (8, 9).
Chest radiography is commonly performed for different purposes in neonatal patients and it may repeat several times during the patient's hospitalization. This means that, such patients will receive several doses of radiographic examinations (10).
Exposure techniques, source-to-patient distance, use or non-use of grid, and imaging field size are factors affecting dose level in radiographic procedures (11). Several things can be done to reduce the patient's radiographic dose for chest radiography. First of all, radiographer must choose optimized exposure factors such as high KVP and low MAS as much as possible (12). Accurate and limited collimation is the second important factor in reducing the patient's radiation dose (13).
Moreover, optimizing exposure parameters in accordance with the safety principle of As Low As Reasonably Achievable (ALARA), appropriate patient positioning, patient immobilization are very helpful for patient dose reduction in pediatric CXR (13, 14).
X-ray field collimation has been also recognized as one of the most important factors influencing image quality and patient dose. According to the safety principle ALARA, radiographers have to limit radiation field to anatomical area of interest (15, 16).
For pediatric CXR, as described in Merrill’s Atlas of Radiographic Positioning & Procedures, X-ray field center should be coincided on T6-7 and field boundaries need to be extended from mastoid process to crest iliac (17). Evidence suggests that beam collimation with these dimensions leads to excessive dose to non-thoracic organs without having a particular clinical benefit (4, 7, 8). It seems, in supine position, when a child’s hands are upright, X-ray field can be collimated from acromioclavicular (AC) joint to lower costal margin (17, 18). In this way, the colons and the humeral shaft will receive less radiation. In any case, thyroid gland will be in the field and the only way to prevent radiation on this gland is to reduce the number of CXR requests (4).
Furthermore, use of tight collimation in digital and computer radiography can be so effective in maintaining image quality and lowering patient dose. Collimating X-ray field properly will also decrease the amount of irradiated tissues. This means, non-thoracic organs will not receive primary radiation and patient dose will be consequently moderated (4). On the other hand, scattered X-rays decrease as the X-ray field is limited and this prevents image fog and reduces contrast (5, 15).
2. Objectives
The main purpose of this study was to investigate X-ray field collimation quality and to assess extrathoracic structures located in radiation field in neonatal chest radiography. A CXR is known as the most common radiography for preterm infants hospitalized in neonatal intensive care units (NICUs) who may frequently undergo this examination in the course of their stay. For this reason, the present study focused on portable chest radiography of newborns and preterm infants admitted to NICUs.
3. Methods
This study was conducted on newborns and preterm infants admitted to NICUs of three hospitals. Hospital A was a maternity center and Hospitals B and C were general ones. The study samples included patients of both genders with different diseases and varying degrees of prematurity. To meet the study objectives, a total number of 213 radiographs - 71 patients in each hospital - related to newborns from three hospitals were evaluated in terms of X-ray field collimation and unnecessary irradiated organs in portable CXR in a retrospective study. In Hospital B, screen film radiography was used for portable neonatal chest radiographies and computer radiography was utilized in other two centers for this purpose.
In all groups, CXRs were performed through portable X-ray devices in NICUs. The given radiographs were also done by various groups of radiographers with different degrees of experience. For each radiograph, field collimation quality and unnecessary irradiated organs in X-ray field during imaging were studied. All these items were accomplished by a radiologist blind to patient data, based on a chart.
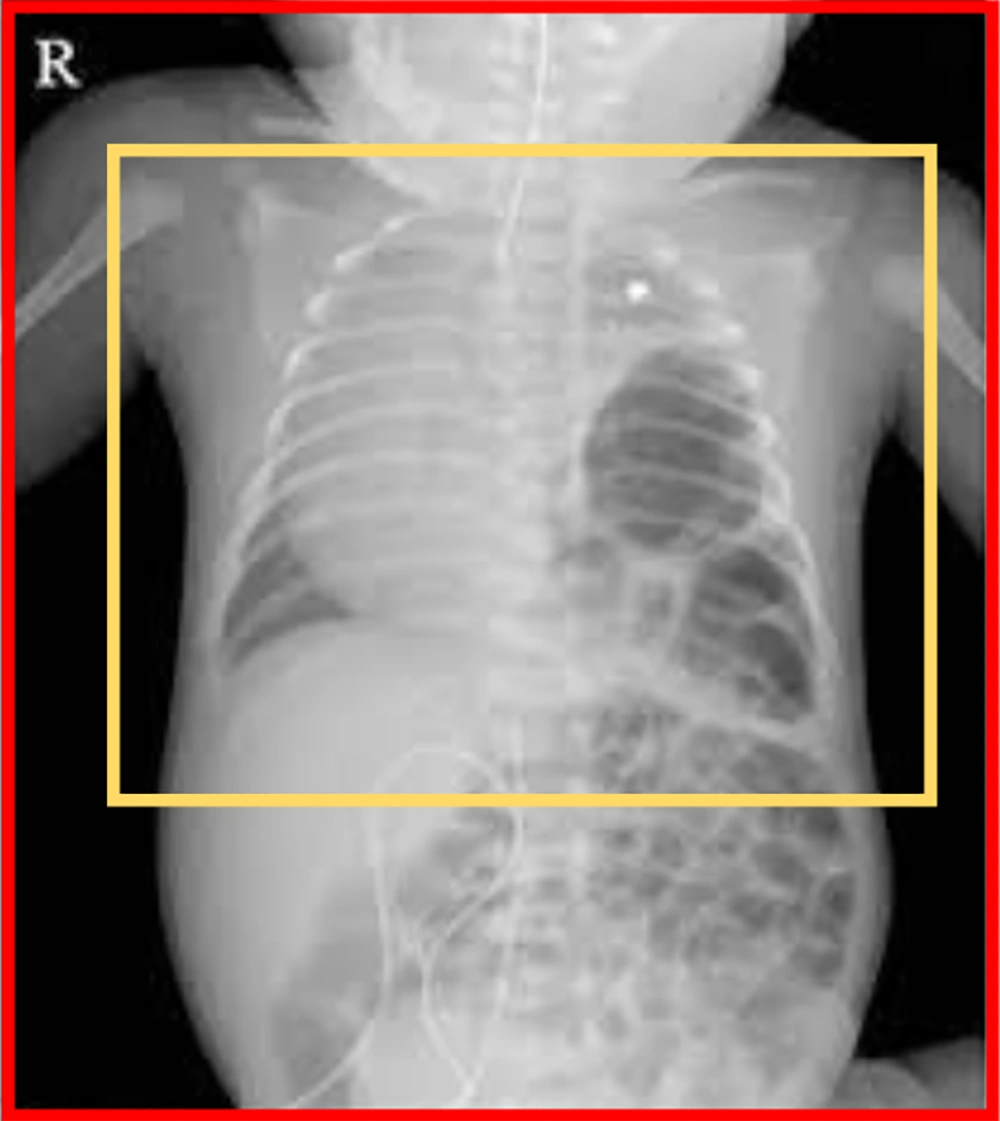
In this study, ideal imaging field (IIF) and current imaging field (CIF) were defined for collimation quality assessment. The margins of the IIF included acromioclavicular joint (AC) level to lower costal margin (top to bottom) and one centimeter beyond the broadest area of the chest on each side (that is, right to left). The CIF size was also defined as square borders of the collimators. The area of the CIF and the IIF along with their ratios was calculated for radiographs as follows:
Ratio factor (RF) = CIF/IIF
The IIF size and the CIF size are shown in Figure 1.
For digital radiographies (in Hospitals A and C), measurements were performed by a ruler available at the Picture Archiving and Communication System (PACS) workstation but a physical ruler was employed for analog graphy (in Hospital B). Based on clinical experience, neonatal and pediatric patients are restless during imaging and are not often expected to be cooperative. For this reason and with regard to limits of working with infants in medical imaging procedures, collimation quality was defined in three subcategories including “acceptable”, “weak” and “unacceptable” collimation, according to RF values and radiologist’s opinion.
The exposure of non-thoracic organs such as the humerus, the mandible, and parts of the abdomen to primary beam in X-ray field was also assessed in this study. The exposure of the humerus was analyzed in three subcategories of “no exposure to the humerus”, “part of the shaft”, and “entire length of the humerus”. It should be noted that insufficient collimation may cause irradiation on the mandible and the abdominal organs. Accordingly, the mandible irradiation was evaluated in two subcategories of “yes” and “no”, whether the mandible had been seen in radiography or not; respectively. Also, the abdomen irradiation was assessed in two subcategories of “yes” and “no”, if the radiation field had expanded far below the lower costal margins or not; respectively. The data were then analyzed using the IBM SPSS Statistics (Version 16) (SPSS Inc.).
4. Results
Collimation quality and extrathoracic organs located inside the radiation field were evaluated. For collimation quality assessments, the CIF and the IIF along with their ratios (i.e. RF) were also defined.
RF analysis is summarized in Table 1, suggesting that collimation quality in neonatal radiographs is not accurate and it has some defects, although there are differences in collimation quality in three hospitals.
| Hospital | Number | Minimum | Maximum | Mean | Standard Deviation (SD) |
|---|---|---|---|---|---|
| A | 71 | 1 | 2.8 | 1.65 | 0.46 |
| B | 71 | 1.15 | 2.6 | 1.54 | 0.21 |
| C | 71 | 1.17 | 2.71 | 1.76 | 0.42 |
| Total | 213 | 1 | 2.8 | 1.65 | 0.39 |
Unfortunately, the study cases had a radiation field of 1.65 ± 0.39 times to necessary field and this was sometimes as high as 2.8 times. In other words, these neonates had received an average of 1.65 ± 0.39 times more radiation from primary beams and this was sometimes as high as 2.8 times.
As mentioned, neonatal and pediatric patients are restless during imaging and are not often expected to be cooperative. For these limits of working with infants in the course of imaging and in order to have a more realistic picture of collimation quality, it was analyzed in three subcategories of “acceptable”, “weak”, and “unacceptable”, according to RF values and radiologist’s opinion. This evaluation is illustrated in Table 2.
| Hospital | Collimation | Collimation Quality | ||
|---|---|---|---|---|
| Acceptable | Weak | Unacceptable | ||
| A | Frequency | 26 | 23 | 22 |
| Within center, % | 36.6 | 32.4 | 31.0 | |
| B | Frequency | 21 | 45 | 5 |
| Within center, % | 29.6 | 63.4 | 7.0 | |
| C | Frequency | 14 | 31 | 26 |
| Within center, % | 19.7 | 43.7 | 36.6 | |
| Total | Frequency | 61 | 99 | 53 |
| Within center, % | 28.6 | 46.5 | 24.9 | |
Hospital A had the highest acceptable collimation and Hospital B had the lowest unacceptable collimation. It should be noted that Hospital A was a maternity center providing specialized services to neonates and children. In Hospital B, radiographers also used an immobilizer to fix patients’ body and limbs during imaging.
In this study, one-way analysis of variance (ANOVA) was utilized to compare RF mean values in different groups. Table 3 outlines these data.
Hospital B had the lowest RF (Table 1) and its mean difference was significant compared with Hospital C.
The exposure of non-thoracic organs in X-ray field such as the humerus, the mandible, and part of the abdomen were also evaluated in this study, as presented in Tables 3-5. Table 3 shows exposure of the humerus in CXR as “no exposure to the humerus (No)”, “part of the shaft”, and “entire length of the humerus” in three hospitals.
| Hospital | Presence of the Humerus | Humerus | ||
|---|---|---|---|---|
| No | Part of the Shaft | Entire Length of the Humerus | ||
| A | Frequency | 28 | 19 | 24 |
| Within center, % | 39.4 | 26.8 | 33.8 | |
| B | Frequency | 11 | 21 | 39 |
| Within center, % | 15.5 | 29.6 | 54.9 | |
| C | Frequency | 18 | 22 | 31 |
| Within center, % | 25.4 | 31.0 | 43.7 | |
| Total | Frequency | 57 | 62 | 94 |
| Within center, % | 26.8 | 29.1 | 44.1 | |
| Hospital | Presence of the Mandible | Mandible | |
|---|---|---|---|
| No | Yes | ||
| A | Frequency | 41 | 30 |
| Within center, % | 57.7 | 42.3 | |
| B | Frequency | 35 | 36 |
| Within center, % | 49.3 | 50.7 | |
| C | Frequency | 39 | 32 |
| Within center, % | 54.9 | 45.1 | |
| Total | Frequency | 115 | 98 |
| Within all patients, % | 54.0 | 46.0 | |
According to Table 3, Hospital A was more successful than two others in terms of radiation dose saving of the humerus.
Tables 5 and 6 represent the exposure of the mandible and part of the abdomen to X-ray field of chest radiographs; respectively. Evaluations also showed that the mandible and part of the abdomen had lower frequency of radiation exposure in Hospital A.
| Hospital | Presence of the Abdomen | Excess Parts of the Abdomen | |
|---|---|---|---|
| No | Yes | ||
| A | Frequency | 29 | 42 |
| Within center, % | 40.8 | 59.2 | |
| B | Frequency | 25 | 46 |
| Within center, % | 35.2 | 64.8 | |
| C | Frequency | 21 | 50 |
| Within center, % | 29.6 | 70.4 | |
| Total | Frequency | 64 | 149 |
| Within center, % | 30.0 | 70.0 | |
These results illustrated that improper collimation could lead to exposure of different organs to irradiation field, receiving excessive dose from primary beams.
5. Discussion
In this study, collimation quality was assessed for portable neonatal CXR in three hospitals. It should be noted that this procedure is the most common radiography performed for preterm infants and neonates hospitalized, so patients may be examined several times during their hospitalization (8, 13). In this study, Hospital A was a maternity center providing specialized services to neonates and children, but Hospitals B and C were general ones. In Hospital B, radiographers had used a body immobilizer to fix patient’s body and limbs during imaging.
The CIF and the IIF as well as their ratios (i.e. RF) were defined for radiographs to meet the objectives of collimation quality assessments: RF = CIF/IIF
RF calculation in this study showed that patients had a radiation field of 1.65 ± 0.39 times to IIF (Table 1) and this was sometimes as high as 2.8 times. In other words, the neonates had also received an average of 1.65 ± 0.39 times more radiation from primary beams and this was sometimes as high as 2.8 times. Moreover, insufficient collimation was seen in all hospitals with different intensities. This means that, extrathoracic organs had been irradiated unnecessarily with primary beams in routine neonatal CXRs, which could cause an elevation in patient dose (11). It seems that mandatory protective rules are required to compel radiographers to execute the safety principle of ALARA including optimum collimation.
Table 2 showed that Hospital A had the highest acceptable collimation in comparison with Hospitals B and C. This superiority might be due to several issues. First, Hospital A was a maternity center providing specialized services to neonates and children. For this reason, it seemed that radiographers in Hospital A had better skills and more experiences for neonatal and pediatric radiographies. Second, radiographies were only done for neonates and infants and neonate CXRs had been frequently performed every day.
According to Table 2, weak and unacceptable collimation (RF of 1.4-2.8) had the most proportion (71.4%), in three hospitals, so it could lead to irradiation on extrathoracic organs. It showed that mandatory actions are required.
Acceptable collimation in this study was higher than that in a similar survey by Karimi et al (28.6% vs 15.5%) (4), maybe due to different criteria considered for ideal collimation in two investigations.
Table 3 also showed that Hospital B had the lowest RF mean in this study, possibly due to patient immobilization technique. In Hospital B, radiographers had used a special body immobilizer to fix neonate’s body and limbs prior to exposure, implying that radiographers needed to become insured from patient’s positioning and easily focus on irradiation field collimation.
The mean difference value for RF in Table 4 demonstrated that difference between Hospitals B and C was significant. Both centers were general hospitals and their radiographers had a variety of skills and experiences. This difference may be due to the fact that patient’s body and limbs had become immobilized in Hospital B by special immobilizers while patient’s positions in Hospital C had been fixed by sand bags and assistance by patient’s companions.
Irradiation on the humerus due to primary beams in three centers is presented in Table 4. Only in 26.8% of neonatal CXRs, the humerus was out of fields. Hospital A also had the highest status in terms of humeral sparing by 39.4%.
Irradiation on the mandible was further analyzed in Table 5. In 46% of all chest radiographies in the present study, the mandible was in the field of radiation and Hospital A had the best status among other centers with 57.7% mandible sparing.
Excess parts of the abdomen may be irradiated in insufficient collimation field during neonatal and infant chest radiography. In this study, the excess parts of the abdomen had been located in the field of primary radiation in 70% of the radiographs.
Totally, the results showed that the X-ray field collimation had not been selected accurately and a range of non-thoracic organs had fallen into the radiation field. On the other hand, body bulk and internal organs in neonates are small and X-ray field increment may lead to serious irradiation on non-thoracic organs (15, 19). In weak and unacceptable collimations, non-thoracic organs were also located in the X-ray field. This means that, these organs will receive unnecessary primary radiation and patient radiation dose increases.
In this study, portable neonatal CXRs were implemented by radiographers with varying degrees of experience and knowledge. Undoubtedly, radiographers’ knowledge as well as their experience and skills in working with neonates could play important roles in collimation quality which was confirmed in the present study. Hospital A was a maternity center providing specialized services to infants and had the highest acceptable collimation (36.6%) compared with other hospitals; moreover, this center had the best score in non-thoracic organs sparing, so about 39.4%, 57.7%, 40.8% of the humerus, the mandible, and parts of the abdomen were spared; respectively.
Undoubtedly, experience and skill in infant radiography can have superiority in sparing extrathoracic organs. Also, radiographer’s adherence to ethical issues has a critical role in collimation quality. Utilizing auxiliary equipment for patient immobilization can also have a contributory role in proper X-ray field collimation. In the present study, RF mean difference was significant between Hospitals B and C (Table 3) as general centers. But, in Hospital B, radiographers had used immobilizers for patient’s body fixation during the procedure.
It should be noted that red bone marrow in the humerus is a critical target for ionizing radiations since it includes hematopoietic stem cells with high mitotic indices (20). So, humerus sparing through a tight collimation and proper positioning is of importance in terms of dosimetry and radiobiology.
Furthermore, the presence of the humerus or the mandible in imaging field can lead to image rendering by the system during post-processing procedure in computer and digital imaging (18, 21). As the head of the humerus or the mandible are depicted as extremely white, it can reduce the contrast of other areas of the image during rendering.
Moreover, use of wide collimation can result in patient dose increment if an unnecessary dense object such as the humerus or the mandible is located on ionization chamber of the automatic exposure control (AEC) system, if it is selected (21, 22).
5.1. Conclusion
Improper X-ray field collimation can induce excessive radiation dose to non-thoracic organs such as humerus, mandible, and parts of the abdomen in chest radiographs. In this regard, infants are much higher sensitive to radiation, so cancer risk for a given dose is much higher for such patients. Improper collimation may even affect image quality and AEC function. It seems that technical training and medical ethics education to radiographers along with use of patient immobilization devices are among important points, helping in proper collimation and radiation reduction on non-thoracic organs in CXRs. Furthermore, mandatory protective rules are required to compel radiographers to execute the safety principle of ALARA including optimum collimation.